Blog & News
Kids' Health Data Highlight: Trouble Affording Nutritious Meals in 2016 (Infographic)
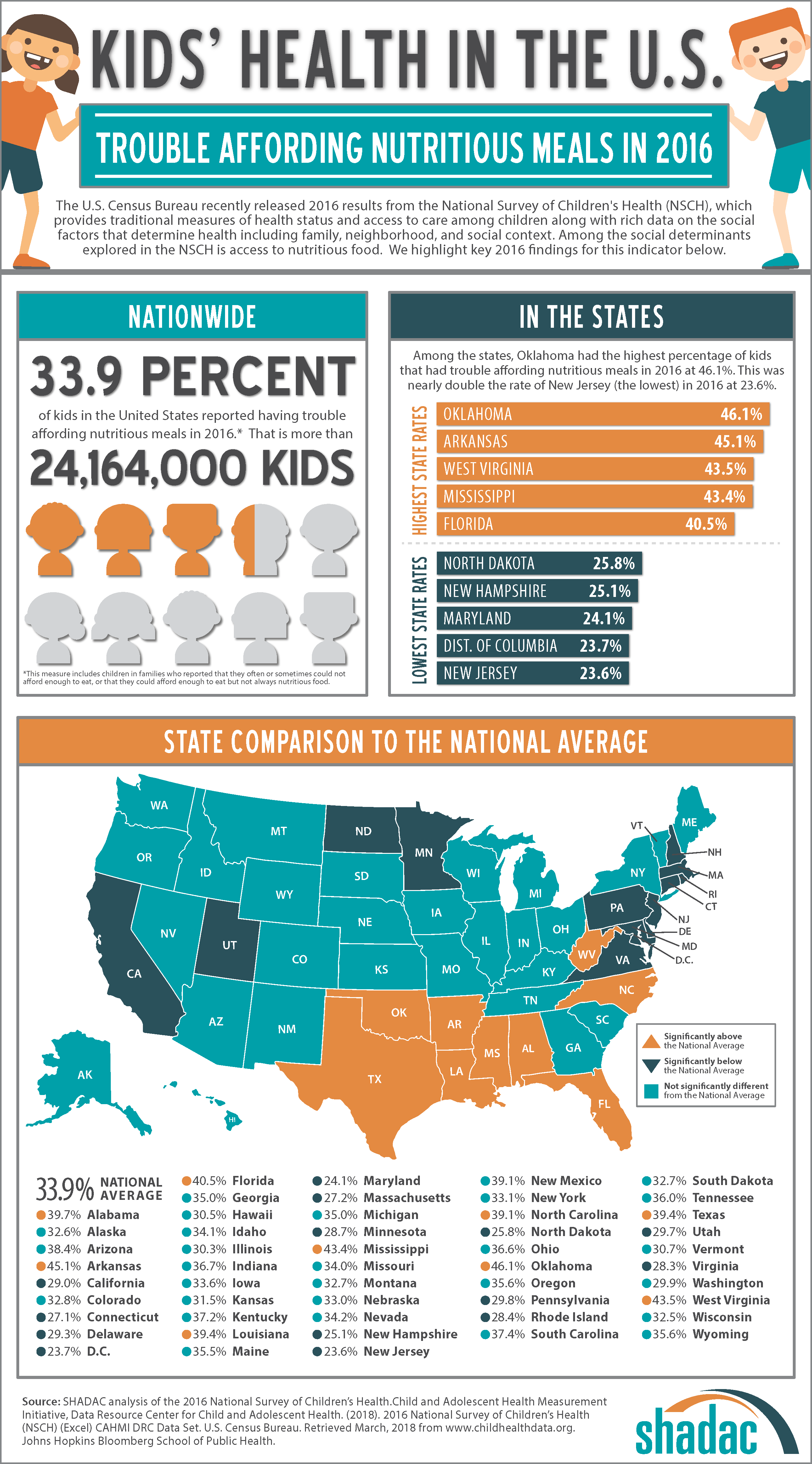
March 29, 2019:It is increasingly clear that health is determined not just by biological and clinical factors but to a greater extent by socio-demographic factors. With this in mind, we need data for monitoring the social determinants of health just as we do for monitoring biological and clinical determinants. The U.S. Census Bureau recently released estimates from the 2016 National Survey of Children’s Health (NSCH), providing a data source that is ideal for precisely this purpose. The NSCH provides traditional measures of health status and access to care among children along with rich data on the social factors that determine health including family, neighborhood, school, and social context.
In the coming weeks, SHADAC is highlighting state-specific findings from the 2016 NCSH on measures that illustrate where states are closer to achieving a culture of health and where improvements can be made. As additional years of NCSH data are released, we will be able to monitor trends in these indicators to track progress in developing a culture of health over time.
According to 2016 data from the NSCH, 33.9% of children nationwide (approximately 24,164,000 children) had trouble affording nutritious meals in 2016.[1]
The five states with the highest percentages of children who had trouble affording nutritious meals in 2016 were Oklahoma (46.1%), Arkansas (45.1%), West Virginia (43.5%), Mississippi (43.4%), and Florida (40.5%).
The five states with the lowest percentages of children who had trouble affording nutritious meals in 2016 were New Jersey (23.6%), the District of Columbia (23.7%), Maryland (24.1%), New Hampshire (25.1%), and North Dakota (25.8%).
In all, the percentage of children that had trouble affording nutritious meals was statistically below the national average in 14 states and statistically above the national average in nine states.
Click on the infographic for additional state-level information about children’s access to nutritious meals.
Additional Kids’ Health Data Highlights
Kids' Health in the U.S.: Difficulties Making or Keeping Friends in 2016
Kids' Health in the U.S.: Parental Attendance at Kids' Activities in 2016
Kids'Health in the U.S.: Living in Neighborhoods with No Amenities in 2016
Kids’ Health in the U.S.: Living in Supportive Neighborhoods in 2016
Kids’ Health in the U.S.: Living in Working Poor Households in 2016
More about the NSCH
The NSCH was administered three times prior to 2016 – in 2003, 2007, and 2011/12. However, the 2016 NSCH is different because it integrated the NSCH with the National Survey of Children with Special Health Care Needs (NS-CSHCN) and introduced a number of new survey items, establishing a new baseline. Going forward, the NSCH will be administered annually. The survey is administered online and via mail, and survey results are weighted to represent the population of non-institutionalized children ages 0-17 who live in housing units nationally and in each state.
The full 2016 NSCH public-use file (PUF) is available on the Census Bureau’s NSCH page
[1] This estimate includes children in families who reported that they often or sometimes could not afford enough to eat or that they could afford enough to eat but not always nutritious food.
Blog & News
2016 County Health Insurance Estimates Now Available
March 2018:The U.S. Census Bureau released Small Area Health Insurance Estimates (SAHIE) for 2016, providing estimates of health insurance coverage for all counties and states.
The SAHIE program is the only source of single-year health insurance estimates for every county in the US. Estimates are available for each county by sex, age, and Federal Poverty Level (FPL). Race/ethnicity information is available at the state level.
The following are highlights from the 2016 SAHIE release.
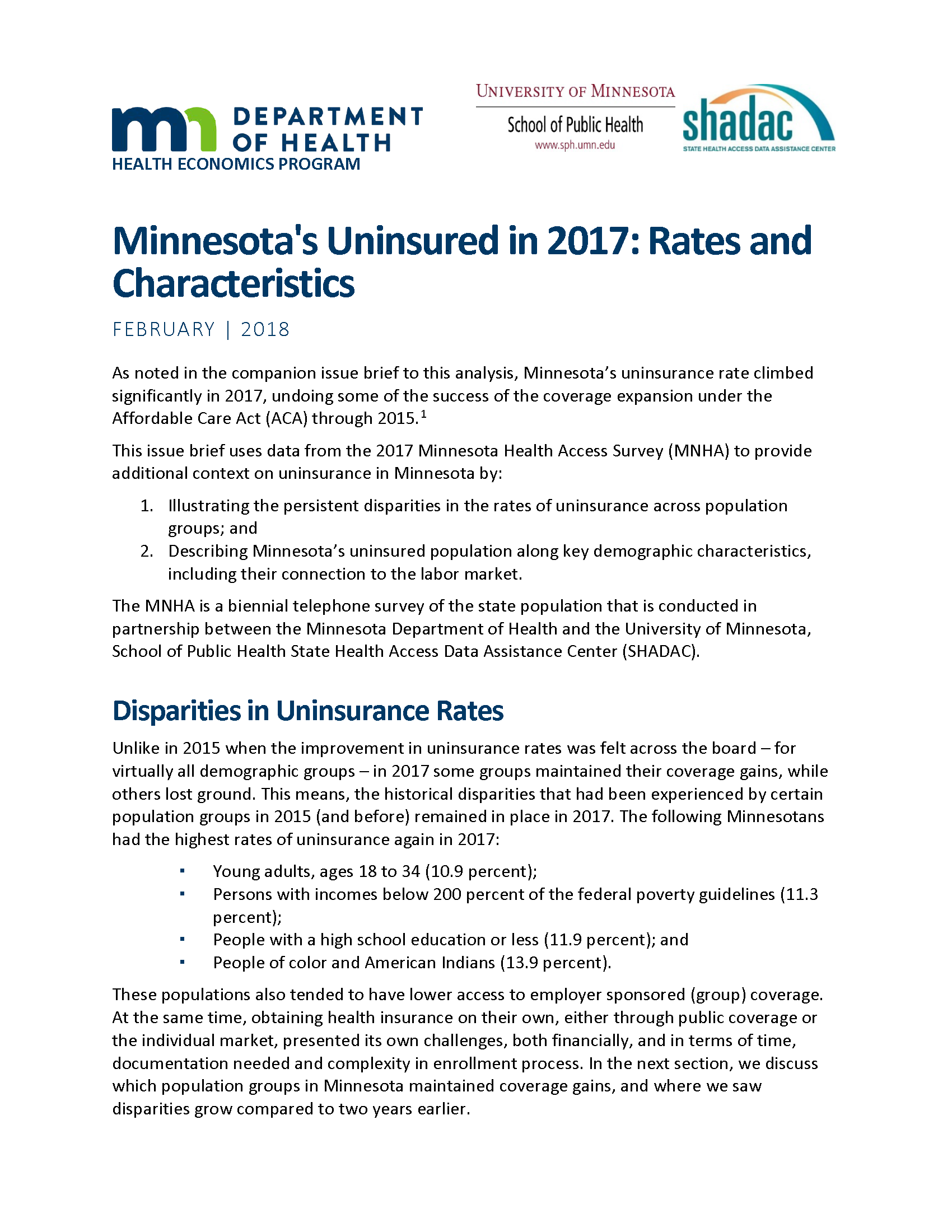
 Nationwide, county uninsured rates for the nonelderly population (i.e., under age 65) ranged from 2.1% to 33.5% in 2016, with a median county uninsured rate of 10.4%
Nationwide, county uninsured rates for the nonelderly population (i.e., under age 65) ranged from 2.1% to 33.5% in 2016, with a median county uninsured rate of 10.4%- In 1,213 counties, (38.6% of all counties), the 2016 nonelderly uninsured rate was at or below 10%. Only 425 counties (13.5 %) had uninsured rates greater than or equal to 15.0% (Figure 1).
- Alaska, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Texas all had counties with 2016 nonelderly uninsurance rates that exceeded 30%.
- The nonelderly uninsured rate decreased between 2015 and 2016 in 629 counties, or 20.0% of all counties. In all, only eight counties experienced an increase in nonelderly uninsured rates from 2015 to 2016.
- In states that expanded Medicaid aimed at low-income working-age adults, 350 counties (23.4% of counties) had a decrease in the uninsured rate for this population compared with 92 (5.6% of counties) in states that did not expand.
Access the full 2016 SAHIE report and visualizations.
Access the 2016 SAHIE estimates.
Find your county’s 2016 uninsured rate using SAHIE’s interactive data tool.
About SAHIE
SAHIE are created using statistical models that combine American Community Survey (ACS) data with population estimates and administrative records.
SAHIE are consistent with the direct ACS survey estimates, but SAHIE are more precise than the ACS 1-year and 5-year survey estimates alone for most counties because SAHIE are supplemented with other data sources.
SHADAC Brief #26 provides an overview of how the SAHIE are developed as well as a comparison of the SAHIE model-based methodology to that used by ACS (see Table 2).
Blog & News
Which Minnesotans Were Uninsured in 2017?
March 13, 2018:Recent findings from the biennial Minnesota Health Access Survey show that Minnesota’s uninsurance rate grew significantly from 4.3 percent in 2015 to 6.3 percent in 2017. However, results also show that uninsurance rates varied among subpopulations in 2017, as did changes in these rates, with coverage holding steady for some populations from 2015 to 2017 while decreasing for others. Similarly, the distribution of various characteristics among Minnesota’s uninsured differs in a variety of instances from the distribution of these characteristics within the state more broadly.
Most Likely to Be Uninsured in 2017
Among Minnesotans, certain subpopulations had higher than average rates of uninsurance in 2017. The highest rates were found among the following groups:
- Young adults, ages 18 to 34 (10.9%)
- People with incomes below 200 percent of the federal poverty guidelines (FPG; 11.3%)
- People with a high school education or less (11.9%)
- People of color and American Indians (13.9%)
Changes in Uninsurance from 2015 to 2017
Changes in uninsurance did not occur uniformly throughout the Minnesota from 2015 to 2017. Variations were seen by income, education, race/ethnicity, and age.
- By income, the largest increase in uninsurance, relative to 2015 levels, occurred among people at 300% FPG or above, although their overall rate of uninsurance remained below the 6.3% state average (5.1% for 301 to 400% FPG, and 3.4% for those at or above 401% FPG) and below that of people at any other income level.
- People with the lowest educational attainment (all categories below a completed college education) saw increases in uninsurance, while uninsurance was unchanged among Minnesotans with college or postgraduate degrees. From 2015 to 2017, uninsurance increased from 12.1% to 20.5% among Minnesotans with less than a high school diploma; from 6.3% to 9.4% among Minnesotans with only a high school diploma, and from 3.5% to 4.8% among Minnesotans with some college or technical school.
- Among racial and ethnic groups, Whites, Hispanics/Latinos, and Asians all saw significant increases in uninsurance from 2015 to 2017, although the magnitude of these increases was higher for Hispanics/Latinos and Asians than for Whites, for whom uninsurance remained below the state average. Uninsurance grew from 3.4% to 4.6% among Whites; from 11.4% to 21.8% among Hispanics/Latinos; and from 4.1% to 10.3% among Asians.
- All adults under age 65, except young adults ages 26 to 34 years, saw significant increases in uninsurance from 2015 to 2017. Uninsurance grew from 6.2% to 11.8% among 18 to 25 year-olds; from 8.2% to 10.3% among 26 to 34 year-olds; from 5.2% to 8.3% among 35 to 54 year-olds; and from 2.8% to 5.7% among 55 to 64 year-olds.
Characteristics of the Uninsured in 2017
The characteristics of Minnesota’s uninsured in 2017 are different in a number of ways compared to the state’s population overall. Compared to Minnesotans overall, uninsured Minnesotans are more likely to:
- Be temporary or seasonal workers (27.4% vs. 9.7%)
- Be self-employed (22.0% vs. 12.5%)
- Work for employers with 50 or fewer employees (60.0% vs. 30.7%).
- Have a high-school degree or less (57.4% vs. 30.1%)
- Be adults aged 18 to 64 (84.9% vs. 61.6%)
- Be born outside the United States (25.7% vs. 9.1%)
- Have incomes below 200% FPG (46.4% vs. 25.8%)
- Be people of color and American Indians (43.9% vs. 19.3%)
- Report fair or poor health (21.5% vs. 12.7%)
- Experience more unhealthy days related to mental health (4.6 days in the last 30 days vs. 2.9 days)
- Lack confidence in getting needed medical care (38.2% vs. 9.9%)
- Report foregoing care due to costs (46.0% vs. 21.0%)
Read the full brief detailing these findings, from SHADAC and the Minnesota Department of Health’s Health Economics Program.
Publication
Section 1115 Medicaid Expansion Waivers: Implementation Experiences
This report summarizes SHADAC's analysis of how four states implemented Section 1115 Medicaid expansion wiavers. These states--Arkansas, Indiana, Iowa, and Michigan--are among eight that have expanded their Medicaid programs through Section 1115 of the Social Security Act rather than through the expansion option available under the Affordable Care Act (ACA).
 SHADAC's analysis was commissioned by the Medicaid and CHIP Payment and Access Commission (MACPAC) and sought to understan how Arkansas, Indiana, Iowa, and Michigan approached the implementation of key provisions of their Section 1115 Medicaid expansion waivers:
SHADAC's analysis was commissioned by the Medicaid and CHIP Payment and Access Commission (MACPAC) and sought to understan how Arkansas, Indiana, Iowa, and Michigan approached the implementation of key provisions of their Section 1115 Medicaid expansion waivers:
- Exchange plan premium assistance (Arkansas & Iowa)
- Enrollee contribution requirements (Iowa & Michigan)
- Health savings accounts (Arkansas & Indiana)
- Healthy behavior incentives (Indiana, Iowa, & Michigan)
- Graduated copayments for emergency department use (Indiana)
SHADAC researchers conducted interviews with 33 individuals representing current and former state agency staff and health insurance carriers in the four study states to identify the steps that states took to operationalize their programs. The report provides background information on the waiver program elements implemented in each of the four study states, summarizes the key pieces of administrative capacity that states put into place to implement their waivers, and details the specific program challenges they faced.
Publication
Health Care Coverage and Access Among Children, Adolescents, and Young Adults, 2010-2016: Implications for Future Health Reforms
 Spencer, DL, McManus, M, Call, KT, Turner, J, Harwood, C., White P, & Alarcon, G. (2018). "Health Care Coverage and Access Among children, Adolescents, and Young Adults, 2010-2016: Implications for Future Health Reforms." Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2017.12.012
Spencer, DL, McManus, M, Call, KT, Turner, J, Harwood, C., White P, & Alarcon, G. (2018). "Health Care Coverage and Access Among children, Adolescents, and Young Adults, 2010-2016: Implications for Future Health Reforms." Journal of Adolescent Health. doi: 10.1016/j.jadohealth.2017.12.012
This article examines changes to health insurance coverage and access to health care among children, adolescents, and young adults since the implementation of the Affordable Care Act using data from the National Health Interview Survey. The authors found significant improvements in coverage among children, adolescents, and young adults since 2010, along with some gains in access. There were few age-group differences in overall coverage and access trends, but the analysis did find an age-gradient pattern, such that coverage and access rates were incrementally worse for young adolescents, older adolescents, and young adults.