Blog & News
SHARE Panel at 7th Annual ASHEcon
July 30, 2018:The 2018 Conference of the American Society of Health Conomists (ASHEcon) will take place from June 10th to June 13th at Emory University in Atlanta, with this year's theme being "Economics and Public Health."
An ASHEcon panel featuring findings from recent SHARE-funded research projects is scheduled for Monday, June 11th, from 10:00 a.m. to 11:30 a.m. in the Azalea Room of the Emory Conference Center Hotel. Panel details are below.
Panel: Medicaid Eligibility Thresholds and Minimum Wage Laws: The Impact of State Policy Decisions on Health Insurance Coverage, Out-of-Pocket Spending, and Access to Care
Chair: Andrew Mulcahy (RAND Corporation)
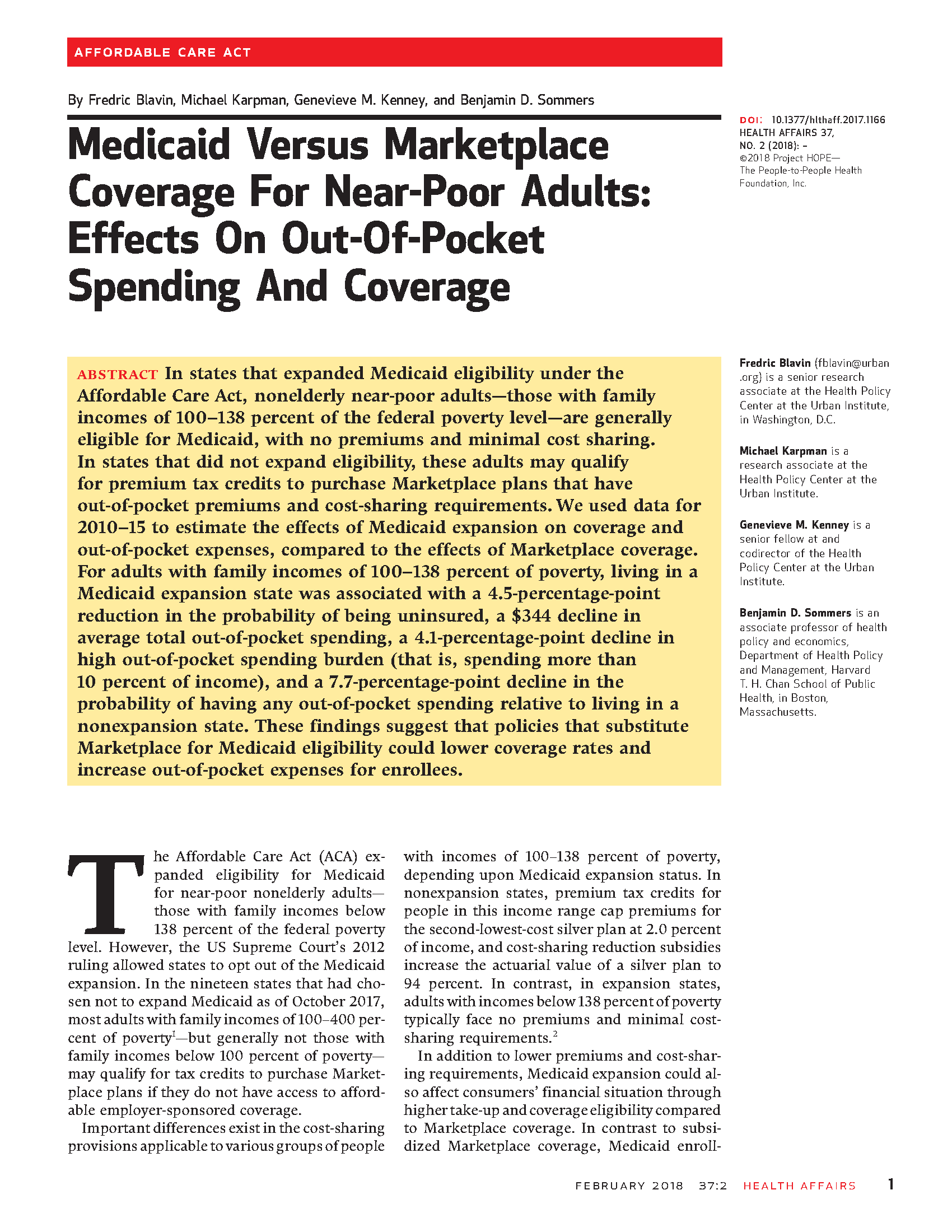
Paper: Medicaid vs. Marketplace Coverage for Near-Poor Adults: Effects on Out-of-Pocket Spending and Coverage
Presenting Author: Fredric Blavin (Urban Institute)
Discussant: Andrew Mulcahy (RAND Corporation)
Paper: The Impact of Changes in Medicaid Eligibility Thresholds on Duration of Health Insurance Coverage and Access to Health Care
Presenting Author: Heather Dahlen (University of Minnesota)
Discussant: Marguerite Burns (University of Wisconsin - Madison)
Paper: Do Minimum Wage Changes Affect Employer-Sponsored Insurance Coverage?
Presenting Author: Christine Eibner (RAND Corporation)
Discussant: Thomas Buchmueller (University of Michigan)
Blog & News
Fifty-State Analysis Finds Lower Access to Care among Adults with Less Education
March 2018:A new analysis from SHADAC examines educational attainment and access to health care, looking at the extent to which adults (25 years and older) with different levels of education skipped needed care due to cost and did not have a personal doctor. These indicators are both available for all states in SHADAC’s State Health Compare.
Skipping Needed Care Due to Cost
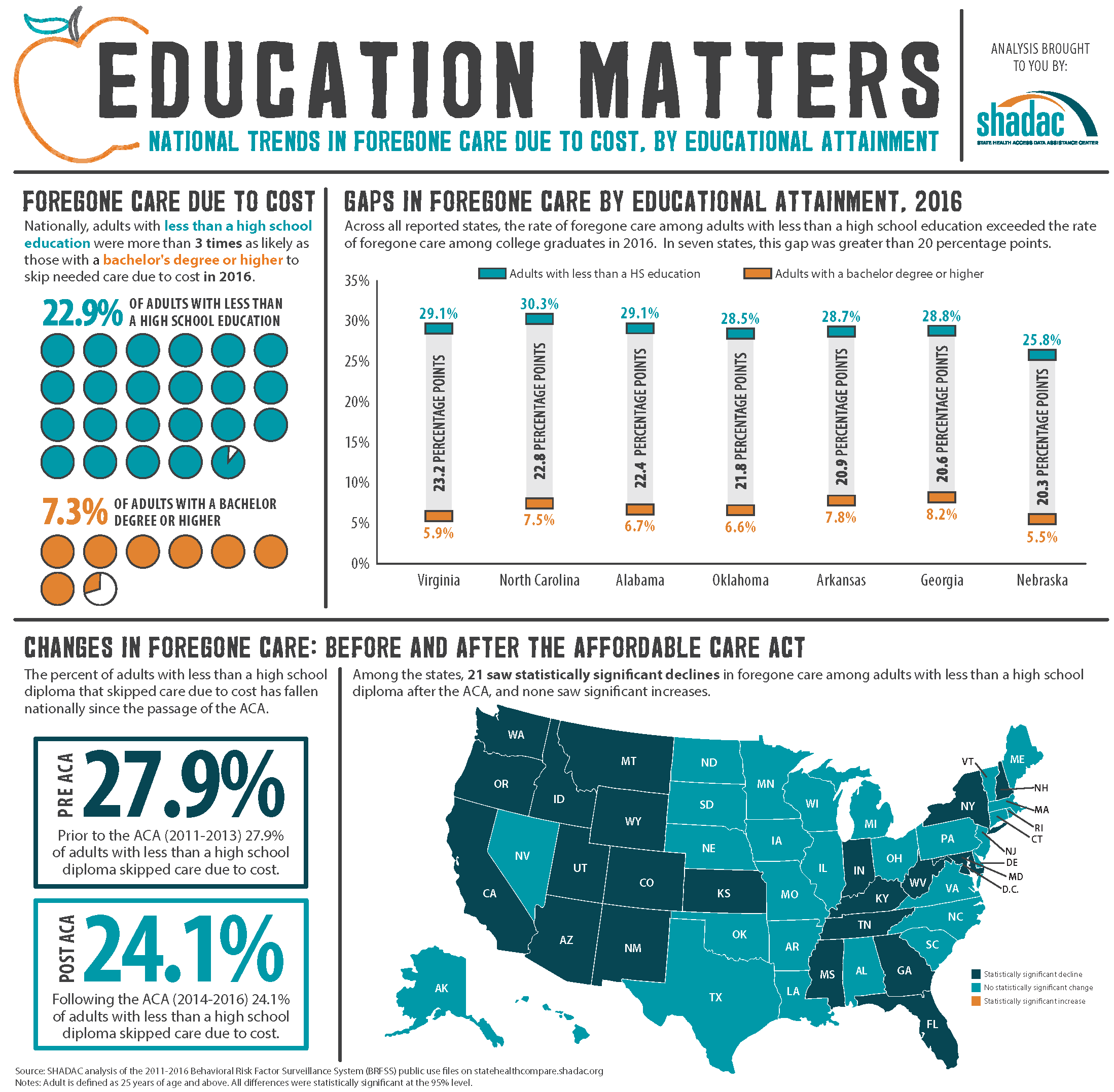 The analysis, which uses data from the Behavioral Risk Factor Surveillance System (BRFSS), found that people with less education are much more likely to skip needed medical care for financial reasons: Nationally, adults with less than a high school education were more than three times as likely to skip care due to cost in 2016 than were adults with a bachelor’s degree or higher (22.9% vs. 7.3%). Among the states, all but one (Alaska[1]) saw significantly higher rates of foregone care among adults with less than a high school diploma than among college graduates. In seven states, the rate of foregone care among adults with less than a high school education exceeded the rate of foregone care among college graduates by more than 20 percentage points: Virginia, North Carolina, Alabama, Oklahoma, Arkansas, Georgia, and Nebraska.
The analysis, which uses data from the Behavioral Risk Factor Surveillance System (BRFSS), found that people with less education are much more likely to skip needed medical care for financial reasons: Nationally, adults with less than a high school education were more than three times as likely to skip care due to cost in 2016 than were adults with a bachelor’s degree or higher (22.9% vs. 7.3%). Among the states, all but one (Alaska[1]) saw significantly higher rates of foregone care among adults with less than a high school diploma than among college graduates. In seven states, the rate of foregone care among adults with less than a high school education exceeded the rate of foregone care among college graduates by more than 20 percentage points: Virginia, North Carolina, Alabama, Oklahoma, Arkansas, Georgia, and Nebraska.
The percentage of these adults with less than a high school diploma that skipped care due to cost has fallen nationally since the passage of the ACA, from 27.9% in the years preceding the ACA (2011 to 2013) to 24.1% in the years following the ACA (2014 to 2016). Among the states, 21 saw statistically significant declines in skipped care after the ACA, and none saw a significant increase.
Not Having a Personal Doctor
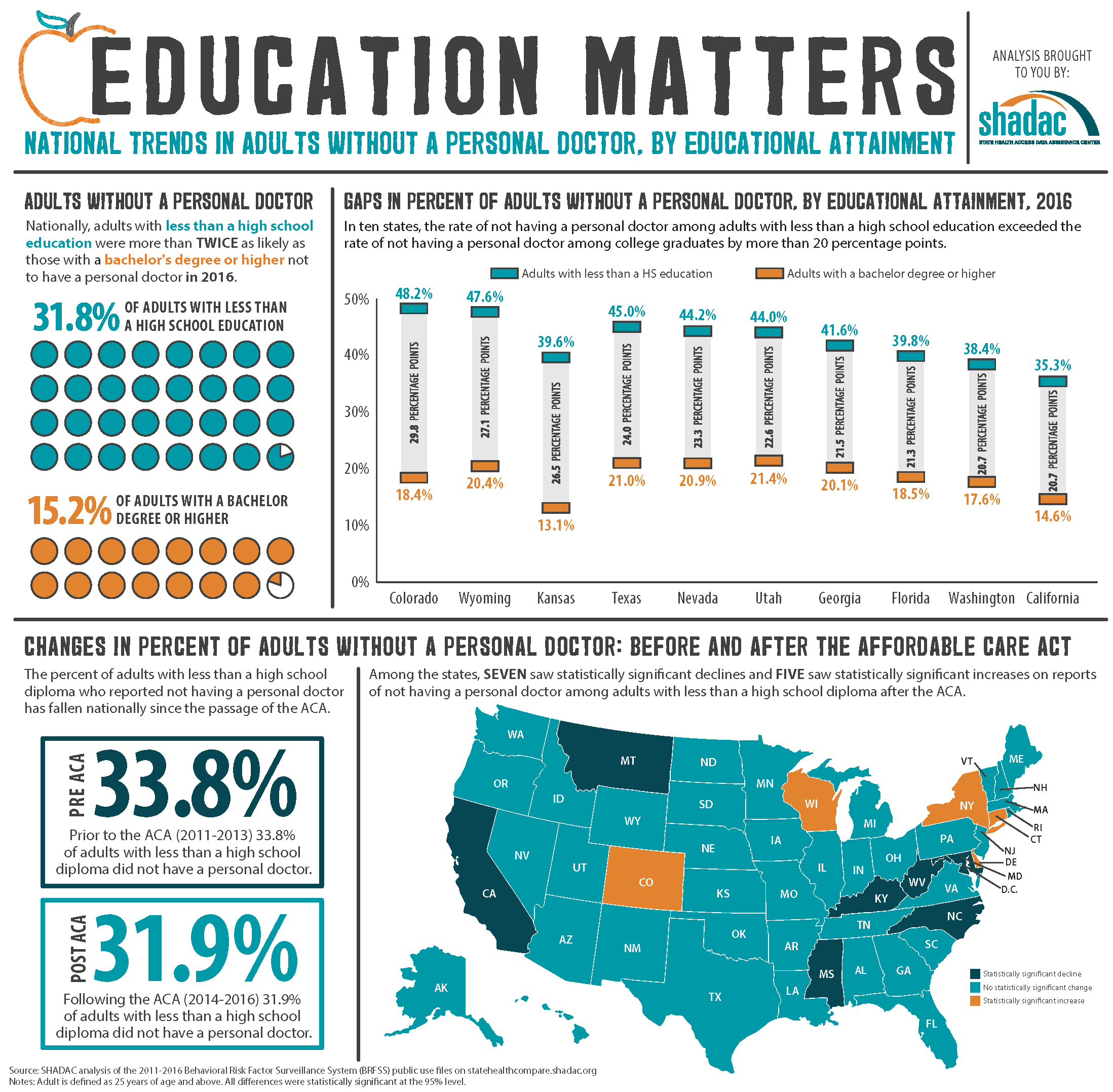 Nationwide, adults with less education were twice as likely to report that they did not have a personal doctor in 2016 as compared to people with a college degree or higher, at 31.8% vs. 15.2%. This same pattern was seen in 44 states. Among the remaining six states and the District of Columbia, no statistically significant differences were found between the two educational groups on reports of lacking a personal doctor. In ten states, the rate of not having a personal doctor among adults with less than a high school diploma exceeded the rate of not having a personal doctor among college graduates by more than 20 percentage points: Colorado, Wyoming, Kansas, Texas, Nevada, Utah, Georgia, Florida, Washington, and California.
Nationwide, adults with less education were twice as likely to report that they did not have a personal doctor in 2016 as compared to people with a college degree or higher, at 31.8% vs. 15.2%. This same pattern was seen in 44 states. Among the remaining six states and the District of Columbia, no statistically significant differences were found between the two educational groups on reports of lacking a personal doctor. In ten states, the rate of not having a personal doctor among adults with less than a high school diploma exceeded the rate of not having a personal doctor among college graduates by more than 20 percentage points: Colorado, Wyoming, Kansas, Texas, Nevada, Utah, Georgia, Florida, Washington, and California.
As with foregone care, the percentage of adults with less than a high school diploma who reported not having a personal doctor has fallen nationally since the enactment of the ACA, dropping from 33.8% to 31.9%. Significant declines on this measure were also seen in 7 states after the ACA went into effect, and 5 states saw significant increases.
States with More Adults Lacking a High School Diploma
Nationwide, 14.1% of adults had less than a high school diploma in 2016, and 16 states were above the national average on this measure. Texas, at 19.5%, had the highest percentage of adults with less than a high school diploma, followed by California (19.0%), Mississippi (18.0%), Louisiana (17.3%), and Kentucky (17.0%). North Dakota, New Hampshire, Wyoming, Montana, and Minnesota had the lowest percentages of residents with less than a high school education in 2016 (at 7.3%, 7.5%, 7.7%, 7.8%, and 7.9%, respectively).
State Fact Sheets
SHADAC researchers have created fact sheets for all states and the U.S. on the above measures. These fact sheets, along with infographics for select states, are available at www.shadac.org/Education&Access.
Learn More at State Health Compare
Learn more about the indicators used in this analysis, as well as other measures related to social determinants of health, at statehealthcompare.shadac.org.
[1] The 2016 estimate for this measure was suppressed for Alaska because the standard error is greater than 30% of the size of the estimate.
Publication
Section 1115 Medicaid Expansion Waivers: Implementation Experiences
This report summarizes SHADAC's analysis of how four states implemented Section 1115 Medicaid expansion wiavers. These states--Arkansas, Indiana, Iowa, and Michigan--are among eight that have expanded their Medicaid programs through Section 1115 of the Social Security Act rather than through the expansion option available under the Affordable Care Act (ACA).
 SHADAC's analysis was commissioned by the Medicaid and CHIP Payment and Access Commission (MACPAC) and sought to understan how Arkansas, Indiana, Iowa, and Michigan approached the implementation of key provisions of their Section 1115 Medicaid expansion waivers:
SHADAC's analysis was commissioned by the Medicaid and CHIP Payment and Access Commission (MACPAC) and sought to understan how Arkansas, Indiana, Iowa, and Michigan approached the implementation of key provisions of their Section 1115 Medicaid expansion waivers:
- Exchange plan premium assistance (Arkansas & Iowa)
- Enrollee contribution requirements (Iowa & Michigan)
- Health savings accounts (Arkansas & Indiana)
- Healthy behavior incentives (Indiana, Iowa, & Michigan)
- Graduated copayments for emergency department use (Indiana)
SHADAC researchers conducted interviews with 33 individuals representing current and former state agency staff and health insurance carriers in the four study states to identify the steps that states took to operationalize their programs. The report provides background information on the waiver program elements implemented in each of the four study states, summarizes the key pieces of administrative capacity that states put into place to implement their waivers, and details the specific program challenges they faced.
Blog & News
SHARE Results from Fred Blavin in Health Affairs: Among Near-Poor Adults, Access to Medicaid Reduced Out-of-Pocket Spending and Uninsurance
May 15, 2018:According to an article released today in Health Affairs, adults with incomes between 100 and 138 percent of the federal poverty level (FPL)—i.e., “near-poor” adults—saw lower out-of-pocket (OOP) costs and a reduced likelihood of being uninsured in states that expanded Medicaid than in non-expansion states.
Overview: Access to Medicaid among Near-Poor Adults
The analysis, which is based on a SHARE-funded study led by Dr. Fred Blavin (Urban Institute), used 2010 to 2015 data from the Current Population Survey (CPS) and the American Community Survey (ACS) along with state Medicaid expansion decisions as a natural experiment to estimate the impact of access to Medicaid on OOP health expenses and health insurance coverage, compared with access to subsidized Marketplace coverage. In states that chose not to expand Medicaid, near-poor adults may qualify for tax credits to purchase Marketplace plans that involve OOP premiums and cost-sharing; in expansion states, this population would generally face no premiums and minimal cost-sharing if they enrolled in Medicaid instead.
Key Findings: Out-of-Pocket Spending
Using OOP spending information from the CPS, Dr. Blavin and his co-authors found that Medicaid expansion, relative to Marketplace access, was associated with a $344 (33.9%) reduction in average total OOP spending, a $125 (23.0%) reduction in average OOP premium spending, and a $218 (46.4%) reduction in average OOP cost-sharing spending from 2010-2013 (before Medicaid expansion) to 2014-2015 (after Medicaid expansion). These decreases in average OOP spending were primarily driven by declines in the probability of having any OOP spending.
The $344 reduction in average total OOP spending from Medicaid expansion corresponds to 2 percent of annual income for adults in the 100 to 138 percent FPL range, and this is consistent with the amount that near-poor individuals would have to pay out-of-pocket for a Marketplace plan in a states that chose not to expand Medicaid. The authors note, however, that the impact of expansion for those who newly enrolled in Medicaid is likely to be higher, especially for those who had high OOP expenses prior to the ACA—e.g., high-cost uninsured adults and those with expensive employer plans.
| Related Resource: Webinar Recording and Slides | |
|---|---|
|
Dr. Blavin presented findings from this analysis during a SHARE webinar on December 5, 2017. The recording and transcript of this event, along with the presentation slides, are now available online. |
|
| Click here to access these materials. |
Key Findings: Coverage
Using coverage information from the ACS, the authors found that Medicaid expansion reduced the probability of being uninsured among near-poor adults by 4.5 percentage points between 2010-2013 and 2014-2015, compared to non-expansion states. This impact was driven by significant increases in Medicaid coverage that were partially offset by declines in ESI and direct purchase coverage.
According to the authors, these findings imply that more restrictive eligibility and enrollment policies, combined with higher premiums for Marketplace coverage relative to Medicaid, were associated with lower take-up rates among near-poor adults.
Read the full Health Affairs article.
Publication
Data Resources for Conducting Health Services and Policy Research
Blewett, LA, Call, KT, Turner J, & Hest, R. (2017). "Data Resources for Conducting Health Services and Policy Research." Annual Review of Public Health 39: 437-452. doi: 10.1146/annurev-publhealth-040617-013544
This article examines six federal household surveys that provide data inputs for monitoring the health and health care of the U.S. population and that are important for conducting helath services policy research: American Community Survey, Current Population Survey, National Health Interview Survey, Behavioral Risk Factor Surveillance System, Medical Expenditure Panel Survey, and Survey of Income and Program Participation.