Publication
State-level Flu Vaccination Rates Among Key Population Subgroups (50-state profiles)
As the nation and individual states prepare to ramp up COVID-19 vaccination rollout campaigns beyond the initial phase of prioritized recipients, understanding the challenges they face in getting vaccines to key resident demographics is important to their success in achieving population-level coronavirus immunity—also commonly known as “herd immunity.”
While states and federal organizations are slowly beginning to collect and disseminate what data they’ve been able to collect regarding COVID vaccination thus far, it is still limited. Adult flu vaccine data, however, can be used as the best available proxy in the meantime for understanding vaccination patterns across states and the nation on a larger scale.
This set of two-page infographics explores state-level estimates on flu vaccination rates for adults (age 18+) using data for all 50 states and the District of Columbia (D.C.) from the Behavioral Risk Factor Surveillance System (BRFSS) survey.
The infographics provide comparisons for individual state flu vaccine rates to the minimum COVID-19 herd immunity target (70%). Each individual state infographic also highlights vaccination rates for individual states as compared to a number of demographic categories, including age, race/ethnicity, household income level, insurance status, chronic conditions, access to care, and educational attainment.
Click on a state below to see its two-page infographic. Click here to access the District of Columbia infographic. Click here to access the United States infographic.
|
State Health Compare Flu Vaccination Data Click here to explore the flu vaccination measure further on State Health Compare |
Further Reading and Resources
Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns
SHADAC Brief, January 2021
New Brief Examines Flu Vaccine Patterns as a Proxy for COVID – Anticipating and Addressing Coronavirus Vaccination Campaign Challenges at the National and State Level
SHADAC Blog, January 2021
COVID-19 Vaccine Challenges: Illustrating Hurdles to Population Immunity and Equity Using Flu Vaccination Data
SHADAC Webinar, February 2021
Ensuring Equity: State Strategies for Monitoring COVID-19 Vaccination Rates by Race and Other Priority Populations
SHVS Expert Perspective, February 2021
Blog & News
50-State Infographics: A State-level Look at Flu Vaccination Rates among Key Population Subgroups
Feb 18, 2021: The rapid development and approval of COVID-19 vaccines less than a year after the pandemic reached the United States has offered hope to end the crisis. But there are still great challenges to effectively and equitably distributing the vaccinations throughout the population.
The rapid development and approval of COVID-19 vaccines less than a year after the pandemic reached the United States has offered hope to end the crisis. But there are still great challenges to effectively and equitably distributing the vaccinations throughout the population.
As states roll out the vaccines to the first phases of recipients, planning is already underway for subsequent phases of vaccination for the broader public. However, these plans will need to adapt to operation on a much larger scale in order to reach experts’ recommended vaccination thresholds of 70-90% in order to achieve “herd immunity,” as well as respond to Dr. Anthony Fauci’s recent declaration of a vaccine “open season” by April—that essentially any member of the general public who wants a vaccine will be able to get one.
To aid states in developing campaigns to achieve these ambitious targets, SHADAC researchers have recently published a number of resources—including an issue brief funded by the California Health Care Foundation—looking to the nation’s previous experiences with implementing another mass vaccination campaign: influenza. By using past flu vaccination rates as a proxy for understanding challenges to widespread vaccination, states can plan for challenges in coronavirus vaccination.
Adding to this group of resources, SHADAC has produced a set of two-page infographics focused on flu vaccination rates for adults (age 18+) using data for all 50 states and the District of Columbia (D.C.) from the Behavioral Risk Factor Surveillance System (BRFSS) survey. The infographics provide comparisons for individual state flu vaccine rates to a COVID-19 herd immunity target and also highlight vaccination rates for individual states as compared to by a number of demographic categories, including age, race/ethnicity, household income level, insurance status, chronic conditions, access to care, and educational attainment.
| HIGHLIGHTS |
National COVID-19 vaccination hurdles
COVID-19 vaccination campaigns face a number of stumbling blocks to effective implementation, including general and specific groups’ vaccine hesitancy, the potential for overpromising and under-delivering on vaccine distribution, a lack of available vaccine doses, for example.
However, as flu vaccination data demonstrate, much work must be done to address issues of vaccine distribution in order to achieve population-level immunization from the novel coronavirus. Only 38.7 percent of U.S. adults reported getting a flu shot during the survey years of 2017-2019—barely more than half the minimum anticipated 70 percent target for herd immunity.
Data from various segments of the national population also show low adult vaccination rates across specific demographic groups. For instance, vaccination rates were significantly lower than the national average for American Indian and Alaska Natives (33.9 percent), Black adults (32.8 percent), and Latino people (30.9 percent).
Younger adults (age 18-39) were also significantly less likely to receive a flu vaccine, at 28.5 percent, as were adults with incomes below $25,000 (34.8 percent), those who reported having no personal doctor (20.1 percent), and people without health insurance, reporting the lowest rate at just 17.6 percent.
State variation in flu vaccination rates
While the Biden administration has signaled plans to take an active role in the distribution and administration of the COVID-19 vaccines, responsibility for the rollout has still largely been borne by the states. It is therefore important that each individual state understands the specific needs of not only their residents broadly, but also by subpopulations, some of whom are more likely than others to require targeted outreach efforts in a vaccination campaign strategy.
Examining adult flu vaccinations across the states shows wide variation in rates. Eighteen states had vaccination rates significantly below the U.S. average, with Nevada having the lowest at 32.7 percent; just seven did not differ significantly from the U.S. rate; and 27 states and the District of Columbia (D.C.) had vaccination rates significantly higher than the U.S.
While the fact that over half of states are above the national average in flu vaccination is a good initial sign, even the highest individual state rate of 45.4 percent in North Carolina unfortunately falls far short of the minimum goal of 70% vaccination for COVID-19 herd immunity. This discrepancy between actual rates of vaccination and goals for coronavirus vaccination campaigns underscores the need to not only examine rates at state levels, but to further break down data to understand the specific needs of states’ populations by demographic subgroups.
For instance, continuing to look at North Carolina, with the highest state vaccination rate, and Nevada, with the lowest, both states face similar barriers in overcoming low vaccination rates among individuals without health insurance coverage (21.8 percent and 14.4 percent, respectively; less than half the rates among those with insurance) and those without a personal doctor (23.8 percent and 17.5 percent; again less than half of flu vaccination rates among adults who report having a personal doctor). However, when analyzing vaccination rates by race and ethnicity, American Indian and Alaska Natives and those reporting “Other/multiple” race in North Carolina each had vaccination rates significantly lower than the overall state rate (33.7 percent and 36.0 percent, respectively), while the same groups in Nevada reported rates of vaccinations higher than the overall adult population (39.3 percent for American Indian and Alaska Natives and 34.7 percent for “Other/multiple” races).
Conclusions
While state and federal organizations continue to build and ramp up data collection on COVID-19 vaccines, looking to flu vaccination rates in the meantime can provide important guidance for understanding the challenges faced in mounting large scale COVID vaccination campaigns, especially in focusing targeted outreach efforts on population subgroups that need it most.
These two-page infographics provide important and detailed information on vaccination rates not only by state, but by demographic categories, as well as how their rates differ from state and national averages for the most recent data years available, 2017-2019.
|
State Health Compare Flu Vaccination Data Click here to explore the flu vaccination measure further on State Health Compare |
Further Reading and Resources
Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns
SHADAC Brief, January 2021
New Brief Examines Flu Vaccine Patterns as a Proxy for COVID – Anticipating and Addressing Coronavirus Vaccination Campaign Challenges at the National and State Level
SHADAC Blog, January 2021
COVID-19 Vaccine Challenges: Illustrating Hurdles to Population Immunity and Equity Using Flu Vaccination Data
SHADAC Webinar, February 2021
Ensuring Equity: State Strategies for Monitoring COVID-19 Vaccination Rates by Race and Other Priority Populations
SHVS Expert Perspective, February 2021
Blog & News
NHIS: Early Release Estimates Show Unchanged Coverage Rates during First Half of 2020, although NCHS Reports Evidence of Nonresponse Bias due to COVID-19
February 15, 2021:The National Center for Health Statistics (NCHS) has just published health insurance coverage estimates for the first half of 2020 (January to June) from the National Health Interview Survey (NHIS) as part of the NHIS Early Release Program. These estimates are some of the first available coverage estimates for 2020 from a federal survey and among the first estimates to cover the beginning of the coronavirus (COVID-19) pandemic in the United States.
Topline Estimates from January-June 2020
At a high level, the new estimates show no significant changes in coverage type or uninsured rate when compared to the same period of time in 2019. Among nonelderly adults (ages 18 to 64) surveyed between January and June 2020, 13.4% were uninsured at the time of interview, 20.8% had public coverage, and 67.9% had private coverage. These rates were 14.7%, 20.4%, and 66.8%, respectively, from January to June 2019.
Nonresponse Bias Report for April-June, 2020 (Q2)
NCHS released a report to accompany the January-June 2020 estimates that presents a preliminary analysis of a drop in response rates in Q2 2020 (April-June).
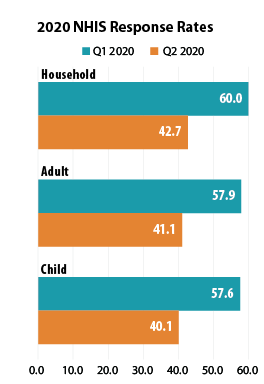 NHIS data collection, which is typically conducted by making personal visits to respondents’ homes, was significantly impacted by the COVID-19 pandemic beginning in Q2 2020: Personal visits were suspended beginning on March 19, 2020, and data was collected by telephone instead. As a result of the shift to telephone-only interviewing, the sample household response rate declined from 60.0% in Q1 (January-March) to 42.7% in Q2; the adult response rate fell from 57.9% to 41.1%; and the child response rate dropped from 57.6% to 40.1%.
NHIS data collection, which is typically conducted by making personal visits to respondents’ homes, was significantly impacted by the COVID-19 pandemic beginning in Q2 2020: Personal visits were suspended beginning on March 19, 2020, and data was collected by telephone instead. As a result of the shift to telephone-only interviewing, the sample household response rate declined from 60.0% in Q1 (January-March) to 42.7% in Q2; the adult response rate fell from 57.9% to 41.1%; and the child response rate dropped from 57.6% to 40.1%.
NCHS researchers compared the characteristics of Q2 respondents to the characteristics of respondents from Q1 to determine whether the smaller Q2 sample was systematically biased in any way and found that lower-income and renter households were underrepresented in the Q2 sample. This points to potential nonresponse bias and to the possibility that the actual uninsured rates for Q2 2020 were higher than the NHIS early release estimates indicate, as lower-income and renter households tend to have higher rates of uninsurance than do middle- and higher-income households and home-owning households.
SHADAC will continue to monitor all subsequent early data releases for 2020 from the NHIS survey, and will provide updates on any new methodology reports such as the investigation into nonresponse bias for Q2 2020 provided by NCHS.
Notes about the Estimates
The above estimates provide a point-in-time measure of health insurance coverage, indicating the percent of persons with that type of coverage at the time of the interview.
All changes described compare January-June 2020 to January-June 2019, and are statistically significant at the 95% confidence level unless otherwise specified.
Citations
Cohen, R.A., Terlizzi, E.P., Cha, A.E., & Martinez, M.E. (2021). Health insurance coverage: Early release of estimates from the National Health Interview Survey, January–June 2020. National Center for Health Statistics (NCHS). https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur202102-508.pdf
Dahlhamer, J.M., Bramlett, M.D., Maitland, A., & Blumberg, S.J. Preliminary evaluation of nonresponse bias due to the COVID-19 pandemic on National Health Interview Survey estimates, April-June 2020. National Center for Health Statistics (NCHS). https://www.cdc.gov/nchs/data/nhis/earlyrelease/nonresponse202102-508.pdf?ACSTrackingID=USCDC_374-DM49266&ACSTrackingLabel=NHIS%20Early%20Release%3A%20Non-response%20Bias&deliveryName=USCDC_374-DM49266
Blog & News
COVID-19 Vaccination Rates: State-level and Subpopulation Evidence from the Household Pulse Survey (Update: Jan 20 to Feb 1)
February 11th, 2021:Newly available COVID-19 vaccines promise to help protect individual Americans against infection and eventually provide population-level herd immunity. However, while the pace of COVID-19 vaccinations has picked up somewhat in recent weeks, the overall rollout thus far has remained somewhat slow and inconsistent. The initial groups prioritized for vaccination were health care workers on the front lines of the pandemic and nursing facility residents, many of whom are especially vulnerable to COVID-19 infection and severe outcomes.
While these groups continue to hold priority in vaccination slots, in response to reports of vaccines lingering unused and criticism from the public that limitations on vaccinations have too far slowed progress toward herd immunity many states have also recently begun expanding vaccine access to other (still high-priority) segments of the general population such as older adults, K-12 and child care workers, and those with high-risk medical conditions. However, there are concerns that these prioritization decisions and the existing mechanisms of the vaccine rollout—in addition to evidence that lower-income individuals, people of color, and individuals without strong connections to the health care system are less likely to get vaccinated—could worsen existing pandemic-related health inequities.
The available data have not assuaged these concerns, and show patterns of lower vaccination rates among people with lower incomes and levels of education, and marginalized racial and ethnic groups. The U.S. Census Bureau recently released updated data on take-up of COVID-19 vaccines from the most recent wave of its Household Pulse Survey (HPS), collected January 20-February 1, 2021.1 The HPS is an ongoing, weekly tracking survey designed to measure impacts of the COVID-19 pandemic. These data provide an updated snapshot of COVID-19 vaccination rates and are the only data source to do so at the state level by subpopulation. This blog post presents top-level findings from these new data, focusing on rates of vaccination (one or more doses) among U.S. adults (age 18 and older) living in households and comparing to results from the previous wave of the HPS, collected January 6-18.2
Roughly 13 percent of adults received a vaccination, but this varied by state
According to the new HPS data, 13.2% of U.S. adults had received one or more COVID-19 vaccinations during this two week period in January through February, though this varied by state from a low of 8.6% in Alabama to a high of 23.2% in Hawaii and Alaska. More than one in six adults had received a vaccine in eight states: Alaska, Hawaii, Indiana, Mississippi, New Mexico, Oklahoma, South Dakota, and West Virginia.
Vaccination rates increased substantially across nearly all states
Nationally, adult vaccination rates were up from the previous wave of the HPS, increasing from 7.7% in January 6-18 to 13.2% in January 20-February 1. Most states also experienced increases in their vaccination rates, though again the size of these increases varied across the states, from an increase of just 0.5 percentage points (PP) in Montana to an increase of 10.5 PP in Mississippi. Vaccination rates more than doubled in eight states: California, Florida, Indiana, Mississippi, Nevada, New York, South Carolina, and West Virginia.
Percent of Adults Who Had Received a COVID-19 Vaccine

Disparities in vaccination rates remain, though some have narrowed
COVID vaccination rates continued to vary to a great degree by demographic and socioeconomic factors, though disparities narrowed slightly from previous weeks.
This narrowing could be due to the expansion of priority groups to include a broader share of the population over this period; however, progress has remained limited in getting vaccines to certain groups such as low-income and Hispanic adults, for instance, and new vaccination strategies may be needed to reach the hardest-to-reach groups such as these.
By race and ethnicity, non-Hispanic Asian and non-Hispanic White adults continued to have above-average vaccination rates at 19.5% and 14.0%, respectively. Vaccination rates among non-Hispanic adults identifying with multiple races or “some other” race increased relative to the average, rising to 13.1%, nearly in line with the national average of 13.2%. Rates among non-Hispanic Black adults (11.0%) and Hispanic/Latino adults of any race (9.4%) remained below the national average.
Percent of Adults Who Had Received a COVID-19 Vaccine by Race/Ethnicity

Disparities in vaccination rates by income narrowed somewhat, though those with the highest incomes continued to be much more likely to have received a vaccine compared with those with lower levels of income. Of adults with incomes of $100,000 or more, 18.0% had received a vaccination compared to just 6.6% of those with incomes less than $25,000. This pattern was broadly consistent across the states, and in nearly all states, adults with incomes of $100,000 or greater were more likely to have received a vaccine than the state overall.
Percent of Adults who Received a COVID-19 Vaccine by Income

Disparities by level of education did not appreciably narrow, with adults holding a bachelor’s degree or higher having the highest vaccination rate at 20.2% and adults without a high school diploma having the lowest vaccination rates at 6.2%. These rates remained stable in relation to the national average compared with earlier in the month, and similar disparities were common across nearly all states.
At least 1 in 5 older adults received a COVID vaccine as the U.S. and many states made large progress in vaccinating older adults
Nationally, 20.4% of older adults (age 65 and older) had received at least one dose of the COVID-19 vaccine, which was more than seven percentage-points higher than among all adults (13.2%). Vaccination rates for older adults range from 8.5% in Minnesota to 56.0% in Alaska. Older adult vaccination rates were below 10% in three states (Kansas, Nebraska, and Minnesota) and above 30% in nine states (Alaska, Colorado, Florida, Georgia, Indiana, Louisiana, Mississippi, North Carolina, and Oklahoma) and the District of Columbia (D.C.).
The U.S. and nearly all states made large progress in vaccinating older adults compared with earlier in the month when older adults were no more likely to have received a vaccine than adults overall. This change was likely a reflection of many states’ recent expansion of vaccine prioritization for the general older-adult population and is heartening, considering that older adults are more likely to develop severe COVID-19 cases or die from the disease as compared to the general population.
Most states saw large increases in rates of vaccination among older adults, though from a relatively low baseline. Compared to earlier in January, 43 states and D.C. more than doubled their 65+ vaccination rates, with 26 of those at least tripling their rates. Only Minnesota failed to make substantial progress, increasing its older-adult vaccination rate to just 8.5% from 8.2% earlier in January, an increase of less than a percentage point.
Percent of Adults Age 65+ Who Had Received a COVID-19 Vaccine

Notes about the Household Pulse Survey Data
The estimated rates presented in this post were calculated from the count estimates published by the Census Bureau. Though these counts are accompanied by standard errors, standard errors are not able to be accurately calculated for rate estimates. Therefore, we are not able to determine if the differences we found in our analysis are statistically significant or if the estimates themselves are statistically reliable. Estimates and differences should be assumed to have large confidence intervals around them—especially for subpopulations at the state level—and caution should be taken when drawing strong conclusions from this analysis. However, the fact that patterns of inequities in other vaccination rates are mirrored by these early indications of COVID-19 vaccination inequities demonstrates reason for concern.
Though produced by the U.S. Census Bureau, the HPS is considered an “experimental” survey and does not necessarily meet the Census’s high standards for data quality and statistical reliability. For example, the survey has relatively low response rates (7.5% for January 20-February 1), and sampled individuals are contacted via email and text message, asking them to complete an internet-based survey. These issues in particular could be potential sources of bias but come with the tradeoffs of increased speed and flexibility in data collection as well as lower costs. A future post will investigate differences between COVID vaccination rates estimated from survey data (such as the HPS) and administrative sources. The estimates presented in this post are based on responses from 80,567 adults. More information about the data and methods for the Household Pulse Survey can be found in a previous SHADAC blog post.
Related Reading
COVID-19 Vaccination Rates: New State-level and Subpopulation Evidence from the Household Pulse Survey (Jan 6 to Jan 18) (SHADAC Blog)
Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns (SHADAC Brief)
New Brief Examines Flu Vaccine Patterns as a Proxy for COVID – Anticipating and Addressing Coronavirus Vaccination Campaign Challenges at the National and State Level (SHADAC Blog)
Ensuring Equity: State Strategies for Monitoring COVID-19 Vaccination Rates by Race and Other Priority Populations (Expert Perspective for State Health & Value Strategies)
SHADAC Webinar - Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns (February 4th) (SHADAC Webinar)
Blog & News
Eight Updated Measures are Now Available on SHADAC’s State Health Compare
February 2nd, 2021:Estimates for a number of measures from several categories (Cost of Care, Health Behaviors, Health Outcomes, Public Health, Quality of Care, and Social and Economic Factors) have recently been updated on SHADAC’s State Health Compare web tool. Data for each of these measures is drawn from a variety of differing surveys.

Child Vaccinations
 Child Vaccinations measures the rate of receipt of recommended vaccinations for children, which is defined as getting the recommended doses of the 7-vaccine series.1 SHADAC has updated the measure parameters to align with the National Immunization Survey’s new method of reporting by birth year, rather than survey year, and has also altered the measure definition to be the “percent of children age 24 months who had received all recommended vaccines,” changed from the “percent of children age 19-35 months who had received all recommended vaccines,” in order to more closely align with the Center for Disease Control and Prevention’s (CDC) child and adolescent recommended vaccination schedule. Data for all states is available on State Health Compare for birth years 2011-2016.
Child Vaccinations measures the rate of receipt of recommended vaccinations for children, which is defined as getting the recommended doses of the 7-vaccine series.1 SHADAC has updated the measure parameters to align with the National Immunization Survey’s new method of reporting by birth year, rather than survey year, and has also altered the measure definition to be the “percent of children age 24 months who had received all recommended vaccines,” changed from the “percent of children age 19-35 months who had received all recommended vaccines,” in order to more closely align with the Center for Disease Control and Prevention’s (CDC) child and adolescent recommended vaccination schedule. Data for all states is available on State Health Compare for birth years 2011-2016.
Children Considered to be Poor
Estimates for this measure capture the percent of children considered to be poor or those whose family income is less than 100% of the Federal Poverty Guidelines (FPG), which set the minimum amount of total income that a family needs for food, clothing, transportation, shelter and other necessities. Estimates are now available for all states for data years 2008-2019 and can be broken down by race and ethnicity.
Broadband Internet Access
This measure provides the percent of non-group quarters households that pay a cell phone or internet service provider for a broadband internet subscription (that includes a cellular data plan, cable, fiber optic, DSL, or satellite internet service). Data are available for 2016-2019 for all states and can be broken down by disability status, family income, Medicaid enrollment, and metropolitan status.
Unaffordable Rents
Data on unaffordable rents, which measures the percentage of rental households that spend more than 30% of their households’ monthly income on rent, is now available for 2012-2019. Breakdowns by disability status, household income categories, Medicaid enrollment, metropolitan status, and White/non-White racial categories are also available for all states.
Medicaid Expenses as Percent of State Budget
This is a measure of state and federal spending on Medicaid as a share of state budgets in a year, which is defined as the fiscal year. Estimates are available for fiscal years 2000-2019 in all states.
Suicide Deaths
Estimates for this measure provide age-adjusted rates of suicide deaths per 100,000 people. Rates can be broken down into categories of age, metropolitan status, race/ethnicity, sex, and method (firearm/non-firearm), and are available from 1999-2019 for all states.
Opioid-Related and Other Drug Poisoning Deaths
This measure provides the age-adjusted rates of deaths caused by drug poisoning (overdose), including those caused by natural and semi-synthetic opioids (e.g., common prescription painkiller pills such as hydrocodone and oxycodone), synthetic opioids (such as fentanyl, but excluding methadone), and the illegal opioid heroin. Also included are drugs that are often related to opioid deaths, such as cocaine and psychostimulants. Users are able to view estimates from 1999-2019, and can view rates for all states by individual drug types, as well as by groups (all opioids vs. all drugs).
Smoke-Free Campuses
Data for this measure indicate a simple “yes” or “no” answer to the question of whether a state has enacted laws to ensure smoke-free campuses at both the K-12 and collegiate levels. Estimates are now available for years 2000-2019 across all states, and can be broken down by campus types (e.g., public and private K-12 schools, public and private colleges, and all campuses).
Notes.
Data for the child vaccinations measure comes from the National Immunization Survey (NIS). Estimates for children considered to be poor, broadband internet access, and unaffordable rents come from the American Community Survey (ACS). The measure of Medicaid expenses as a percentage of a state’s budget comes from the National Association of State Budget Officers (NASBO) State Expenditure Reports. Rates of suicide deaths and opioid-related and other drug poisoning deaths are drawn from the National Center for Health Statistics (NCHS) Vital Statistics Data via the Centers for Disease Control and Prevention’s (CDC) WONDER database. Data for the smoke-free campuses are drawn from the CDC State Tobacco Activities Tracking and Evaluation (STATE) System.
Click here to explore these updated estimates on State Health Compare!
1 The 7-vaccine series consists of: 4 or more doses of either the diphtheria, tetanus toxoids, and pertussis vaccine (DTP), the diphtheria and tetanus toxoids vaccine (DT), or the diphtheria, tetanus toxoids, and acellular pertussis vaccine (DTaP); 3 or more doses of any poliovirus vaccine; 1 or more doses of a measles-containing vaccine (MCV); 3 or more doses or 4 or more doses of Haemophilus influenzae type b vaccine (Hib) depending on Hib vaccine product type (full series Hib); 3 or more doses of hepatitis B vaccine; 1 or more doses of varicella vaccine; and 4 or more doses of pneumococcal conjugate vaccine (PCV).










