Blog & News
State Health Compare Data Highlight: Potentially Preventable Hospitalizations
May 29, 2019:More expensive than outpatient or primary care, hospitalization contributes substantially to healthcare costs, with hospital care accounting for 33% of healthcare spending, or $1.1 trillion, in 2017.[1] Reducing potentially preventable hospitalizations—i.e., hospital admissions for certain acute illnesses or chronic conditions that might not have required hospitalization if they had been better managed through outpatient primary care—is therefore a key mechanism by which healthcare costs can be reduced. National and state-level data on potentially preventable hospitalizations allow policymakers and analysts to track and monitor trends in this area, assess progress or setbacks, and consider policy levers that could effect change.
State Health Compare: A Unique Source of State-Level Estimates on Potentially Preventable Hospitalizations
SHADAC’s State Health Compare is the only publicly accessible source of state-level measures on potentially preventable hospitalizations, with three measures available: 1) per person cost of potentially preventable hospitalizations; 2) rates of potentially preventable adult hospitalizations; and 3) rates of potentially preventable child hospitalizations. These measures are available for 2009 through 2015 (the most recent year available).
About the Data
State Health Compare uses data from the Health Care Cost and Utilization Project (HCUP) to produce the above measures.[2] HCUP is a collection of national and state inpatient and emergency department databases that constitutes the largest available all-payer longitudinal hospital care data source. HCUP data are derived from hospital administrative discharge records originally used for hospital billing procedures.[3] State Health Compare’s national estimates were calculated using HCUP’s Nationwide Inpatient Sample (NIS), and state-specific results were calculated using HCUP’s State Inpatient Databases (SID) along with state inpatient databases purchased directly from states.
State Health Compare Highlights from 2015
- In 2015, per person costs of potentially preventable hospitalizations averaged $129 nationwide. Among the states, costs ranged from $70 per person in Colorado to $215 per person in the District of Columbia.
- The national average for potentially preventable hospitalizations per 100,000 adults was 1,520 in 2015, compared to a low of 867 in New Mexico and a high of 2,061 in the District of Columbia.
- The rate of potentially preventable hospitalizations per 100,000 children averaged 131 nationwide in 2015. Among the states, this rate ranged from 46 in Vermont to 260 in the District of Columbia.
Policy Implications
Data on potentially preventable hospitalizations can be used as evidence in support of multiple policy interventions. For example, these data point to the need for policies that would increase preventive service utilization as well as policies that would increase utilization of effective primary care–both strategies that are shown to reduce potentially preventable hospitalizations. [4],[5]
Explore potentially preventable hospitalizations on State Health Compare.
Related Reading
In 2016, SHADAC published a report on using HCUP data for State Health Policy Analysis, available here.
Agency for Healthcare Research and Quality. (2019). HCUP Overview, Healthcare Cost and Utilization Project (HCUP). Available at: https://www.hcup-us.ahrq.gov/overview.jsp
[1] Centers for Medicaid & Medicaid Services (CMS). National Health Expenditures 2017 Highlights [PDF File]. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/highlights.pdf
[2] SHADAC used the first three quarters of 2015 data for the 2015 estimates because HCUP switched from ICD-9 to ICD-10 coding in the fourth quarter of 2015. The next year of data will continue to use ICD-10 codes. When SHADAC publishes the 2016 HCUP data, we will indicate a break in series.
[3] There are some states where the data are not available (or not supplied to the Health Care Cost and Utilization Project) or for which data are suppressed because of reliability issues.
[4] “Introduction” in The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Yong, P.L., Saunders, R.S., Olsen, L.A., eds. National Academies Press (US), 2010. Available at: https://www.ncbi.nlm.nih.gov/books/NBK53914/
[5] Agency for Healthcare Research and Quality (AHRQ). Chartbook on Care Coordination: Potentially Avoidable Hospitalizations. Content last reviewed June 2018. Available at: https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/carecoordination/measure3.html
Publication
SHADAC Issue Brief "Aligning Quality Measures across Payers: Lessons from State Innovation Models"
In an effort to improve quality and contain the growing cost of health care, states are increasingly undertaking a shift away from fee-for-service reimbursement models that reward quantity and moving toward alternative payment models that reward value.
Many of the states leading the way in payment and delivery system reform have received State Innovation Model (SIM) awards from the Center for Medicare & Medicaid Innovation (CMMI) that have aided in accelerating that work.
An issue brief authored by SHADAC researcher Colin Planalp examines the work of five SIM states to develop common measure sets that align quality measures across private and public payers—a strategy aimed at reducing administrative burdens on providers and giving focus to quality improvement efforts. Drawing from the experiences of Connecticut, Massachusetts, Minnesota, Rhode Island, and Washington, the brief outlines a framework for other states to undertake quality measure alignment projects in the future.
This paper was produced by SHADAC with support from the CMMI. SHADAC is part of a team led by NORC at the University of Chicago that serves as the SIM Resource Support Contractor. SHADAC and other technical assistance partners support states and the Innovation Center in designing and testing multi-payer health system transformation approaches.
Strategy: Voluntary or Mandatory Alignment
One of the first key decisions made by states undertaking multipayer quality measure alignment is the choice between adopting a mandatory approach—requiring private payers to use the measure set—or voluntary alignment approach—encouraging stakeholder buy-in via engagement and needs prioritization. The issue brief examines both methods and highlights important considerations of each using examples of voluntary alignment from Connecticut and Washington, and examples of mandatory alignment (e.g., statutory and regulatory authorities) in Massachusetts, Minnesota, and Rhode Island.
Alignment Adoption Techniques
Each state referenced in the brief emphasized stakeholder engagement (i.e., establishing workgroups with representatives from state agencies, commercial health plans, health care providers, consumer advocates and other stakeholders) to ensure that the common measure sets met important priorities and to develop buy-in for adopting measures. The brief examines states’ stakeholder engagement strategies, as well as other techniques employed by the states to bolster their new common measure sets such as Washington’s adoption of the measures in its Medicaid and state employee health plans.
Measure Set Development: Priorities and Goals, Measure Evaluation, and Selection
The issue brief also lays out a roadmap for other states to develop their own common quality measure sets, pulling lessons from the processes employed by the five study states. The state workgroups tasked with selecting metrics for their common measure sets reported that their responsibilities generally entailed identifying and incorporating shared priorities and goals in selecting common measures, cataloguing measures currently in use within the state, selecting criteria for systematically evaluating potential measures, and evaluating and selecting measures according to those agreed-upon criteria.
Measure Set Sustainability
As a final step, the states profiled in this brief also have created and implemented processes to ensure their common measure sets will remain effective and relevant by periodically updating the measure sets by either removing measures where provider performance has topped out and/or adding new measures to address evolving quality priorities.
Lessons Learned
Ultimately, what conversations with these states revealed was a common set of lessons that can be utilized by other states planning to undertake quality measure alignment moving forward. Articulated at various points within the issue brief are recommendations for states to focus on:
- Including workgroup members from all stakeholder groups: commercial, public, state agencies, providers, consumers, and any other key groups.
- Encouraging stakeholder engagement in all aspects of selecting and implementing common measure sets.
- Strongly defining a rationale to promote stakeholder involvement, buy-in, and engagement.
- Selecting measures that are meaningful and practically applicable for providers and payers alike.
- Adopting a common measure set in public programs in order to promote mirrored alignment in commercial programs.
- Continuing to review measures after they have been set, and updating or modifying if necessary.
Read the full issue brief for more details on aligning quality measures in states.
Suggested Further Reading
Quality Measurement for HCBS and Behavioral Health in Medicaid: What’s Happening and What’s Missing
Blog & News
New SHADAC Issue Brief Highlights Lessons Learned from SIM States Working to Align Quality Measures
March 21, 2019:In an effort to improve quality and contain the growing cost of health care, states are increasingly undertaking a shift away from fee-for-service reimbursement models that reward quantity and moving toward alternative payment models that reward value.
Many of the states leading the way in payment and delivery system reform have received State Innovation Model (SIM) awards from the Center for Medicare & Medicaid Innovation (CMMI) that have aided in accelerating that work.
A new issue brief from SHADAC researcher Colin Planalp examines the work of five SIM states to develop common measure sets that align quality measures across private and public payers—a strategy aimed at reducing administrative burdens on providers and giving focus to quality improvement efforts. Drawing from the experiences of Connecticut, Massachusetts, Minnesota, Rhode Island, and Washington, the brief outlines a framework for other states to undertake quality measure alignment projects in the future.
This paper was produced by SHADAC with support from the CMMI. SHADAC is part of a team led by NORC at the University of Chicago that serves as the SIM Resource Support Contractor. SHADAC and other technical assistance partners support states and the Innovation Center in designing and testing multi-payer health system transformation approaches.
Strategy: Voluntary or Mandatory Alignment
One of the first key decisions made by states undertaking multipayer quality measure alignment is the choice between adopting a mandatory approach—requiring private payers to use the measure set—or voluntary alignment approach—encouraging stakeholder buy-in via engagement and needs prioritization. The issue brief examines both methods and highlights important considerations of each using examples of voluntary alignment from Connecticut and Washington, and examples of mandatory alignment (e.g., statutory and regulatory authorities) in Massachusetts, Minnesota, and Rhode Island.
Alignment Adoption Techniques
Each state referenced in the brief emphasized stakeholder engagement (i.e., establishing workgroups with representatives from state agencies, commercial health plans, health care providers, consumer advocates and other stakeholders) to ensure that the common measure sets met important priorities and to develop buy-in for adopting measures. The brief examines states’ stakeholder engagement strategies, as well as other techniques employed by the states to bolster their new common measure sets such as Washington’s adoption of the measures in its Medicaid and state employee health plans.
Measure Set Development: Priorities and Goals, Measure Evaluation, and Selection
The issue brief also lays out a roadmap for other states to develop their own common quality measure sets, pulling lessons from the processes employed by the five study states. The state workgroups tasked with selecting metrics for their common measure sets reported that their responsibilities generally entailed identifying and incorporating shared priorities and goals in selecting common measures, cataloguing measures currently in use within the state, selecting criteria for systematically evaluating potential measures, and evaluating and selecting measures according to those agreed-upon criteria.
Measure Set Sustainability
As a final step, the states profiled in this brief also have created and implemented processes to ensure their common measure sets will remain effective and relevant by periodically updating the measure sets by either removing measures where provider performance has topped out and/or adding new measures to address evolving quality priorities.
Lessons Learned
Ultimately, what conversations with these states revealed was a common set of lessons that can be utilized by other states planning to undertake quality measure alignment moving forward. Articulated at various points within the issue brief are recommendations for states to focus on:
- Including workgroup members from all stakeholder groups: commercial, public, state agencies, providers, consumers, and any other key groups.
- Encouraging stakeholder engagement in all aspects of selecting and implementing common measure sets.
- Strongly defining a rationale to promote stakeholder involvement, buy-in, and engagement.
- Selecting measures that are meaningful and practically applicable for providers and payers alike.
- Adopting a common measure set in public programs in order to promote mirrored alignment in commercial programs.
- Continuing to review measures after they have been set, and updating or modifying if necessary.
Read the full issue brief for more details on aligning quality measures in states.
Suggested Further Reading
Quality Measurement for HCBS and Behavioral Health in Medicaid: What’s Happening and What’s Missing
Blog & News
A State-level Measure of Drug Affordability on State Health Compare: Made Changes to Medical Drugs Because of Cost
February 25, 2019:Americans spend more on prescription medications per capita than residents of any other nation due to higher U.S. drug prices. In 2016, prescription drugs accounted for an estimated 14.1 percent of total national health care costs, or $471 billion. [1],[2] The high prices of prescription drugs have captured current national attention, with both the Trump Administration and congressional lawmakers proposing a number of solutions to the issue.
State Health Compare: Americans Are Making Changes to Their Medical Drugs Due to Cost
|
SHADAC’s State Health Compare measure “Made Changes to Medical Drugs” is produced using the National Health Interview Survey (NHIS), for which State Health Compare is the only source of state-level estimates, providing a unique way to see how the cost of prescriptions and other medical drugs affects Americans’ ability to afford these medications across and within states. |
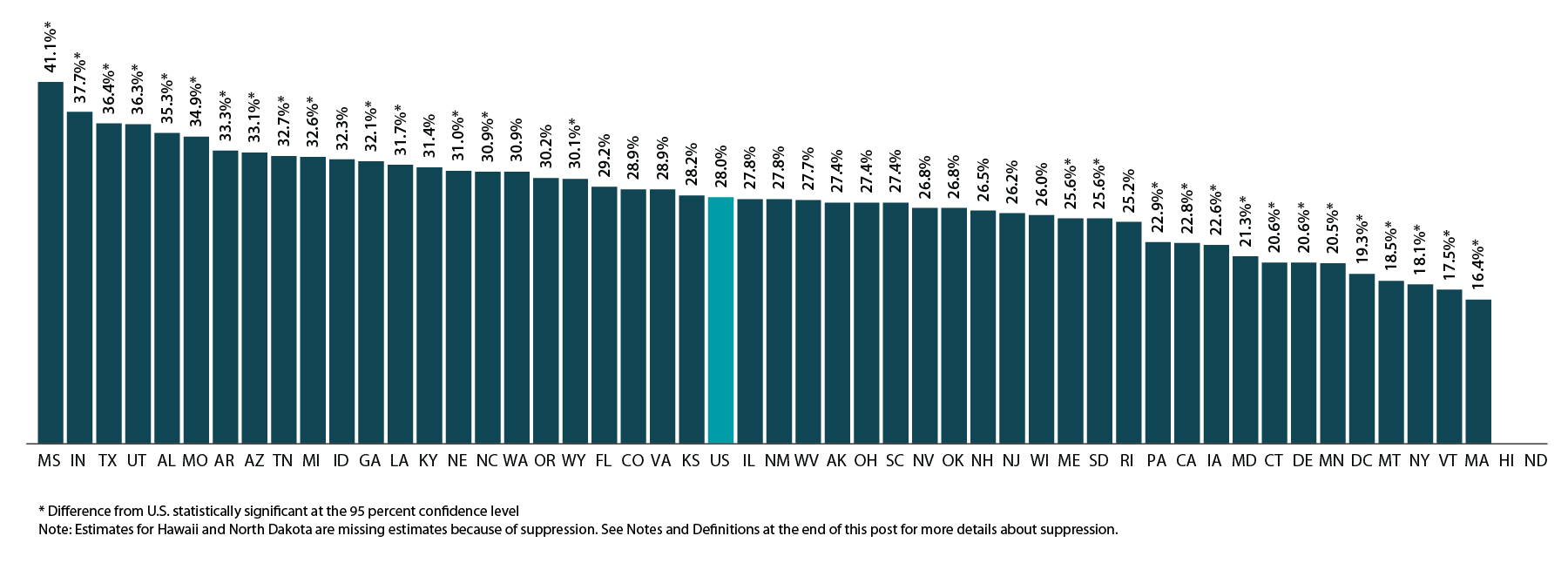
According to estimates from SHADAC’s State Health Compare, many Americans are making changes to their medical drugs in response to rising drug prices. In 2016, 28.0% of non-elderly adults (ages 19-64) said that due to cost they asked their doctor for cheaper medications, delayed refills, took less medication than prescribed, skipped doses, used alternative therapies, and/or bought medications out of the country.
The percentage of the U.S. population that made changes to drugs due to cost has been relatively stable over time at the national level, but there are substantial differences by state and significant disparities exist between age groups and types of insurance coverage.
MADE CHANGES TO MEDICAL DRUGS: HIGHLIGHTED ESTIMATES
There are significant differences by state in cost-related drug changes
As shown in the figure below, there is substantial state variation in the percent of non-elderly adults who report making changes to medical drugs due to cost, ranging from 16.4% in Massachusetts to 41.1% in Mississippi, a gap of 24.7 percentage points.
Percent of Non-elderly Adults Who Made Changes to Medical Drugs Because of Cost by State, 2016
Elderly adults were less likely to make changes to drugs due to cost
At the national level, elderly adults (age 65 and older) were less likely to report having made changes to their medical drugs due to cost relative to non-elderly adults (ages 18 to 64) at 22.7% vs. 28.0%, respectively. This difference may be related to the near-universal coverage of elderly adults through the Medicare program (though Medicare has limited drug coverage) compared to the relatively high rates of uninsurance among the non-elderly adult population. The discrepancy could also be due to differences in the resources that individuals in these two age groups have available to pay for drugs.
At the state level, there are large, statistically significant differences between elderly and non-elderly adults in the percentage of each group that made changes to medical drugs due to cost, as shown in the figure below. These differences range from a high of 13.1 percentage points in New Mexico (27.8% for those ages 19-64 vs. 14.7% for those ages 65+) to a low of 1.2 percentage points in Louisiana (31.7% for those ages 19-64 vs. 30.5% for those ages 65+) and Washington (30.9% for those ages 19-64 vs. 29.7% for those ages 65+).
Percent Who Made Changes to Medical Drugs Because of Cost by State and Age, 2016
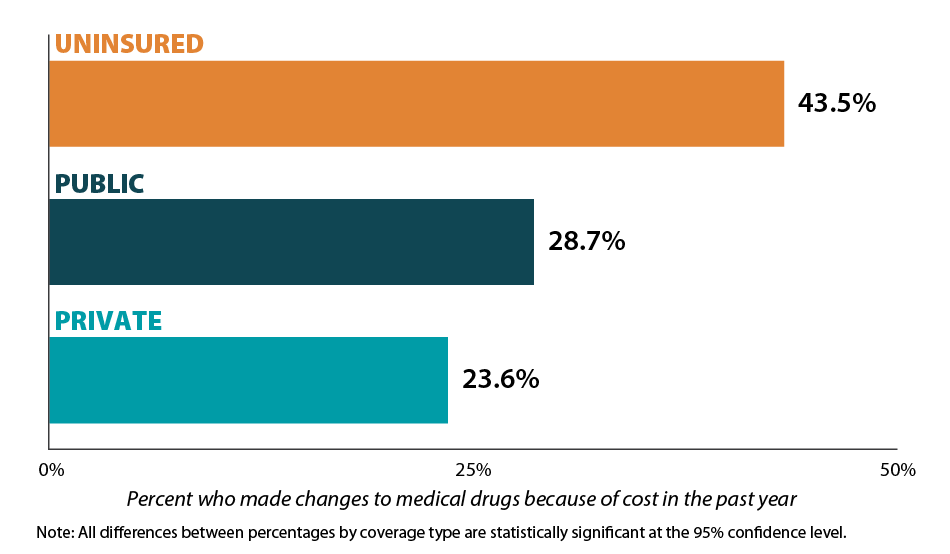
Those with health insurance are less likely to have made changes to drugs due to cost
Individuals with health insurance coverage were less likely to have made changes to medical drugs due to cost compared with uninsured individuals in 2016. At the national level, the share of the population that reported making changes to medical drugs due to cost was 23.6% for non-elderly adults with private coverage, 28.7% for non-elderly adults with public coverage, and 43.5% for non-elderly adults with no coverage. This represents a gap of 19.9 percentage points between private coverage and no coverage.[3]
Percent Who Made Changes to Medical Drugs Because of Cost by Coverage Type, 2016
Notes and Definitions
Made Changes to Medical Drugs is defined as the rate of individuals who made changes to medical drugs because of cost during the past twelve months by age for the civilian non-institutionalized population. This includes asking the doctor for cheaper medications, delaying refills, taking less medication than prescribed, skipping dosages, using alternative therapies, and/or buying medications out of the country.
The source of the estimates is SHADAC analysis of NHIS data, National Center for Health Statistics (NCHS). The NHIS sample is drawn from the Integrated Health Interview Survey (IHIS, MN Population Center and SHADAC). Data were analyzed at the University of Minnesota's Census Research Data Center because state identifiers were needed to produce results and these variables were restricted.
Estimates were created using the NHIS survey weights, which are calibrated to the total U.S. Civilian non-institutionalized population for estimates broken down by age, and to the civilian non-institutionalized population age 18 to 64 for estimates broken down by coverage type.
Though SHADAC goes to great effort to produce as many state-level estimates as possible for our measures, due to sample size restrictions many state estimates of this measure are suppressed when broken down by coverage type. Namely, estimates are suppressed if the number of sample cases was too small or the estimate had a relative standard error greater than 30 percent. Among those with private coverage, 46 state estimates are available; among those with public coverage, 7 state estimates are available; and among the uninsured, 2 state estimates are available.
Other State Health Compare estimates that use data from the NHIS
Made Changes to Medical Drugs is one of eight State Health Compare measures that SHADAC produces using data from the NHIS listed below. State Health Compare is the only source for state-level estimates of these measures.
- Made Changes to Medical Drugs
- Trouble Paying Medical Bills
- No Trouble Finding Doctor
- Told that Provider Accepts Insurance
- Had Usual Source of Medical Care
- Had General Doctor or Provider Visit
- Had Emergency Department Visit
- Spent the Night in a Hospital
[1] Roehing, C. May 2018. Projections of the Prescription Drug Share of National Health Expenditures Including Non-Retail. Altarum Report. Available at: https://altarum.org/sites/default/files/uploaded-publication-files/Projections_of_the_Prescription_Drug_Share_of_National_Health_Expenditures_June_2018.pdf
Blog & News
MACStats from MACPAC: 2018 Medicaid and CHIP Data Book Now Available
February 1, 2019: The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released the 2018 version of its Medicaid and CHIP Data Book. This data book is a collection of federal and state statistics regarding the Medicaid and CHIP programs that are compiled by MACPAC from multiple data sources on key topic areas including Medicaid and CHIP eligibility, enrollment, and expenditures, as well as beneficiary health, service use, and access to care. An excellent resource, the data book draws on a wide variety of data sources including Medicaid administrative data (e.g., CMS-64 data, MSIS data, Medicaid Managed Care enrollment reports, etc.) as well as federal survey data in order to compile policy relevant, but difficult to access, information about the Medicaid and CHIP programs into one comprehensive tool.
The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released the 2018 version of its Medicaid and CHIP Data Book. This data book is a collection of federal and state statistics regarding the Medicaid and CHIP programs that are compiled by MACPAC from multiple data sources on key topic areas including Medicaid and CHIP eligibility, enrollment, and expenditures, as well as beneficiary health, service use, and access to care. An excellent resource, the data book draws on a wide variety of data sources including Medicaid administrative data (e.g., CMS-64 data, MSIS data, Medicaid Managed Care enrollment reports, etc.) as well as federal survey data in order to compile policy relevant, but difficult to access, information about the Medicaid and CHIP programs into one comprehensive tool.
SHADAC is excited to be among the contractors that contributed to this product, providing MACPAC with estimates from the National Health Insurance Survey (NHIS) and the Medical Expenditure Panel Survey (MEPS) that highlight individual enrollment, primary source of insurance coverage, and service use and access to care with breakdowns available by age, demographics, and health characteristics. SHADAC produced these estimates using data for years 2016 and 2017, which are the latest available respectively for each survey.
For additional information on data methods and sources used in the data book, see MACPAC’s Technical Guide to MACStats, which provides supplementary information to help readers interpret the exhibits in the MACStats tables and figures as well as to understand the data sources and methods used.