Blog & News
NHIS: 2018 Uninsured Rate Unchanged from 2017
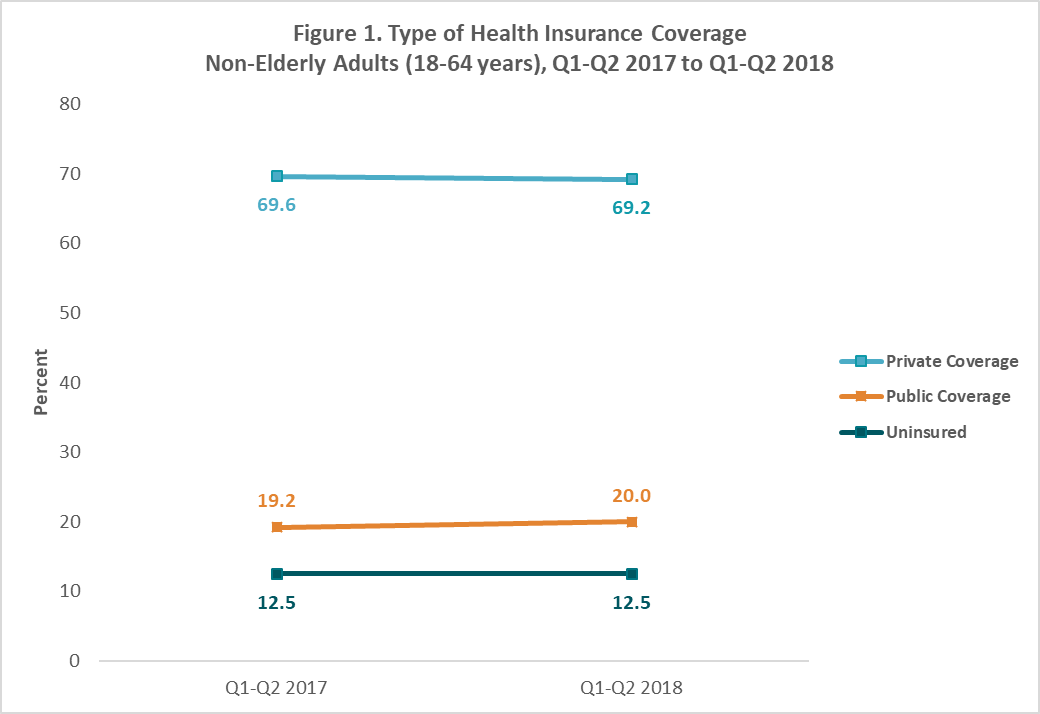
November 16, 2018:Nationwide, 12.5% of nonelderly adults (ages 18-64) were uninsured in the first half of 2018, unchanged from 12.5% in the same period in 2017.
This finding is based on new health insurance coverage estimates for Q1-Q2 2018 from the National Health Interview Survey (NHIS). These estimates were released by the National Center for Health Statistics (NCHS) as part of the NHIS Early Release Program and are the first available half-year coverage estimates for 2018 from a federal survey.
Uninsurance and Public and Private Coverage Rates Remained Stable for Nearly All Groups in 2018
The new NHIS estimates show that uninsurance rates, as well as rates of public and private coverage, were statistically unchanged across age, race/ethnicity, and income groups between the first half of 2017 and the first half of 2018. Figure 1 shows levels of health insurance coverage by type among non-elderly adults overall across this time period.
Changes in Coverage Type among Some Subgroups
The rate of public coverage among non-elderly adults with incomes below 100% of the federal poverty level (FPL) increased to 55.8% in the first half of 2018 from 51.4% in the first half of 2017, while the rate of private coverage among this group decreased to 20.0% in the first half of 2018 from 25.8% in the first half of 2017 (Figure 2). The rate of uninsurance among this group remained statistically unchanged over the same period.
The rate of public coverage also increased among all non-elderly persons (age 0–64) with incomes at or above 200% FPL, growing to 12.2% in the first half of 2018 from 11.2% in the first half of 2017. Non-elderly adults (age 18-64) with the same level of income also experienced an increase in public coverage over the same period, though this change was only significant at the 90% confidence level. Neither age group in this income range saw a significant change in private coverage or uninsurance from the first half of 2017 to the first half of 2018.
About the Numbers
The above estimates provide a point-in-time measure of health insurance coverage, indicating the percent of persons with that type of coverage at the time of the interview. The 2018 estimates are for the months of January to June 2018 and are based on a sample of 39,112 persons from the civilian noninstitutionalized population.
Differences described in this post are statistically significant at the 95% confidence level unless otherwise specified.
For more information about the early 2018 NHIS health insurance coverage estimates, read the National Center for Health Statistics brief.
Citation
Martinez, ME., Zammitti, EP., & Cohen, RA. November 15, 2018. “Health Insurance Coverage: Early Release Estimates from the National Health Interview Survey, January–June 2018.” National Center for Health Statistics: National Health Interview Survey Early Release Program. Available at https://www.cdc.gov/nchs/data/nhis/earlyrelease/Insur201811.pdf.
Blog & News
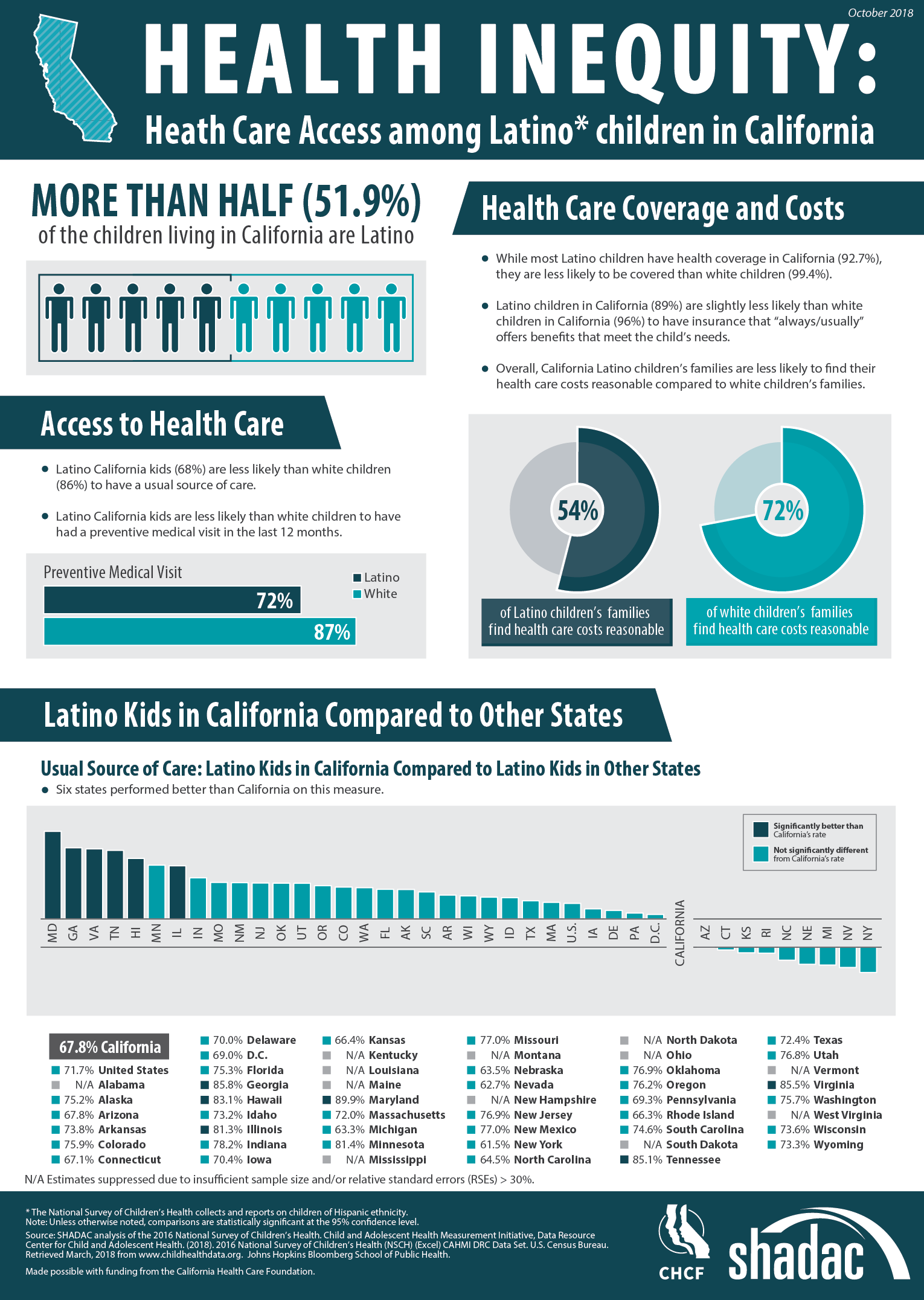
Latino Children in California Face Inequitable Access to Care (Infographic)
October 31, 2018:According to the 2016 National Survey of Children’s Health (NSCH), Latino children in California face lower access to health care than their white counterparts across multiple access indicators.
Despite representing more than half of children living in the state, Latino children are less likely than white children to: have health insurance coverage, have insurance benefits that meet their needs, find their health care costs reasonable, have a usual source of care, and have had a preventive medical visit in the last twelve months. The infographic presented here illustrates the 2016 NSCH estimates for these measures for both Latino and white children and also compares California’s performance to other states on the percentage of Latino children who have a usual source of care.
About the Data
The National Survey of Children’s Health is an annual survey funded and directed by the Health Resources and Services Administration (HRSA) Maternal and Child Health Bureau (MCHB). Learn more about the NSCH at www.childhealthdata.org.
Blog & News
Lynn Blewett in Health Affairs Blog: Examining the New Basic Health Plan Financing Rule
October 2018:On August 24th, the Centers for Medicare and Medicaid (CMS) released a Final Administrative Order that would revise and recalculate their payments toward Basic Health Programs (BHPs). Only two states have established BHPs—Minnesota and New York—under Section 1331 of the Affordable Care Act (ACA).
SHADAC Director Lynn Blewett and David Anderson, a researcher at the Duke University Margolis Center, co-authored a Health Affairs blog that takes a look at the background of BHPs in Minnesota and New York, how this new order affects them, and what may happen with federal BHP financing going forward.
BHP Background and Financing
BHPs are optional state coverage programs designed to improve continuity of care and affordable coverage for low-income individuals who would otherwise be eligible for coverage on the health insurance Marketplace. Minnesota and New York both implemented BHPs in 2015, and their BHPs currently cover 89,000 and 700,000 people, respectively. BHPs must cover the ACA’s essential health benefits, and both New York and Minnesota offer low to no cost-sharing.
Federal funding for BHPs is based on 95 percent of the total advance premium tax credits (APTCs) and cost-sharing reductions that would have been provided if a state’s BHP population would have enrolled in the second-lowest-cost silver qualified health plan (QHP) on the state’s health insurance Marketplace. The methodology for determining payment is published annually and is based on BHP enrollment characteristics for each state, including age, geographic area, household size, and income. Minnesota estimated that approximately 25 percent of the federal funding for its BHP came from cost-sharing reductions.
Major Changes to BHP Federal Financing
In October 2017, the Centers for Medicare and Medicaid Services (CMS) announced it would stop paying cost-sharing reductions to insurers, who remain legally obligated to pay for these same reductions to cover costs of deductibles, coinsurance, and co-payments for individuals at 100 to 250 percent FPL in states that did not expand Medicaid, and 138 to 250 percent FPL in Medicaid expansion states. Many insurers chose to offset the elimination of cost-sharing reduction by increasing premiums in order to secure higher premium tax credits for consumers.
State and Federal Responses
Minnesota and New York were notified that the CMS would stop funding the cost-sharing reductions of their BHPs in December 2017, and payments were subsequently halted in the first quarter of 2018. Both Minnesota and New York initially requested that CMS revise its calculations to account for a higher premium tax credit component of BHP payments to make up for the cost-sharing elimination. CMS did not initially respond, and the states moved to sue CMS.
CMS responded to the litigation by providing an interim settlement of $169 million to the states and establishing a new BHP payment methodology that provides an 18.8 percent adjustment to the BHP payment for both Minnesota and New York based on a survey of health insurers on the extent of their 2018 premium increase attributed to the discontinuation of cost-sharing reduction funding. Both Minnesota and New York questioned the revised BHP payment methodology. However, the new methodology currently only holds for 2018, and it is yet unknown if it will be used to calculate payments for 2019 and 2020.
Learn More
Read the full Health Affairs blog to learn more about the future of BHPs for Minnesota and New York.
Publication
Comparing Federal Government Surveys That Count the Uninsured: 2018
This brief provides an annual update to comparisons of uninsurance estimates from four federal surveys1:
- The American Community Survey (ACS)
- The Current Population Survey (CPS)
- The Medical Expenditure Panel Survey - Household Component (MEPS-HC)
- The National Health Interview Survey (NHIS)
In this brief, we present current and historical national estimates of uininsurance along with the most recent available state-level estimates from these surveys. We also discuss the main reasons for variation in the estimates across the different surveys.
1 Another federal survey that provides estimates of the uninsured is the Behavioral Risk Factor Surveillance System (BRFSS), which provides uninsurance estimates for the adult population 18 years and over nationally and among states. Details about the BRFSS are included in Appendix A of the brief, and estimates from the BRFSS are provided in Appendix B.
Blog & News
Employer-Sponsored Insurance, 2013-2017: Premiums Grow Faster, Deductibles Continue to Increase - Chartbook and State Fact Sheets
October 1, 2018:The nation’s attention has recently concentrated on health insurance coverage purchased through Affordable Care Act marketplaces, but it is important to remember that the majority of non-elderly Americans (51.6%) continue to get their health insurance coverage from an employer.[1] A new analysis from SHADAC uses data from the Medical Expenditure Panel Survey (MEPS) to highlight the experiences of private sector workers with employer-sponsored insurance (ESI) from 2013 through 2017 at the national level and within the states.
Key Findings
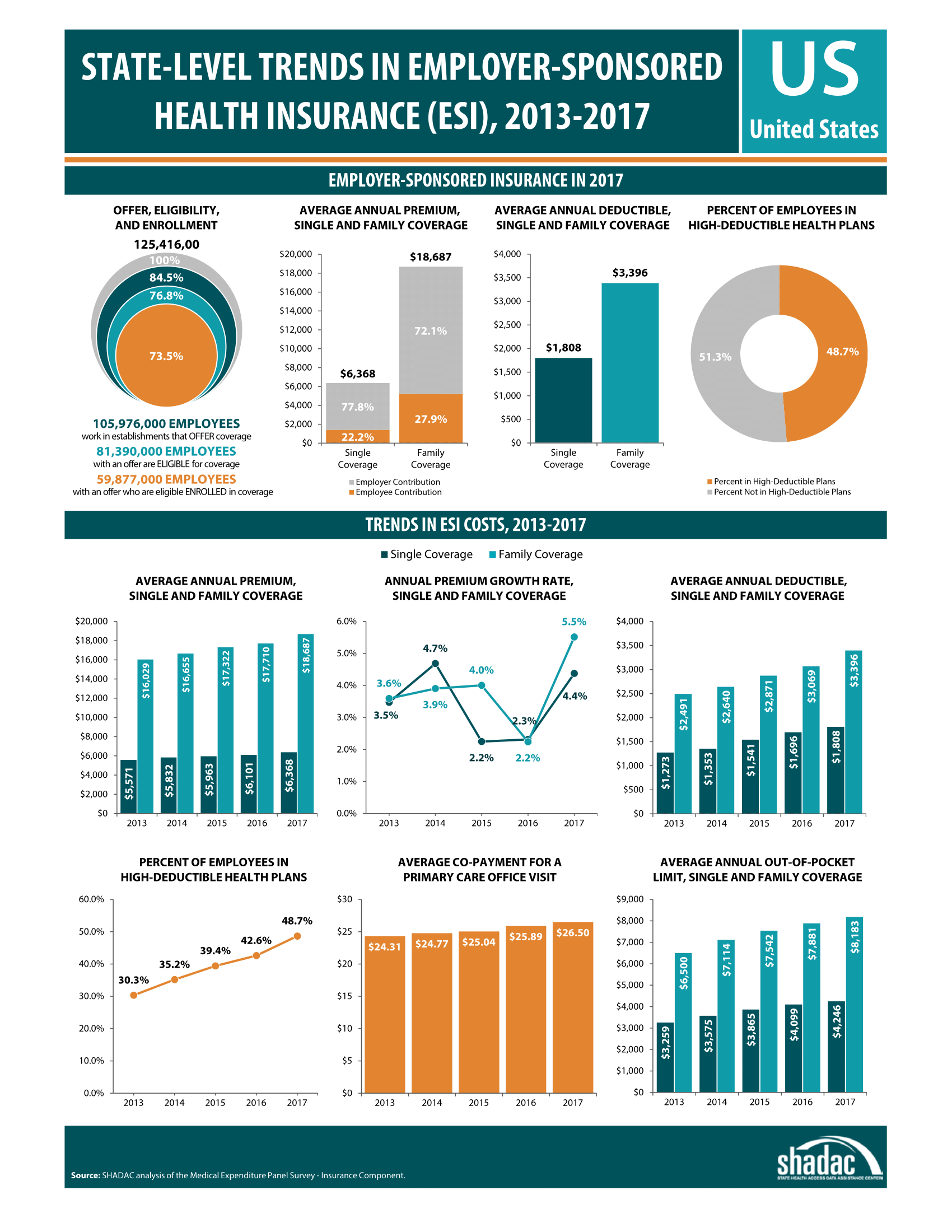 The percent of eligible U.S. employees receiving health coverage through ESI held steady in 2017, at 73.5 percent, representing nearly 60 million employees.
The percent of eligible U.S. employees receiving health coverage through ESI held steady in 2017, at 73.5 percent, representing nearly 60 million employees.- Nationwide, the percentage of employers offering health insurance coverage grew 3.5% to 46.9% from 2016 to 2017; however, there were no significant changes in the percent of employees that had an offer of coverage, the percent of employees that were eligible for coverage offered, or the percent of eligible employees that took up coverage.
- In 2017 the average annual single-coverage premium rose $267 to $6,368 nationwide. This marked a 4.4% increase from 2016--the highest annual growth rate for single-coverage premiums since 2014.
- The average annual family-coverage premium rose $977 to $18,687 in 2017. This was a 5.5% increase from 2016 and the highest annual rate of growth for family-coverage premiums in the last five years.
- The average annual single-coverage deductible nationwide rose $112 to $1,808 in 2017, a 6.6% increase from 2016.
- The average annual family-coverage deductible rose $327 to $3,396 in 2017, a 10.7% increase from 2016.
- In 2017, almost half of private-sector employees nationwide who had ESI (48.7%) were enrolled in a high-deductible health plan.[2] Enrollment in high-deductible health plans has been steadily rising and increased 14.2% between 2016 and 2017.
- The average annual out-of-pocket limit for single-coverage rose $147 to $4,246, a 3.6% increase from 2016.
- The average copayment for an office visit to a general practitioner rose $0.61 to $26.50, an increase of 2.4% from 2016; the average co-payment for a visit to a specialist rose $1.68 to $41.97, a 4.2% increase from 2016.
- State variation in access to and enrollment in ESI plans, along with variation in ESI premiums, deductibles, and cost-sharing, continued.
The Takeaway
Employer-sponsored insurance continues to be the backbone of the insurance coverage system in the United States, covering more than half the population. The level of financial protection offered by ESI has continued to decline steadily in the form of higher deductibles; however, for the first time in recent years this decrease in financial protection was accompanied by an acceleration of the growth in premiums. Given the dominant role of employer coverage in the broader coverage landscape, it is important to note that changes in the costs and value of employer coverage affect a significant number of people.
Explore the Analysis
The following products present findings from this analysis:
- Chartbook highlighting key findings on levels of, and trends in: average ESI premiums, deductibles, and employee cost sharing, as well as employee access to and take up of ESI coverage
- Two-page fact sheets on ESI for each state
- 50-state interactive map showing levels of, and changes in, average annual premiums for single-coverage in 2017, with links to state profile pages
- 50-state comparison tables
About the Data
This analysis uses data from the Medical Expenditure Panel Survey-Insurance Component (MEPS-IC).
Related Reading
New 2017 MEPS-IC Data: ESI Offer Rate Held Steady, but Premiums Continued to Rise and More Employees Enrolled in High Deductible Plans
SHADAC Blog
[1] SHADAC analysis of the 2016 American Community Survey (ACS) Public Use Microdata Sample Files.
[2] For the purposes of this analysis, high-deductible health plans are defined as plans that meet the minimum deductible amount required for Health Savings Account (HSA) eligibility ($1,300 for an individual and $2,600 for a family in 2017). This includes employees enrolled in single- and family-coverage plans.