Blog & News
SHADAC Comments on New Direction for Center for Medicare and Medicaid Innovation
December 07, 2017:On September 20, 2017, the federal Center for Medicare and Medicaid Innovation (Innovation Center) issued a request for stakeholder feedback on a proposed new direction for the Center, which is shifting its focus toward testing new models of patient-centered care that emphasize choice and competition.
| Innovation Center: Elements of Proposed New Direction | ||
|---|---|---|
|
Guiding Principles
|
Potential Models of Interest
|
|
The Innovation Center laid out a set of guiding principles for this shift as well as a list of potential models of interest (see text box).
Comments from SHADAC: Summary
Drawing on our experience providing evaluation services to states implementing innovative ways to deliver and pay for health care, SHADAC provided feedback to the Innovation Center. This feedback is summarized below.
Access the full text of SHADAC’s response.
Feedback: Guiding Principles
SHADAC commented on the principles of (a) transparent model design and evaluation and (b) small-scale testing.
Regarding transparency in model design and evaluation, we emphasized two key points:
- Successful model design should include planning and discussion of parameters for evaluation. Specifically, the information, data, and evidence needed to determine the impact of new models should be determined in advance, and data collection and evaluation requirements should be prioritized from the outset and revisited over time.
- Evaluations of innovations should include clear documentation of actual interventions to assess outcomes. Evaluations must determine how models are implemented in practice (versus planned interventions) in order to better associate interventions with changes in outcomes.
Regarding the principle of small-scale testing, SHADAC identified two considerations:
- The Innovation Center should focus on developing the capacity to monitor similar state-based models across states to inform intervention scalability. To this end, effort should be put toward developing measurement frameworks, standards for data collection, and metrics to respond to questions about the efficacy of reforms.
- Adequate funding should be provided to support state and local evaluations and to support the timely release of interim and final evaluation results in order to promote accountability and shared learning.
Feedback: Potential Models – State-based and Local Innovation, Including Medicaid-Focused Models
SHADAC identified two important lessons from our work with states implementing delivery system and payment reform that can inform future state-based models:
- Flexibility in model implementation must be balanced with participant accountability.
- It is important to determine and communicate the value (or return on investment) of payment reforms and to develop data collection systems to support this work.
Feedback: Opportunities and Challenges Associated with Potential Models
SHADAC also identified opportunities and challenges for states implementing payment and delivery system models.
The opportunities identified were (among others): accelerating progress and facilitating learning through access to external expertise; facilitating evaluation of market and payment reforms through APCD analytic work and development; and encouraging provider organization participation by promising data analytics during model design.
On the flipside, SHADAC identified the following challenges: performance measurement issues; the demand for more timely claims data and the integration of clinical data with administrative/claims data; data privacy legal issues; and limited capacity among provider organization for provider electronic data-sharing outside of their own organization walls.
Other Feedback: Dissemination of Evaluation Findings
SHADAC encouraged the Innovation Center to continue to support rapid-cycle feedback reporting from required state-led evaluations. We also noted that evaluation plans and interim findings could be more accessible to other states through Innovation Center website links and up-to-date inventories, infographics, or dashboards of evaluation and monitoring methods, activities, data sources, and results.
View the full text of SHADAC's response below or download the PDF here.
Blog & News
Now Available from State Health Compare: 2016 Data on Insurance Coverage, Medical Spending Burden, and Social Determinants of Health
December 04, 2017:SHADAC has updated six measures in State Health Compare to include estimates for 2016 for each state. The updated measures include:
- Health Insurance Coverage
- People with High Medical Care Cost Burden
- Unemployment Rate
- Income Inequality
- Adult Educational Attainment
- Children Considered to be Poor
State Health Compare provides a deep dive into the first measure, allowing users to explore insurance coverage status and type across a wide range of socioeconomic factors such as age, citizenship, education, income, health status, and race/ethnicity. State estimates for high medical spending and adult educational attainment are available by income and race/ethnicity; estimates of children in poverty are available by race/ethnicity; and unemployment and income inequality are available for states as a whole.
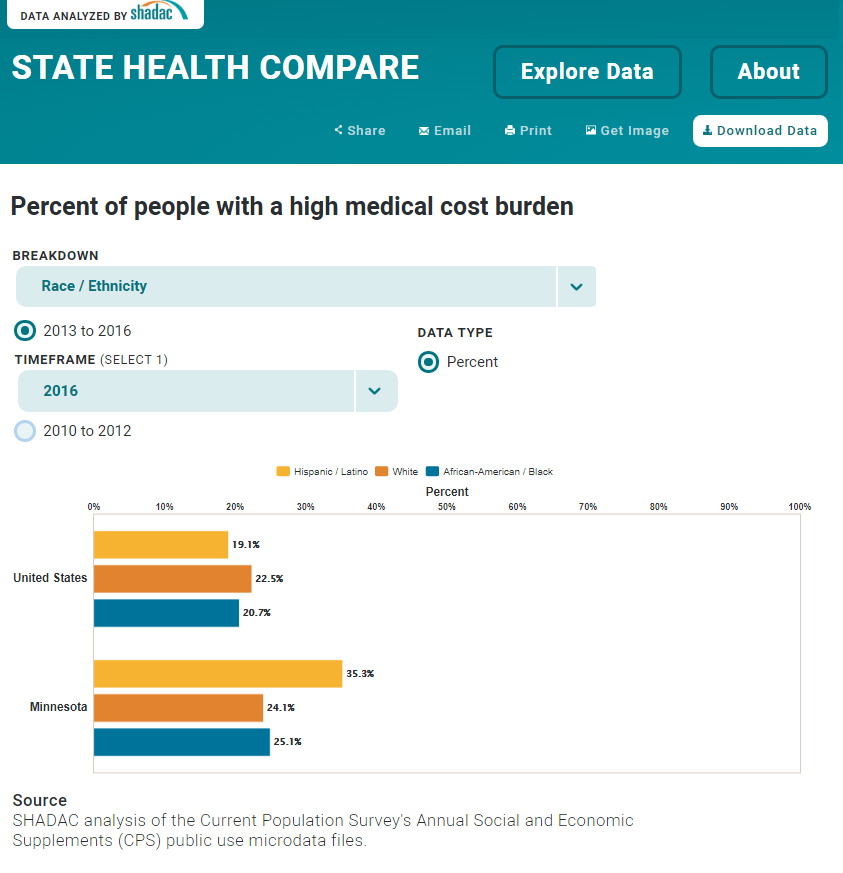
Data Highlight: High Out-of-Pocket Medical Spending in Minnesota in 2016
State Health Compare allows users to examine equity at the state level and between populations of interest. For example, when considering the proportion of people with a high medical care cost burden (i.e., family out-of-pocket medical spending exceeded 10% of annual income), Minnesota is a case where the data reveal important equity issues: 24.4% of all Minnesotans faced high medical spending in 2016. However, this number rose to 35.3% for the state’s Hispanic/Latino population. This percentage is significantly higher than that of the Minnesota’s white population, at 24.1%, and that of the Hispanic/Latino population nationwide, at 19.1%.1
Data Sources
The State Health Compare estimates for insurance coverage, income inequality, adult educational attainment, and children in poverty come from the American Community Survey (ACS). The estimates of medical costs come from the Current Population Survey (CPS), and the unemployment estimates are generated by the Bureau of Labor Statistics using the CPS.
| Significance Testing Using State Health Compare |
|---|
|
A recent SHADAC brief explains how to test for statistically significant differences between populations of interest using data from State Health Compare. The brief (1) explains how to conduct a quick visual scan of statistically significant differences using the State Health Compare’s margins of error output and (2) provides step-by-step instructions for using margins of error to conduct a more robust test of statistical significance through hypothesis testing. Access the brief. |
1 Differences are statistically significant at a 95% confidence level.
Blog & News
Employee Health Plans at Large Firms Paid for Smaller Portion of Medical Expenses in 2016 (Infographic)
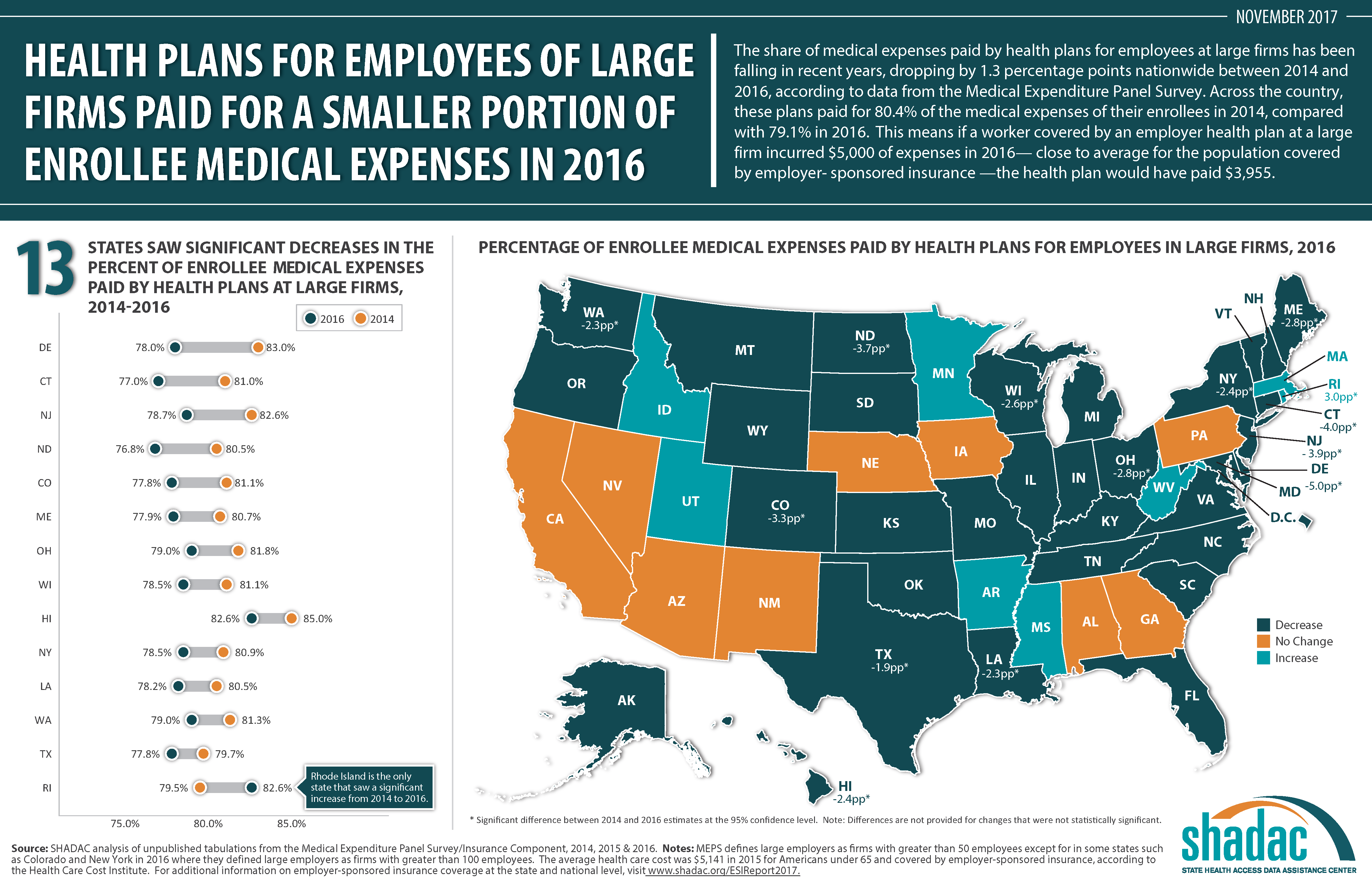
November 03, 2017:The share of medical expenses paid by health plans for employees at large firms has been falling in recent years, dropping by 1.3 percentage points nationwide between 2014 and 2016, according to data from the Medical Expenditure Panel Survey. Across the country, these plans paid for 80.4% of the medical expenses of their enrollees in 2014, compared with 79.1% in 2016.
This means if a worker covered by an employer health plan at a large firm incurred $5,000 of expenses in 2016—close to the average for the population covered by employer-sponsored insurance [1]—the health plan would have paid $3,955. (Text continues below infographic.)
THE STATE STORY
In all, 13 states saw significant decreases from 2014 to 2016:
- Delaware -5.0pp (83.0% to 78.0%)
- Connecticut -4.0pp (81.0% to 77.0%)
- New Jersey -3.9pp (82.6% to 78.7%)
- North Dakota -3.7pp (80.5% to 76.8%)
- Colorado -3.3pp (81.1% to 77.8%)
- Maine -2.8pp (80.7% to 77.9%)
- Ohio -2.8pp (81.8% to 79.0%)
- Wisconsin -2.6pp (81.1% to 78.5%)
- Hawaii -2.4pp (85.0% to 82.6%)
- New York -2.4pp (80.9% to 78.5%)
- Louisiana -2.3pp (80.5% to 78.2%)
- Washington -2.3pp (81.3% to 79.0%)
- Texas -1.9pp (79.7% to 77.8%)
Rhode Island is the only state that saw a significant increase in the percentage of medical expenses paid by health plans for employees at large firms, with a 3.0 percentage-point increase from 2014 to 2016 (from 79.5% to 82.5%).
In all, 36 states saw no significant change in the percentage of medical expenses paid by employer plans from 2014 to 2016.
Source: SHADAC analysis of unpublished tabulations from the Medical Expenditure Panel Survey/Insurance Component, 2014, 2015 & 2016.
*MEPS defines large employers as firms with greater than 50 employees except for in some states such as Colorado and New York in 2016 where they defined large employers as firms with greater than 100 employees.
For additional information on employer-sponsored insurance coverage at the state and national level, visit www.shadac.org/ESIReport2017.
[1] Health Care Cost Institute. November 2016. “2015 Health Care Cost and Utilization Report.” Available at http://www.healthcostinstitute.org/report/2015-health-care-cost-utilization-report/
Blog & News
New Resource: State Fact Sheets on Health Care Access and Utilization from 2011 to 2015
October 10, 2017:SHADAC has produced a new set of state fact sheets that examine key indicators of health care access and utilization from 2011 to 2015 using data from the National Health Interview Survey (NHIS).
The fact sheets are available for all 50 states and the District of Columbia and look at access and utilization indicators for the population as a whole and by age (0-18 years, 19-64 years, and 65+ years).
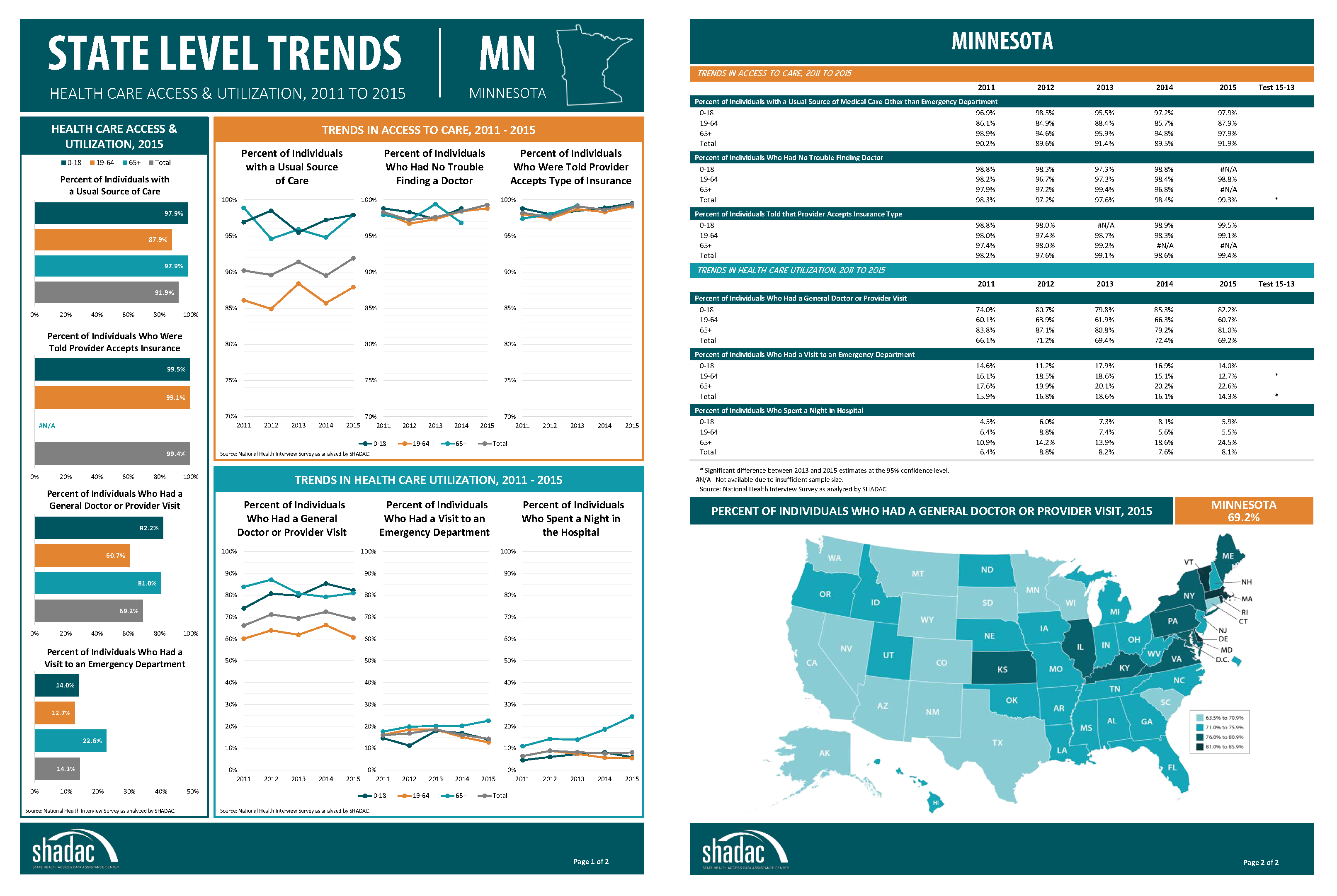 The analysis includes the following access to care indicators:
The analysis includes the following access to care indicators:
- Percent of individuals with a usual source of care
- Percent of individuals who had no trouble finding a doctor
- Percent of individuals who were told provider accepts insurance type
We include the following indicators of health care utilization:
- Percent of individuals who had a general doctor or provider visit
- Percent of individuals who had a visit to an emergency department
- Percent of individuals who spent a night in the hospital
Access the new state fact sheets.
Download a fact sheet for the entire United States.
Publication
State Trends in Health Care Access & Utilization, 2011-2015
These SHADAC state fact sheets highlight key indicators of health care access and utilization from 2011 to 2015 at the state level using data from the National Health Interview Survey (NHIS).
Estimates for the following indicators are provided for the population as a whole and by age (0-18, 19-64, 65+):
Access to Care
- Percent of individuals with a usual source of care
- Percent of individuals who had no trouble finding a doctor
- Percent of individuals who were told provider accepts insurance type
Health Care Utilization
- Percent of individuals who had a general doctor or provider visit
- Percent of individuals who had a visit to an emergency department
- Percent of individuals who spent a night in the hospital
Choose a state below to view and download its individual fact sheet.
Download a single file for all 50 states and the District of Columbia.
Download a fact sheet for the entire United States.