Blog & News
Drug overdose deaths grew by almost 30 percent in 2020
July 15, 2021:Fentanyl- and methamphetamine-type drugs surged roughly 50 percent in 2020
Drug overdose deaths surged in the United States during the first year of the COVID-19 pandemic, increasing nearly 30 percent in just 12 months. Provisional data recently published by the U.S. Centers for Disease Control and Prevention (CDC) show that more than 92,000 people died of drug overdoses in 2020—surpassing records yet again.1
The growth was widespread throughout the country, with only two states (New Hampshire and South Dakota) spared from the jump in drug overdose deaths. Conversely, some states saw their death rates increase more than 50 percent, including Kentucky, South Carolina, Vermont, and West Virginia.
Much of the growth in drug overdose deaths was driven by synthetic opioids such as fentanyl, which increased more than 50 percent from 2019 to 2020 (see Figure 1). Fentanyl has become a key product for international drug traffickers, often finding its way as an adulterant in other drugs like heroin and cocaine, and even as an ingredient in counterfeits of common opioid prescription pills such as Oxycontin. The emergence of fentanyl in the U.S. illicit drug trade is a newer phenomenon beginning in the past decade, and it has recently spread from eastern states to increasingly affect states in the western half of the country as well.
Figure 1. Changes in drug overdose deaths in the U.S., 2019 to 2020

A family of drugs called “psychostimulants”—mostly methamphetamine—also drove a large increase in deaths in 2020, up nearly 50 percent since 2019. Deaths involving methamphetamine and other psychostimulants have grown dramatically in the past few years. The increased death toll involving psychostimulants is likely caused by two factors: First, the methamphetamine trafficked in the U.S. today is generally much more potent than methamphetamine sold in the past, raising the potential risk of overdoses caused by methamphetamine. Second, methamphetamine today is often contaminated with, or used alongside, synthetic opioids, raising the risk of an overdose involving the use of multiple drugs simultaneously.
Of the main drugs involved in overdoses2, only heroin was associated with a decline in deaths during 2020—falling by less than 10 percent since 2019. Meanwhile, overdose deaths involving prescription opioids increased more than 20 percent, reversing a trend of relatively stable or even declining death rates over several years. Cocaine overdose deaths similarly increased by more than 20 percent in 2020.
1 National Center for Health Statistics (NCHS). (2021, July 14). Vital Statistics Rapid Release: Provisional Drug Overdose Death Counts [Data set]. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
2 The drug overdose death categories presented in the CDC data include: heroin, natural opioid analgesics (e.g., morphine and codeine) and semisynthetic opioids (e.g., oxycodone and hydrocodone), synthetic opioids such as methadone and synthetic opioids other than methadone (e.g., fentanyl and tramadol), cocaine, and psychostimulants.
Blog & News
Pandemic drinking may exacerbate upward-trending alcohol deaths
June 14, 2021:Even before 2020, alcohol-involved deaths reached a modern record
Considering the well-deserved attention paid to the opioid crisis in recent years, few people might guess that rates of alcohol-involved deaths were as high as or higher than opioid overdose death rates in nearly half of states (Figure 1).1 Like the opioid crisis, the trend in alcohol-involved deaths is also worsening, having grown by roughly 50 percent in just over a decade. All this was before the coronavirus crisis had even begun.
Figure 1. State alcohol death rates vs. opioid death rates, 2019

|
Data and analysis on alcohol-involved deaths Read more about growing alcohol-involved death |
Now, evidence is accumulating that the pandemic precipitated dangerous changes in the way people consume alcohol in the United States. For instance, research has found increased alcohol sales since the crisis began, a finding illustrated by data showing that liquor taxes represented a rare instance of increased revenues for some states, such as Minnesota, during the COVID pandemic.2,3 Other studies have found that U.S. adults report consuming more alcohol in order to deal with pandemic-related stress, and that they are drinking more frequently and engaging in more high-risk drinking behaviors, such as heavy drinking and binge drinking.4,5,6
As we climb our way out of the immediate crisis, the U.S. will need to shift attention back to long-running public health threats. Beyond the obvious toll of the virus itself, another legacy of the pandemic may be the exacerbation of existing problems, including alcohol-related deaths and the opioid crisis. The opioid crisis was commonly recognized before 2020, but the upward trend in alcohol deaths was still occurring largely under the radar (Figure 2). But recent attention to risky pandemic-related alcohol consumption can sharpen our focus on this emerging concern.
Figure 2. U.S. alcohol-involved death rates, 2000-2019

With alcohol especially, the U.S. has a window of opportunity to intervene before many people’s pandemic-era risky drinking habits result in deaths, since the bulk of alcohol-involved deaths result from years of excessive drinking. In the coming years, it will be vital for states to monitor and study these issues and to consider doubling down on policy initiatives to curb the tide through efforts such as enhancing access to treatment of substance use disorder and by persuading and assisting people in recalibrating their alcohol consumption to healthier levels.
Visit State Health Compare to explore state-level data on alcohol death and opioid death rates.
1 SHADAC Staff. U.S. alcohol-related deaths grew nearly 50% in two decades: SHADAC briefs examine the number among subgroups and states. https://www.shadac.org/news/us-alcohol-related-deaths-grew-nearly-50-two-decades. Published April 19, 2021. Accessed May 12, 2021.
2 Rebalancing the ‘COVID-19 effect’ on alcohol sales. Nielseniq.com. https://nielseniq.com/global/en/insights/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/. Published May 7, 2020. Accessed May 12, 2021.
3 Ewoldt J. Liquor stores neared sales records for 2020 as bars, restaurants closed. Startribune.com. https://www.startribune.com/liquor-stores-neared-sales-records-for-2020-as-bars-restaurants-closed/573469221/. Published December 26, 2020. Accessed May, 12, 2021.
4 American Psychological Association. Stress in America: One year later, a new wave of pandemic health concerns. https://www.apa.org/news/press/releases/stress/2021/sia-pandemic-report.pdf. Published March 2021. Accessed May 12, 2021.
5 Pollard MS, Tucker JS, Green HD. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020; 3(9): e2022942. doi: 10.1001/jamanetworkopen.2020.22942.
6 Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health. 2020;17(24): 9189. doi: 10.3390/ijerph17249189
Blog & News
5 States and DC Led the Pack for Per-Capita State Public Health Funding over Past Decade: New Brief Explores Public Health Funding Estimates on State Health Compare
June 8, 2021:New data collected by the Trust for America’s Health show that most states (43) and the District of Columbia maintained or increased total public health funding levels in FY 2020 amid the COVID-19 public health emergency. However, seven states decreased their total public health funding during this time, and TFAH points out that increases due to state-supported COVID-19 response funding are unlikely to lead to sustained funding growth. It will be important to continue monitoring state funding for public health activities throughout and after the COVID-19 emergency, as these activities have been persistently underfunded over time.1
A new SHADAC brief provides an overview of TFAH’s FY 2020 data on state public health funding--which we standardize to the estimated population of each state to create per-capita estimates--looking at state variation in 2020 and trends over the last decade. SHADAC’s State Health Compare web tool provides access to these per-capita estimates, which are available for data years 2005 through 2020.2
Highlights from the brief are below.
Wide State Variation in Per Capita Public Health Funding Persisted in 2020
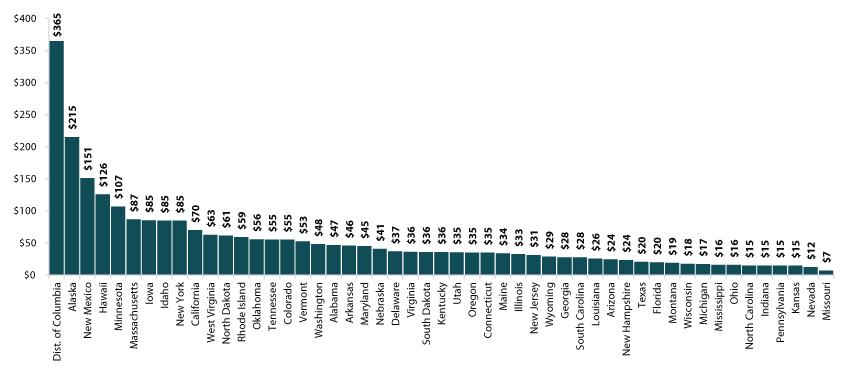
As in 2019, there was a wide gap between state public health funding levels among states in 2020, with state-provided funding ranging from $7 per capita in Missouri to $365 per capita in the District of Columbia. While Missouri’s spending held steady at $7 per capita between 2019 and 2020, the District of Columbia increased its funding by $2 per capita and stayed far ahead of the next-highest funding rate of $215 per capita seen in Alaska. Kentucky held the median spot for 2020, spending $36 per person on public health.
Figure 1. Per Person Public Health Funding, 2020
A Handful of States Consistently Near the Top for Public Health Spending
Five states (Alaska, Hawaii, Idaho, New York, and California) and the District of Columbia were consistently among the top 10 for public health funding over the course of the last 10 years (2011 through 2020). Alaska, the District of Columbia, and Hawaii were among the top five for public health spending during each of the last ten years as well, with Alaska and Hawaii each having been the top spending state four times.
A Few States Consistently among Lowest-Ranked for Public Health Spending
There was more movement among the ranks of the states with the lowest public health spending than among the highest-ranking states from 2011 to 2020. Just three states were consistently among the bottom 10 for public health spending during this time: Missouri, Nevada, and Mississippi. Missouri and Nevada were among the bottom five for public health spending during each of the last ten years as well, and each of the two states was the lowest spending state overall five times.
Explore Additional Public Health Data at State Health Compare
Visit State Health Compare to explore national and state-level estimates for the following public health indicators:
- Weight Assessment in Schools
- School Nutrition Standards Stronger than USDA
- School Required to Provide Physical Activity
- Smoke Free Campuses
- Cigarette Tax Rates
State Health Compare also features a number of other indicator categories, including health insurance coverage, cost of care, access to and utilization of care, care quality, health behaviors, health outcomes, and social determinants of health.
1 McKillop, M., & Lieberman, D.A. (May 2021). “The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2021.” Trust for America’s Health Issue Report. Available at https://www.tfah.org/wp-content/uploads/2021/05/2021_PHFunding_Fnl.pdf
2 With the exception of data year 2006, for which no estimates are available.
Blog & News
U.S. Alcohol-Related Deaths Grew Nearly 50% in Two Decades: SHADAC Briefs Examine the Numbers among Subgroups and States
April 19, 2021:In the midst of the opioid epidemic, the United States has been quietly experiencing another mounting public health crisis as deaths involving alcohol have grown to historic highs. After years of stability, the rate of alcohol-related deaths began to increase in 2007 and has increased significantly almost every year since according to vital statistics data from the U.S. Centers for Disease Control and Prevention (CDC).
Because alcohol contributes to so many diseases, it is challenging to calculate a complete death toll for alcohol. However, even a conservative estimate that counts only causes of death that are 100 percent attributable to alcohol yields a rate of 10.4 deaths per 100,000 people in 2019—49 percent higher than the U.S. rate in 2006—representing over 39,00 deaths nationwide.
This trend in alcohol-related death rates predates the COVID-19 pandemic, during which time research indicates that there have been concerning changes in alcohol use..i,ii, iii For instance, some states have reported increased alcohol sales, and surveys have found increases in alcohol consumption and high-risk drinking behaviors, such as heavy drinking and binge drinking.iv,v,vi,vii According to a SHADAC COVID-19 survey conducted in April 2020, 15.4% of adults nationwide reported increased alcohol consumption due to the stress of COVID, with numbers up across demographic categories of race, age, gender, and educational attainment. While experts will look to alcohol-related death rates as one important indicator of the behavioral health impact of COVID-19, data on alcohol-related deaths for 2020 will not be available until next year at the earliest. In the meantime, new vital statistics data from 2019, estimates of which can be found on the SHADAC’s State Health Compare, provide an updated baseline to help understand potential changes during and since the COVID-19 crisis.

 A new SHADAC brief draws on CDC vital statistics data to present trends and variations in alcohol-related death rates across the nation, among the states, and by subpopulation breakdowns from 2006 to 2019. The brief paints a picture of the current landscape of alcohol-related deaths—highlighting geographic areas and demographic groups that warrant particular attention.
A new SHADAC brief draws on CDC vital statistics data to present trends and variations in alcohol-related death rates across the nation, among the states, and by subpopulation breakdowns from 2006 to 2019. The brief paints a picture of the current landscape of alcohol-related deaths—highlighting geographic areas and demographic groups that warrant particular attention.
To accompany the issue brief, SHADAC also developed infographics for all 50 states and the District of Columbia. These infographics present trends in state-level alcohol-involved death rates from 2000-2019, show how each state's 2019 rate compares to the national average, and provide a glimpse into how 2019 alcohol-involved death rates and opioid overdose death rates compare in each state.
Below are a few highlighted findings from the issue brief.
National and State Alcohol-Related Death Rates Trending Upward Since 2006
After years of stability, deaths from total alcohol-involved causes increased significantly beginning in 2007 and continued to grow through 2019, which is the most recent year for which data are available. Since 2006, death rates from total alcohol-related causes grew significantly in 11 out of 13 years, increasing by 49% overall between 2006 and 2019.
U.S. alcohol-involved death rates, 2000-2019

From 2006 to 2019, death rates from total alcohol-involved causes increased significantly in nearly all states, with 48 states seeing increases during this time. Only two states (Alaska and Hawaii) had statistically unchanged rates, while the District of Columbia saw a statistically significant decline in alcohol-involved death rates.
Wide State Variation in Alcohol-Involved Death Rates, with Rates Higher in the Western U.S.
Although almost all states experienced statistically significant increases in alcohol-involved deaths since 2006, there was a wide variation in death rates across the states. For instance, in 2019, New Mexico had the highest death rate from alcohol-involved causes, at 34.3 deaths per 100,000 people, which was almost six times the lowest rate of 5.9 deaths per 100,000 people in Hawaii.
A map of state alcohol-involved death rates compared to the U.S. rate illustrates a regional pattern, with the highest death rates largely found in the western portion of the country. Of the 21 states with alcohol-involved death rates that were significantly higher than the U.S. rate of 10.4 deaths per 100,000 people in 2019, all but three (New Hampshire, Tennessee, and Vermont) were found west of the Mississippi River. Additionally, only four states west of the Mississippi (Hawaii, Louisiana, Missouri, and Texas) had alcohol-involved death rates that were significantly lower than the U.S. rate.
State alcohol-involved death rates per 100,000 compared to the U.S. rate, 2019

National Alcohol-Involved Death Rates Varied Widely by Race/Ethnicity, but All Groups Saw Increases
Between 2006 and 2019, all racial and ethnic groups that we examined experienced statistically significant increases in their alcohol-involved death rates. However, there was still wide variation in alcohol-involved death rate patterns between them.
In 2019, American Indian and Alaska Native people had the highest total alcohol-involved death rate, at 50.5 deaths per 100,000 people, which was significantly above the overall population rate of 10.4 deaths per 100,000 people. The 2019 rate for American Indian and Alaska Native people was also 64 percent higher than their 2006 rate of 30.8 deaths per 100,000 people, representing the largest increase among racial and ethnic groups.
White people had the second-highest alcohol-involved death rate in 2019, at 11.1 deaths per 100,000 people, which was significantly higher than the overall population rate. Their rate has increased 61 percent since 2006 (when the rate was 6.9 deaths per 100,000 people), which was the second largest increase among racial and ethnic groups.
U.S. alcohol-involved death rates by race/ethnicity, 2006 and 2019

For further analysis, including an examination of national alcohol-related death rates by age, sex, and urbanization, see the full SHADAC issue brief.
About the Data
SHADAC accesses vital statistics data from the Centers for Disease Control and Prevention, National Center for Health Statistics, via the CDC Wonder Database.
Except where otherwise indicated, rates of suicide deaths presented here are age-adjusted. Rates and standard errors were obtained from the CDC Wonder Database using ICD-10 cause of death codes for a limited set of health conditions considered by the CDC to be 100 percent attributable to alcohol as the primary cause of death. viii Additionally, we only include deaths in which an alcohol-attributable cause was listed as the “underlying cause of death” (i.e., the direct cause), rather than including deaths in which an alcohol-attributable cause was listed as a “multiple causes of death” (i.e., a contributing cause).
Explore the Data
Alcohol-involved death rate data from the CDC WONDER Database can be accessed on SHADAC’s State Health Compare. Data are available for the years 2000 to 2019 for the U.S. and all 50 states and the District of Columbia, and can be analyzed by age, sex, race/ethnicity, and metropolitan status.
i Grossman, E.R., Benjamin-Neelon, S.E., & Sonnenschein, S. (2020). “Alcohol Consumption during the Covid-19 Pandemic; A Cross-Sectional Survey of US Adults.” Int J Environ Res Public Health 17(24): 9189. Doi: https://dx.doi.org/10.3390%2Fijerph17249189
ii Pollard, M.S., Tucker, J.S., & Green, H.D. (2020). “Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US.” JAMA Netw Open 3(9): :e2022942. doi:10.1001/jamanetworkopen.2020.22942
iii American Psychological Association. (2021). “One year later, a new wave of pandemic health concerns.” American Psychological Association. Available at https://www.apa.org/news/press/releases/stress/2021/one-year-pandemic-stress
iv https://pubs.niaaa.nih.gov/publications/surveillance-covid-19/COVSALES.htm#fig1
v https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2770975
vi https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7763183/
vii https://www.tandfonline.com/doi/full/10.1080/00952990.2020.1832508
viii https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html
Publication
Escalating Alcohol-Involved Death Rates: Trends and Variation across the Nation and in the States from 2006 to 2019 (Infographics)
April 19, 2021
In the midst of the opioid epidemic, the United States has been quietly experiencing another mounting public health crisis as deaths involving alcohol have grown to historic highs. After years of stability, the rate of alcohol-related deaths began to increase in 2007 and has increased significantly almost every year since, growing by 49 percent to 10.4 deaths per 100,000 people in 2019. Of the 414,000 alcohol-involved deaths that occurred nationwide during the 2006 to 2019 time period, 88,000 would not have occurred if alcohol-involved deaths had held steady at 2006 rates.
 In an effort to shed light on the growing issue of alcohol-involved deaths, SHADAC researchers have produced an issue brief that describes trends and variation in alcohol-involved death rates at the state and national levels, and among demographic subgroups, using vital statistics data from the Centers for Disease Control and Prevention for 2006 to 2019.
In an effort to shed light on the growing issue of alcohol-involved deaths, SHADAC researchers have produced an issue brief that describes trends and variation in alcohol-involved death rates at the state and national levels, and among demographic subgroups, using vital statistics data from the Centers for Disease Control and Prevention for 2006 to 2019.
To accompany the issue brief, SHADAC also developed infographics for all 50 states and the District of Columbia. These infographics present trends in state-level alcohol-involved death rates from 2000-2019, show how each state's 2019 rate compares to the national average, and provide a glimpse into how 2019 alcohol-involved death rates and opioid overdose death rates compare in each state.
State alcohol-involved deaths per 100,000 people, 2019
Click on a state below view its infographic.
Quick infographic links: the United States, the District of Columbia, and All States.
Related Reading:
U.S. Alcohol-Related Deaths Grew Nearly 50% in Two Decades: SHADAC Briefs Examine the Numbers among Subgroups and States (SHADAC Blog)
Overdose Crisis in Transition: Changing National and State Trends in a Widening Drug Death Epidemic (SHADAC Briefs)
50-State Analysis of Drug Overdose Trends: The Evolving Opioid Crisis Across the States (Infographics)














