Blog & News
Children's Health Insurance Coverage, 2013-2016: Post-ACA Reductions in Uninsurance Persisted
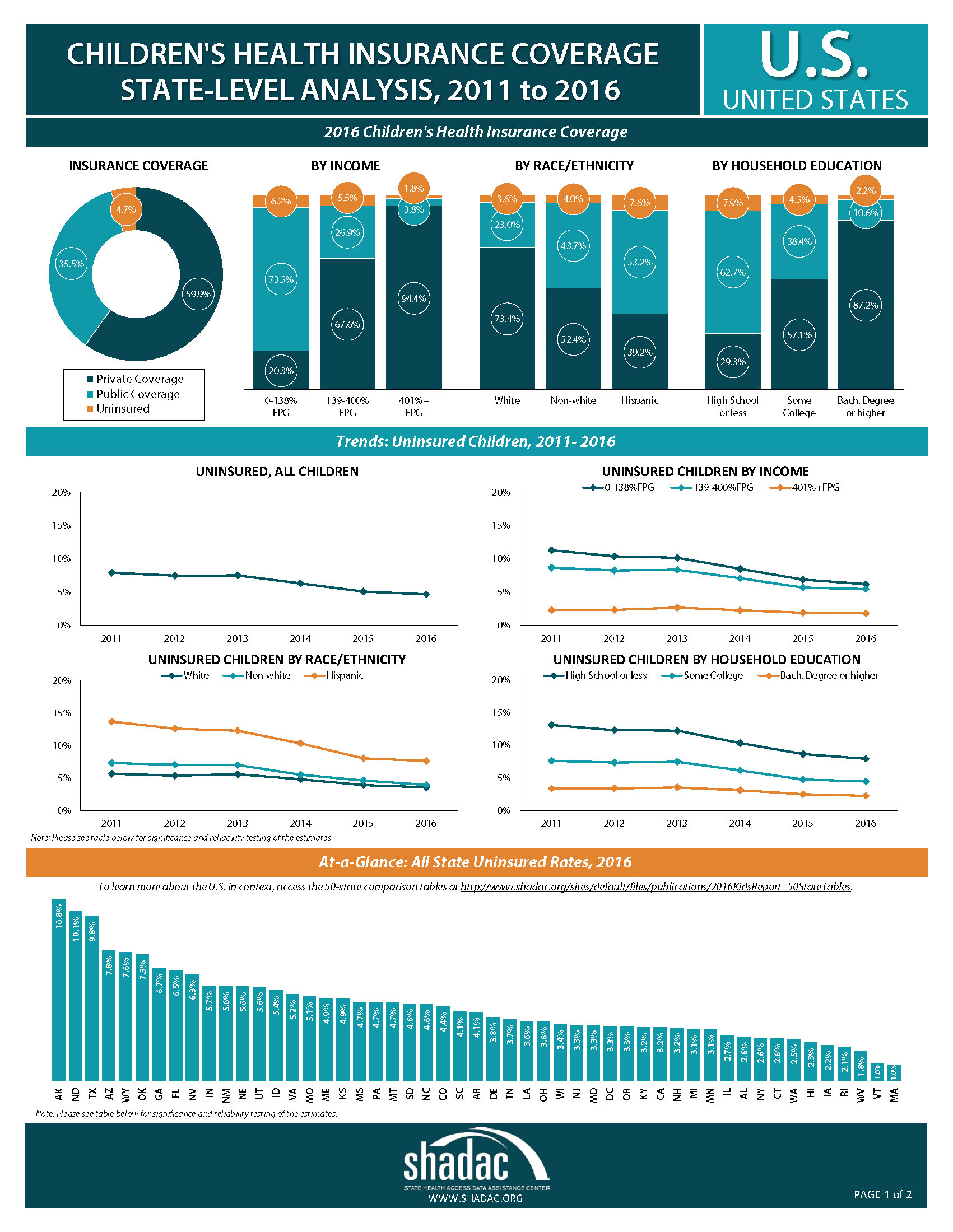
March 05, 2020:A new analysis from SHADAC examines health insurance coverage among children in the United States from 2013 through 2016, looking at changes in children’s coverage before and after the coverage provisions of the Affordable Care Act (ACA) took effect in 2014. The report examines coverage at both the national and state level, among children as a whole and by income, race/ethnicity, and educational attainment.
Key Findings
- Children in the United States have seen significant declines in uninsurance since the coverage provisions of the ACA took effect, with the number of uninsured children dropping by 2.2 million, or 2.9 percentage points (pp), between 2013 and 2016. These coverage gains were sustained despite an uncertain policy climate around the ACA.
- Recent reductions in the rate of uninsurance among children were driven by increases in both public and private coverage from 2013 to 2016, although public coverage increases were greater than increases in private coverage, at 1.8 pp and 1.1 pp, respectively.
- Drops in uninsurance were seen across demographic categories, and some of the largest coverage gains continued to be made by groups of children that have historically had the highest rates of uninsurance: low-income, Hispanic, and non-white children and children in households with low educational attainment. Despite coverage gains, coverage rates for these groups are still significantly below those of high-income children and white children, and coverage varies across states.
"The decline in the number of uninsured children after the enactment of the ACA is historic and persistent," noted report author Elizabeth Lukanen. "It is especially encouraging to see uninsurance rates drop in almost all states and across children of different demographic and income groups. Given the uncertain health policy environment, ongoing monitoring of children’s uninsurance will be necessary to ensure that reductions in uninsurance are sustained."
Explore the Analysis
The following products present findings from this analysis:
- Summary chartbook highlighting key findings on coverage among children from 2013 to 2016 at the national and state level and by income, race/ethnicity, and educational attainment
- Two-page profiles of children’s coverage for each state
- 50-state map linking to individual state profile pages
- 50-state comparison tables
About the Data
This analysis uses data from the American Community Survey (ACS).
Blog & News
Sarah Gollust in Health Affairs: TV Advertising Volumes Were Associated with Insurance Marketplace Shopping and Enrollment In 2014
June 05, 2018:According to an article released in Health Affairs, people living in counties with higher numbers of television advertisements sponsored by the federal government were significantly more likely to shop for and enroll in a Marketplace plan. Sarah Gollust of the University of Minnesota, School of Public Health was the lead author of this analysis, which was funded through Dr. Gollust’s SHARE grant. The paper was co-authored by Andrew Wilcock (Harvard Medical School), Erika Franklin Fowler (Wesleyan University), Colleen Barry (Johns Hopkins Bloomberg School of Public Health), Jeff Neiderdeppe (Cornell University), Laura Baum (Wesleyan University), and Pinar Karaca-Mandic (University of Minnesota).
Overview: Effectiveness of Health Insurance Advertising
The effectiveness of health insurance advertising has gained renewed attention following reductions to the marketing budget for the federal Marketplace, but there is limited evidence on the relationship between advertising and enrollment behavior. Dr. Gollust and her co-authors combined survey data from the 2014 National Health Interview Survey (NHIS) on adults ages 18–64 with data on volumes of televised advertisements aired in respondents’ counties of residence during the 2013–2014 open enrollment period to study whether the volumes of televised content were associated with the shopping and enrollment behavior of U.S. adults in the new health insurance Marketplaces in 2014.
Key Findings
The researchers found that people living in counties with higher numbers of ads sponsored by the federal government during the 2013-2014 open enrollment period were significantly more likely to shop for and enroll in a Marketplace plan in 2014. On the other hand, people living in counties with higher numbers of political ads opposing the ACA were less likely to shop for or enroll in a Marketplace plan.
Shopping for a Marketplace Plan
According to the analysis, the probability of shopping for a plan on the Marketplace was 13.4% in counties in the tenth percentile of volume of federal ads, compared to 16.2% in counties in the ninetieth percentile. Conversely, the probability of shopping for a Marketplace plan was 14.2% in counties in the tenth percentile of volume of political ads, compared to 12.9% in counties in the ninetieth percentile.
Enrolling in a Marketplace Plan
Similarly, the probability of enrolling in a Marketplace plan was 3.7% for respondents in counties with median volumes of federal ads, compared with 5.2% for respondents in counties in the ninetieth percentile. In contrast, the probability of enrolling in a Marketplace plan was 4.5% in counties in the tenth percentile of volume for political ads, compared to 3.3% in counties in the ninetieth percentile.
Policy Implications
This study shows that advertising efforts are likely an important component of health insurance enrollment campaigns. The authors note, however, that these findings might not extrapolate to the 2018 enrollment period, when 11.8 million Americans enrolled in HealthCare.gov plans despite federal cuts to all television advertising. These findings are from a period when the ACA was new, during which time advertising from all sponsors may have played a particularly important role and during which time the messaging was likely different.
Learn More
Read the full Health Affairs article to learn more about study methods, findings, and policy implications.
Publication
Affordable Care Act Impact in Kentucky: Increasing Access, Reducing Disparities
The American Journal of Public Health (AJPH) has just released a SHADAC-authored article, “Affordable Care Act in Kentucky: Increasing Access, Reducing Disparities.” The piece was co-authored by SHADAC Director Lynn A. Blewett along with SHADAC researchers Colin Planalp and Giovann Alarcón. The authors used data from the American Community Survey (ACS) to examine changes in uninsurance and uninsurance disparities by race/ethnicity in Kentucky since the state’s implementation of the Affordable Care Act (ACA).
Key Findings: Kentucky’s Uninsured
The authors found that Kentucky’s uninsurance rate for all ages declined significantly between 2013 and 2015, from 14.4% to 6.1%. Among racial/ethnic groups, the largest decline in the uninsurance was experienced by Blacks (from 16.7% uninsured in 2013 to 5.5% in 2015), although uninsurance rates among the state’s White and Hispanic populations also declined significantly (from 13.3% to 5.3% and from 34.5% to 24.2%, respectively). Only the uninsurance rate for Asians remained statistically unchanged between 2013 and 2015.
Key Findings: Disparities
In Kentucky in 2015, coverage disparities among Blacks were eliminated. In 2013, Blacks were overrepresented among the uninsured, accounting for 8.9% of the state’s uninsured while representing a smaller 7.7% of the state’s population. But in 2015, Blacks represented 7.1% of the state’s uninsured, which was not significantly different from their overall proportion of the population in 2015 (7.8%). However, Whites did continue to experience favorable disparities in 2015, being underrepresented among the uninsured, at 74.2%, compared with their share of the population, at 85.4%. Moreover, Kentucky’s Hispanic/Latino population remained overrepresented among the state’s uninsured in 2015, making up 13.0% of the state’s uninsured but only 3.3% of the state’s total population. Asians were also overrepresented among the uninsured in 2015, representing 2.8% of the uninsured but just 1.4% of the population.
Read the full American Journal of Public Health article to learn more about study methods and findings, as well as the role of health policy in reducing disparities.
Blog & News
SHADAC Research in American Journal of Public Health: ACA Led to Increased Health Insurance Access, Reduced Disparities in Kentucky
May 30, 2018:The American Journal of Public Health (AJPH) has just released a SHADAC-authored article, “Affordable Care Act in Kentucky: Increasing Access, Reducing Disparities.” The piece was co-authored by SHADAC Director Lynn A. Blewett along with SHADAC researchers Colin Planalp and Giovann Alarcón. The authors used data from the American Community Survey (ACS) to examine changes in uninsurance and uninsurance disparities by race/ethnicity in Kentucky since the state’s implementation of the Affordable Care Act (ACA).
 Key Findings: Kentucky’s Uninsured
Key Findings: Kentucky’s Uninsured
The authors found that Kentucky’s uninsurance rate for all ages declined significantly between 2013 and 2015, from 14.4% to 6.1%. Among racial/ethnic groups, the largest decline in the uninsurance was experienced by Blacks (from 16.7% uninsured in 2013 to 5.5% in 2015), although uninsurance rates among the state’s White and Hispanic populations also declined significantly (from 13.3% to 5.3% and from 34.5% to 24.2%, respectively). Only the uninsurance rate for Asians remained statistically unchanged between 2013 and 2015.
Key Findings: Disparities
In Kentucky in 2015, coverage disparities among Blacks were eliminated. In 2013, Blacks were overrepresented among the uninsured, accounting for 8.9% of the state’s uninsured while representing a smaller 7.7% of the state’s population. But in 2015, Blacks represented 7.1% of the state’s uninsured, which was not significantly different from their overall proportion of the population in 2015 (7.8%). However, Whites did continue to experience favorable disparities in 2015, being underrepresented among the uninsured, at 74.2%, compared with their share of the population, at 85.4%. Moreover, Kentucky’s Hispanic/Latino population remained overrepresented among the state’s uninsured in 2015, making up 13.0% of the state’s uninsured but only 3.3% of the state’s total population. Asians were also overrepresented among the uninsured in 2015, representing 2.8% of the uninsured but just 1.4% of the population.
Read the full American Journal of Public Health article to learn more about study methods and findings, as well as the role of health policy in reducing disparities.
Blog & News
NHIS: Insurance Coverage Held Steady Overall in 2017, but Key Income Groups Saw Changes
June 04, 2018:The National Center for Health Statistics (NCHS) released health insurance coverage estimates for 2017 from the National Health Interview Survey (NHIS) as part of the NHIS Early Release Program. These are the first available full-year coverage estimates for 2017 from a federal survey, with estimates available for the nation and 18 states.
Insurance Coverage Remained Stable Overall in 2017
Rates of insurance coverage remained statistically unchanged between 2016 and 2017 nationwide and in the 18 states for which NCHS released estimates among most populations by age, sex, race/ethnicity, Marketplace Type, Medicaid-expansion Status, and region (Figure 1). There were, however, significant changes in rates of insurance coverage among non-elderly adults by income level in 2017.
Health Insurance Coverage by Income
Increase in uninsurance and decrease in private coverage among those 250-400% FPL
Between 2016 and 2017, the rate of uninsurance increased from 10.1% to 12.6% among non-elderly adults (ages 18-64) with incomes between 250% and 400% of the federal poverty level (FPL). This change was statistically significant. This increase in uninsurance was coupled with a statistically significant decrease in private coverage from 78.2% in 2016 to 75.5% in 2017 among the same group (Figure 2).
Eligibility for premium tax credits insulate individuals in this income range from premium increases, so the observed increase in uninsurance and decrease in private coverage among this group suggests that some may have left the individual market in response to other factors such as uncertainty surrounding the status of the ACA, available premium subsidies, and the individual coverage mandate.
This hypothesis is supported by the lack of any statistically significant changes in private coverage among non-elderly adults with incomes too high to be eligible for premium tax credits (>400% FPL) and among non-elderly adults with incomes that make them eligible for cost-sharing subsidies and more generous premium tax credits (100%-250% FPL). Additionally, there was a small but statistically significant decrease in private health insurance coverage purchased through the ACA Health Insurance Marketplaces among non-elderly adults with incomes 200% FPL or higher (4.3% in 2016 to 3.8% in 2017).
Increase in private coverage, decrease in public coverage for those below 100% FPL
Between 2016 and 2017, the rate of private coverage increased from 21.6% to 26.5% among non-elderly adults with incomes below 100% FPL. This change was statistically significant. This increase in private coverage was coupled with a statistically significant decrease in public coverage from 53.7% in 2016 to 50.2% in 2017 (Figure 3). There was no statistically significant change in the uninsurance rate or in rates of private health insurance coverage purchased through the ACA Health Insurance Marketplaces among this group between 2016 and 2017. This evidence points to an increase in private coverage from sources other than the ACA Marketplaces and a corresponding decrease in public coverage (i.e., Medicaid).
We will continue to monitor changes in insurance coveraged among these and other income groups as more detailed 2017 data becomes available later this year.
About the Numbers
The above estimates provide a point-in-time measure of uninsurance, indicating the percent of persons without coverage at the time of the interview.
The sample size of the NHIS fell from 97,459 in 2016 to 78,074 in 2017, a decrease of 19.9%. This change is important because smaller sample sizes decrease the precision of estimate and hamper the ability to make state-level estimates, to make estimates for small or minority populations, and to statistically detect changes over time.
For more information about the early 2017 NHIS health insurance coverage estimates, read the National Center for Health Statistics brief.
Citation
Cohen, RA, Zammitti, EP, & Martinez, ME. May 22, 2018. “Health Insurance Coverage: Early Release Estimates from the National Health Interview Survey, 2017.” National Center for Health Statistics: National Health Interview Survey Early Release Program. Available at https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201805.pdf