Blog & News
2017 ACS: Uninsured Rate Increased Nationally and in 14 States (Infographic)
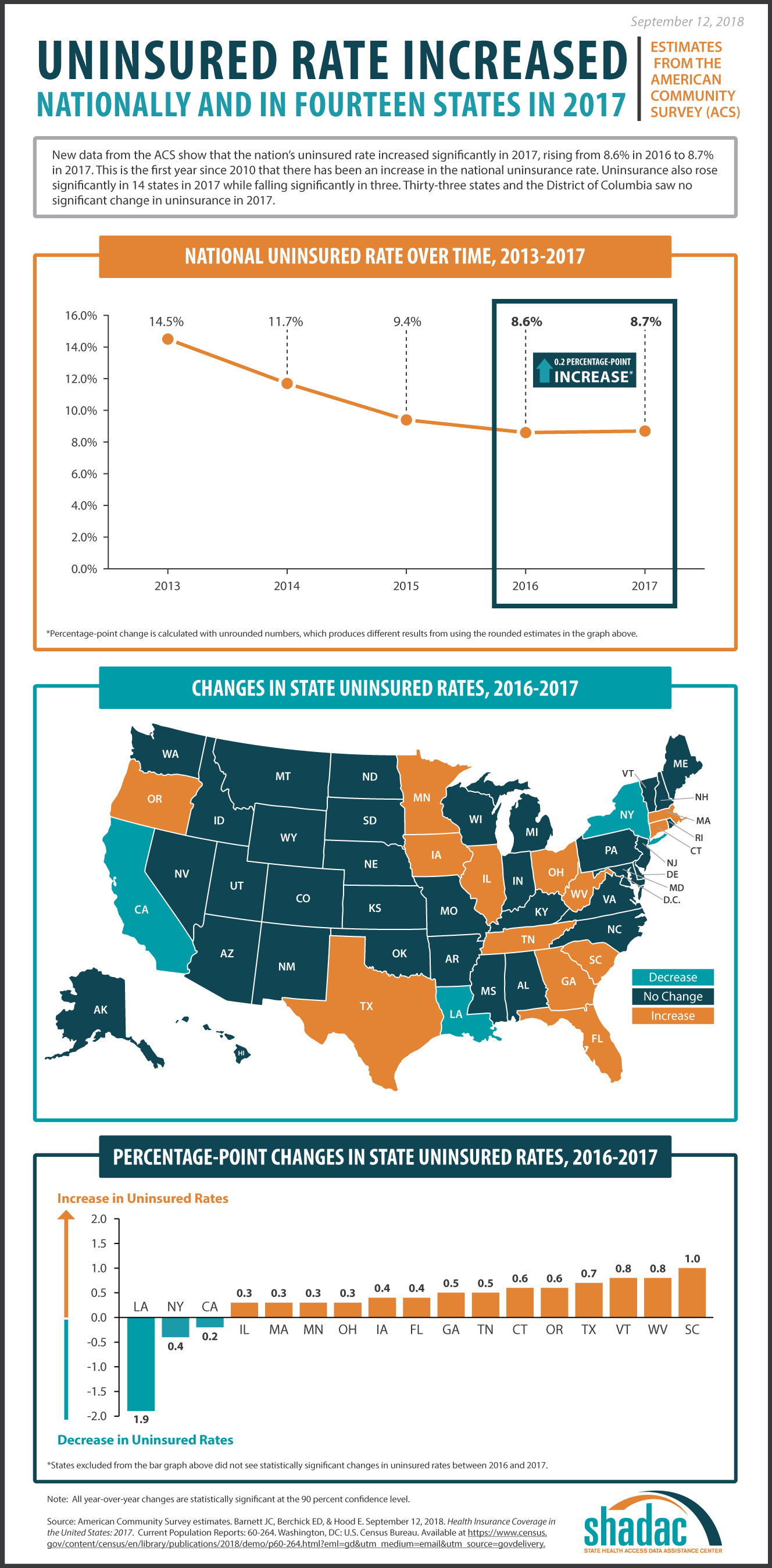
September 12, 2018:New health insurance coverage estimates from the American Community Survey (ACS) show that there was a statistically significant 0.2 percentage point increase in the national uninsured rate between 2016 and 2017. Uninsurance also increased in 14 states between 2016 and 2017, and decreased significantly in three states during the same period.
Uninsurance from 2016 to 2017
The national uninsurance rate increased from 8.6% in 2016 to 8.7% in 2017[1], with 715,000 more uninsured Americans in 2017. This is the first year since 2010 that there has been an increase in the national uninsurance rate.
Fourteen states saw significant increases in uninsurance from 2016 to 2017: Illinois, Massachusetts, Minnesota, Ohio, Florida, Iowa, Georgia, Tennessee, Oregon, Connecticut, Texas, Vermont, West Virginia, and South Carolina (Table 1). Among these states, South Carolina saw the largest percentage-point increase, at 1.0 percentage points, and Indiana, Massachusetts, Minnesota, and Ohio all experienced 0.3 percentage-point increases in uninsurance, tied for the smallest increases.
| Table 1. State Increases in Uninsurance, 2016-2017 | |||
|---|---|---|---|
| State | 2016 Percent Uninsured | 2017 Percent Uninsured | Percentage-Point Change, 2016-2017* |
| Illinois | 6.5 | 6.8 | 0.3 |
| Massachusetts | 2.5 | 2.8 | 0.3 |
| Minnesota | 4.1 | 4.4 | 0.3 |
| Ohio | 5.6 | 6.0 | 0.3 |
| Florida | 12.5 | 12.9 | 0.4 |
| Iowa | 4.3 | 4.7 | 0.4 |
| Georgia | 12.9 | 13.4 | 0.5 |
| Tennessee | 9.0 | 9.5 | 0.5 |
| Oregon | 6.2 | 6.8 | 0.6 |
| Connecticut | 4.9 | 5.5 | 0.6 |
| Texas | 16.6 | 17.3 | 0.7 |
| Vermont | 3.7 | 4.6 | 0.8 |
| West Virginia | 5.3 | 6.1 | 0.8 |
| South Carolina | 10.0 | 11.0 | 1.0 |
|
*Differences are calculated with unrounded numbers, which may produce different results from using the rounded values in the table. |
|||
Three states—California, Louisiana, and New York—experienced statistically significant decreases in uninsurance from 2016 to 2017. Of these states, Louisiana saw the largest percentage-point drop in uninsurance, from 10.3% to 8.4% (-1.9pp). New York experienced a drop in uninsurance from 6.1% in 2016 to 5.7% in 2017 (-0.4pp). California experienced a decrease in uninsurance from 7.3% in 2016 to 7.2% in 2017 (-0.2pp).
Uninsurance Levels in 2017
Texas continues to have the highest uninsurance rate in 2017 at 17.3%, an increase from 16.6% in 2016.
The lowest 2017 uninsurance rate was 2.8% in Massachusetts. This was an increase from 2016, when the state’s uninsurance rate was 2.5%.
Taken together, the uninsurance rate remained statistically unchanged in states that expanded Medicaid. The individual state uninsurance rates in these states ranged from a low of 2.8% in Massachusetts to a high of 13.7% in Alaska.
The uninsurance rate increased 0.4 percentage points overall in states that did not expand Medicaid. The individual state uninsurance rates ranged from a low of 5.4% in Wisconsin to a high of 17.3% in Texas.
Census Bureau Experts Will Share Insights during September 18th Webinar
On Tuesday, September 18th, SHADAC will host a webinar to examine the new 2017 ACS and CPS estimates, with technical insight provided by researchers from SHADAC and from the U.S. Census Bureau, which administers both surveys.
Speakers will discuss the new national and state estimates, and attendees will learn:
- When to use which estimates from which survey
- How to access the estimates via Census reports and American FactFinder
- How to access state-level estimates from the ACS using SHADAC tables
Attendees will have an opportunity to ask questions after the speaker presentations.
[1] The uninsurance estimates provided are rounded, while percentage-point changes are calculated using unrounded numbers; thus the national uninsured rate increased by 0.2 percentage points.
Blog & News
NHIS: 2018 Uninsured Rates Unchanged from 2017
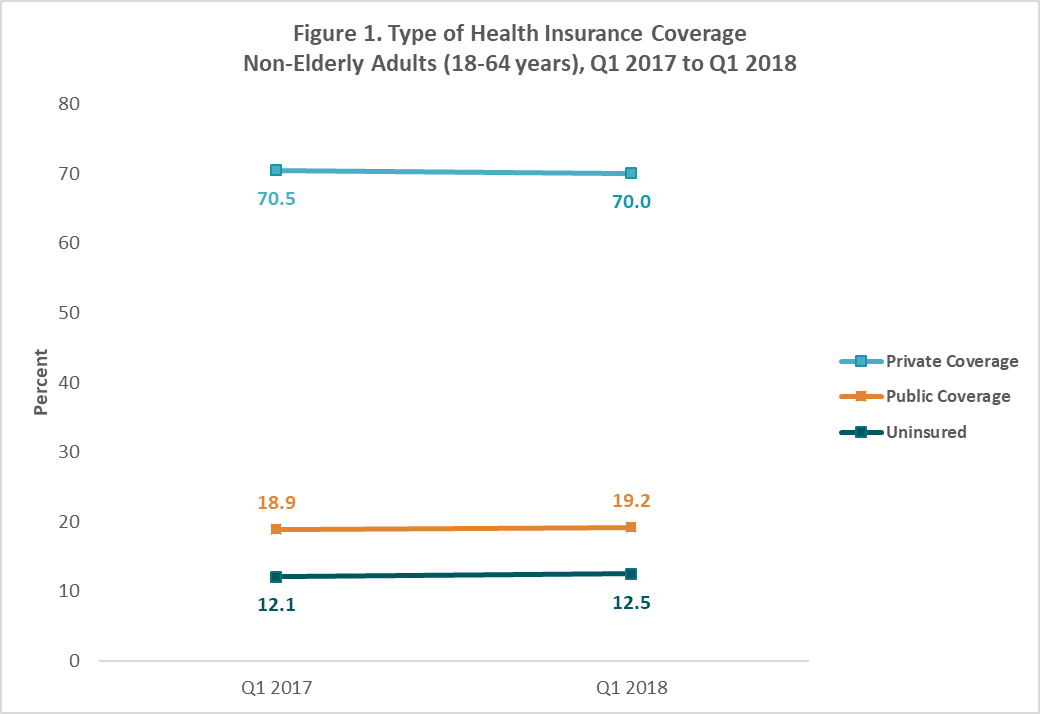
August 29, 2018:The National Center for Health Statistics (NCHS) released health insurance coverage estimates for Q1 2018 from the National Health Interview Survey (NHIS) as part of the NHIS Early Release Program. These are the first available full-year coverage estimates for 2018 from a federal survey. Nationwide, the uninsurance rate among non-elderly adults was 12.5% in the first quarter of 2018, statistically unchanged from 12.1% in the same period in 2017.
Uninsurance Remained Stable for Nearly All Groups in 2018
The new estimates show that uninsurance rates were statistically unchanged across age, race/ethnicity, and income groups from the first quarter of 2017 to the first quarter of 2018.
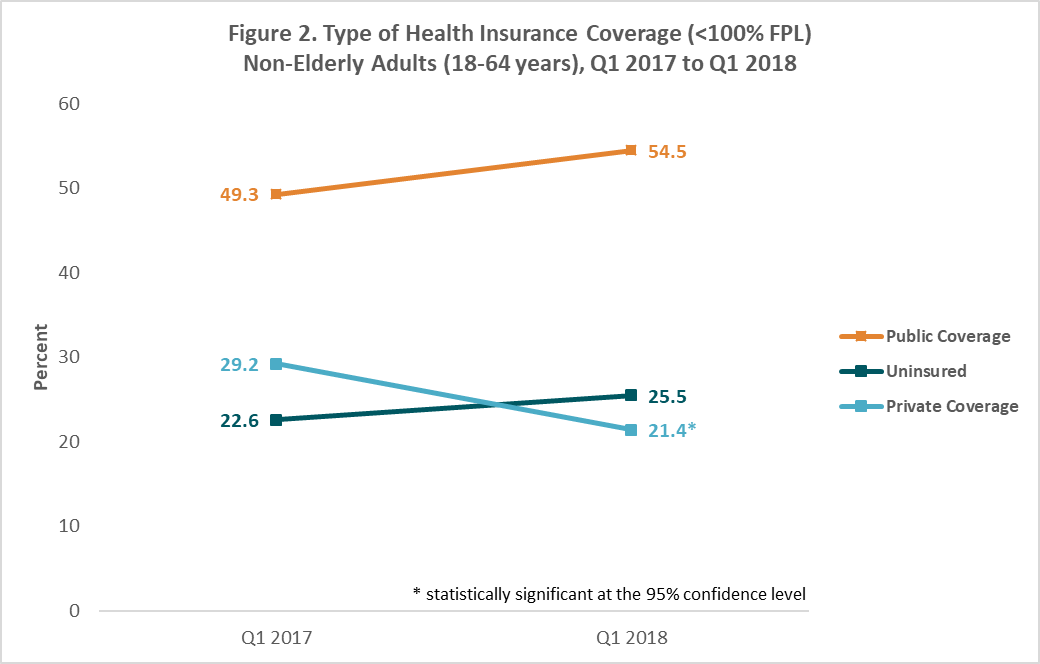
Decreases in Private Coverage among Non-Elderly Adults with Low Incomes
The rate of private coverage among non-elderly adults (ages 18-64) with incomes below 100% of the federal poverty level (FPL) decreased to 21.4% in Q1 2018 from 29.2% in Q1 2017. Rates of public coverage and uninsurance both increased among this group during the same period, though these changes were not statistically significant. No other income groups experienced significant changes in rates of private coverage, public coverage, or uninsurance during this period.
About the Numbers
The above estimates provide a point-in-time measure of health insurance coverage, indicating the percent of persons with that type of coverage at the time of the interview. The estimates are for the months of January to March 2018 and are based on a sample of 19,510 persons from the civilian noninstitutionalized population.
Differences described in this post are statistically significant at the 95% confidence level unless otherwise specified.
For more information about the early 2018 NHIS health insurance coverage estimates, read the National Center for Health Statistics brief.
Citation
Cohen, RA, Martinez, ME, & Zammitti, EP. August 29, 2018. “Health Insurance Coverage: Early Release Estimates from the National Health Interview Survey, January–March 2018.” National Center for Health Statistics: National Health Interview Survey Early Release Program. Available at https://www.cdc.gov/nchs/data/nhis/earlyrelease/Insur201808.pdf.
Blog & News
New 2017 MEPS-IC Data: ESI Offer Rate Held Steady, but Premiums Continued to Rise and More Employees Enrolled in High Deductible Plans
July 28, 2018:Though much attention has been paid to the individual health insurance market, a majority of Americans continue to get health insurance through an employer. Monitoring changes to employer-sponsored insurance (ESI) is critical to understanding Americans’ ability to access and afford health care.
The Agency for Healthcare Research and Quality (AHRQ) has released 2017 estimates from the Medical Expenditure Panel Survey – Insurance Component (MEPS-IC) on private sector employer-sponsored insurance (ESI) coverage, premiums, and deductibles. Highlights from the national tables are available in AHRQ Statistical Brief #513.
ESI offer rate remains stable
Nationally, the percent of employees working at establishments that offer coverage was statistically stable in 2017 at 84.5 percent (vs. 84.3 percent in 2016). Montana and Arizona were the only two states to experience statistically significant changes in the offer rate from 2016 to 2017: Montana’s offer rate increased from 66.2% to 73.2%, and Arizona’s increased from 83.5% to 87.4%. No state experienced a statistically significant decline in offer rates from 2016 to 2017.
ESI premiums continue to rise
At the national level, 2017 premiums for single-coverage ESI grew by 4.4 percent compared to 2016. This increase was larger than the 2.2 percent increase in premiums from 2015 to 2016. There was substantial state variation in the size of premium increases (Table 1). Fifteen states experienced statistically significant increases in premiums, 35 states (including D.C.) experienced no significant change in premiums, and Utah experienced a significant decrease.
| Table 1. States with Significant Changes in ESI Premiums, 2016-2016 (Single Coverage) | ||||
|---|---|---|---|---|
| State | 2016 ($) | 2017 ($) | Change ($) | Change (%) |
| Wyoming | 6,509 | 7,257 | 748 | 11.5% |
| New York | 6,614 | 7,309 | 695 | 10.5% |
| South Dakota | 5,881 | 6,533 | 652 | 11.1% |
| North Carolina | 5,717 | 6,348 | 631 | 11.0% |
| New Jersey | 6,492 | 7,074 | 582 | 9.0% |
| Alabama | 5,536 | 6,075 | 539 | 9.7% |
| Colorado | 5,972 | 6,456 | 484 | 8.1% |
| Michigan | 5,906 | 6,388 | 482 | 8.2% |
| Missouri | 5,881 | 6,354 | 473 | 8.0% |
| Connecticut | 6,545 | 7,012 | 467 | 7.1% |
| Tennessee | 5,543 | 6,006 | 463 | 8.4% |
| Oklahoma | 5,784 | 6,236 | 452 | 7.8% |
| Massachusetts | 6,621 | 7,031 | 410 | 6.2% |
| Rhode Island | 6,665 | 7,048 | 383 | 5.7% |
| Pennsylvania | 6,201 | 6,522 | 321 | 5.2% |
| Utah | 6,117 | 5,568 | -549 | -9.0% |
| United States | 6,101 | 6,368 | 267 | 4.4% |
| Source: Medical Expenditure Panel Survey - Insurance Component (MEPS-IC), Agency for Healthcare Research and Quality (AHRQ), Center for Financing, Access, and Cost Trends (CFACT). Notes: Estimates represent average annual premiums for single-coverage employer-sponsored insurance in nominal dollars. All changes are significant at the 95% confidence level. |
||||
More employees enrolled in high deductible plans
Nationally, the percent of employees enrolled in high deductible health plans (HDHP) increased to 48.7 percent in 2017 (from 42.6 percent in 2016). This increase in HDHP enrollment (6.1 percentage points) was larger than last-year’s change (3.2 percentage points). Six states and DC experienced significant increases in rates of HDHP enrollment (Table 2); no states experienced significant decreases in HDHP enrollment.
| Table 2. States with Significant Changes in Percent of Employees Enrolled in High Deductible Health Plans, 2016-2017 | |||
|---|---|---|---|
| State | 2016 (%) | 2017 (%) | Change (PP) |
| Florida | 39.9 | 61.9 | 22.0 |
| Utah | 43.7 | 62.8 | 19.1 |
| Vermont | 43.6 | 57.1 | 13.4 |
| Virginia | 36.5 | 46.7 | 10.2 |
| District of Columbia | 23.2 | 32.9 | 9.7 |
| California | 28.1 | 36.0 | 7.9 |
| Texas | 48.5 | 56.2 | 7.7 |
| United States | 42.6 | 48.7 | 6.1 |
| Source: Medical Expenditure Panel Survey - Insurance Component (MEPS-IC), Agency for Healthcare Research and Quality (AHRQ), Center for Financing, Access, and Cost Trends (CFACT). Notes: Estimates represent the percent of private-sector employees enrolled in high deductible health insurance plans. High-deductible health plans are defined as plans that meet the minimum deductible amount required for Health Savings Account (HSA) eligibility ($1,300 for an individual and $2,600 for a family in both periods). All changes are significant at the 95% confidence level. Changes are shown as percentage point changes. |
|||
Explore the Data: State Health Compare
SHADAC's State Health Compare has been updated to include 2017 MEPS-IC data. Visit State Health Compare to explore national and state-level MEPS-IC estimates for the years 2002 to 2017 for the following indicators:
- Workers in establishments that offer coverage
- Average annual ESI premium
- Employee contributions to premiums
- High deductible health plan enrollment (2012–2017)
Note: All changes described in this post are statistically significant at the 95 percent confidence level, unless otherwise noted.
Blog & News
Now Available: SHADAC Presentations from the 2018 AcademyHealth Annual Research Meeting
July 19, 2018:SHADAC presentation materials from the 2018 AcademyHealth Annual Research Meeting (ARM) are now available. Click on the presentation titles below to view and download the materials.
- “The Intersection of Structural Risk Factors and Insurance-Based Discrimination on Healthcare Access Inequities”
Presenter: Kathleen Call
Co-Authors: Rhonda Jones-Webb, Brooke Cunningham, Giovann Alarcón, Sarah Hagge, Alisha Simon - “Who Gets It Right? Characteristics Associated with Accurate Reports of Health Insurance Coverage”
Presenter: Kathleen Call
Co-Authors: Angela Fertig, Joanne Pascale, Don Oellerich - “Minnesota LTSS Projection Model: MN-LPM”
Presenter: Giovann Alarcón
Co-Authors: Robert Hest, Lynn A. Blewett - “Modeling Financial Eligibility for Medicaid Payment of LTSS”
Presenter: Robert Hest
Co-Authors: Giovann Alarcón, Lynn A. Blewett - “Modeling State-based Reinsurance: One Option for Stabilization of the Individual Market"
Presenter: Brett Fried
Co-Authors: Lynn A. Blewett, Coleman Drake - “Advancements in Care Coordination: Findings from an Evaluation of Minnesota’s State Innovation Model Initiative”
Presenter: Carrie Au-Yeung
Co-Authors: Christina Worrall, Donna Spencer, Emily Zylla, Kelli Johnson, Lacey Hartman - “Section 1115 Medicaid Expansion Waivers: Implementation Experiences of Arkansas, Indiana, Iowa, & Michigan”
Presenter: Carrie Au-Yeung
Co-Authors: Emily Zylla, Elizabeth Lukanen, Colin Planalp
Blog & News
SHARE Panel at 7th Annual ASHEcon
July 30, 2018:The 2018 Conference of the American Society of Health Conomists (ASHEcon) will take place from June 10th to June 13th at Emory University in Atlanta, with this year's theme being "Economics and Public Health."
An ASHEcon panel featuring findings from recent SHARE-funded research projects is scheduled for Monday, June 11th, from 10:00 a.m. to 11:30 a.m. in the Azalea Room of the Emory Conference Center Hotel. Panel details are below.
Panel: Medicaid Eligibility Thresholds and Minimum Wage Laws: The Impact of State Policy Decisions on Health Insurance Coverage, Out-of-Pocket Spending, and Access to Care
Chair: Andrew Mulcahy (RAND Corporation)
Paper: Medicaid vs. Marketplace Coverage for Near-Poor Adults: Effects on Out-of-Pocket Spending and Coverage
Presenting Author: Fredric Blavin (Urban Institute)
Discussant: Andrew Mulcahy (RAND Corporation)
Paper: The Impact of Changes in Medicaid Eligibility Thresholds on Duration of Health Insurance Coverage and Access to Health Care
Presenting Author: Heather Dahlen (University of Minnesota)
Discussant: Marguerite Burns (University of Wisconsin - Madison)
Paper: Do Minimum Wage Changes Affect Employer-Sponsored Insurance Coverage?
Presenting Author: Christine Eibner (RAND Corporation)
Discussant: Thomas Buchmueller (University of Michigan)