Blog & News
Register Now: February 6th Webinar - Exploring Disparities Using SHADAC's State Health Compare
January 28, 2019:Exploring Disparities Using New and Updated Measures on SHADAC’s State Health Compare: State-Level Highlights for Unaffordable Rents, Unhealthy Days, and More
Date: February 6, 2019
Time: 1:00 p.m. – 2:00 p.m. Central
Register now.

Join us on Wednesday, February 6th at 1:00 PM Central for a webinar introducing two new measures of health outcomes and social determinants of health on SHADAC’s State Health Compare—Unhealthy Days and Unaffordable Rents. This presentation, hosted by SHADAC researchers Brett Fried and Robert Hest, will examine these new measures and highlight how the estimates can be used to explore disparities between states and among sub-populations.
 The webinar will also provide a virtual tour of some of the more than 40 state-level measures currently available on State Health Compare, highlighting recently updated data in particular. Mr. Fried and Mr. Hest will demonstrate how users can employ State Health Compare to easily create compelling maps, charts, and graphs, as well as download the raw estimates to perform deeper analyses and statistical testing.
The webinar will also provide a virtual tour of some of the more than 40 state-level measures currently available on State Health Compare, highlighting recently updated data in particular. Mr. Fried and Mr. Hest will demonstrate how users can employ State Health Compare to easily create compelling maps, charts, and graphs, as well as download the raw estimates to perform deeper analyses and statistical testing.
SHADAC researchers will answer questions from attendees after the presentation.
Adult Unhealthy Days: A New Measure on State Health Compare
SHADAC Blog
Housing Affordability Matters: Measuring and Addressing the Burden of Unaffordable Rents
SHADAC Blog
Examining Unaffordable Rents as a Social Determinant of Health
SHADAC Publication - Infographics
Significance Testing Using State Health Compare
SHADAC Brief
Blog & News
Now Available on State Health Compare: Updated Measures on Public Health, Health Outcomes, and Access, Cost, and Utilization of Care
December 12, 2018:SHADAC has updated eight data measures with the latest available estimates on our State Health Compare site. The updated measures include:
This measure indicates an individual state’s share of public health funding for the previous fiscal year. Data is available from 2005-2017, excepting in 2006 when data is not available.
This measure highlights the percent of people who made changes to their medical drugs due to cost in the past year. Breakdowns by age and coverage type are available for each state from 2011-2016.
This measure shows the percent of people who did not have trouble finding a doctor in the past year. The measure can be broken down by age and coverage type, and is now available from 2011 through 2016.
This measure captures the percent of persons who reported that their provider did accept their insurance type in the past year. The measure is available for 2011-2016 and can be broken down by age and coverage type as well.
Available for years 2011-2016, this measure counts the percent of people who had a usual source of medical care other than the emergency department (i.e., doctor’s office, clinic, health center, etc.) in the past year. Breakdowns by age and coverage type are also available.
This measure indicates the percent of adults who reported having a general doctor or provider visit in the past year. This measure can be broken down by age coverage type, and is available for all states from 2011 through 2016.
This measure, indicates the rates of individuals who reported a visit to the emergency department during the past twelve months for any reason and can be broken down by age and coverage type. Estimates are available from 2011-2016.
This measure denotes the rate of individuals who reported spending the night in a hospital at least once over the past year and can be broken down by age and coverage type. The measure is available from 2011-2016 for all states.
Explore these updated estimates on State Health Compare.
Data Sources
The State Health Compare estimates for public health funding come from Trust for America’s Health (TFAH) and all other measures regarding adults who made changes to medical drugs, had no trouble finding a doctor, are told that their provider accepts their insurance, had a usual source of medical care, had a general doctor or provider visit, had an emergency department visit, or spent the night in a hospital over the past year come from the National Health Interview Survey (NHIS).
Blog & News
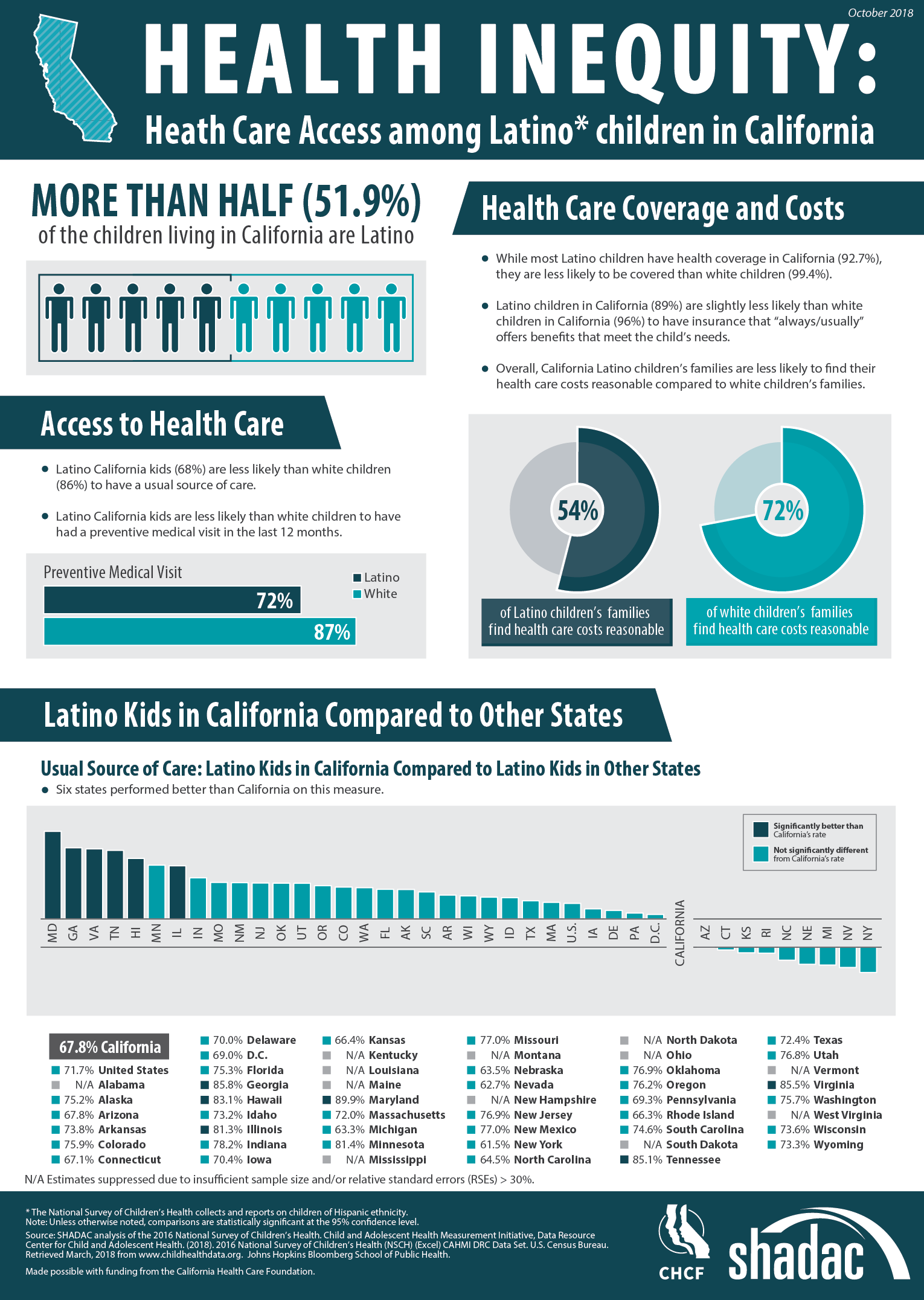
Latino Children in California Face Inequitable Access to Care (Infographic)
October 31, 2018:According to the 2016 National Survey of Children’s Health (NSCH), Latino children in California face lower access to health care than their white counterparts across multiple access indicators.
Despite representing more than half of children living in the state, Latino children are less likely than white children to: have health insurance coverage, have insurance benefits that meet their needs, find their health care costs reasonable, have a usual source of care, and have had a preventive medical visit in the last twelve months. The infographic presented here illustrates the 2016 NSCH estimates for these measures for both Latino and white children and also compares California’s performance to other states on the percentage of Latino children who have a usual source of care.
About the Data
The National Survey of Children’s Health is an annual survey funded and directed by the Health Resources and Services Administration (HRSA) Maternal and Child Health Bureau (MCHB). Learn more about the NSCH at www.childhealthdata.org.
Blog & News
Lynn Blewett in Health Affairs Blog: Examining the New Basic Health Plan Financing Rule
October 2018:On August 24th, the Centers for Medicare and Medicaid (CMS) released a Final Administrative Order that would revise and recalculate their payments toward Basic Health Programs (BHPs). Only two states have established BHPs—Minnesota and New York—under Section 1331 of the Affordable Care Act (ACA).
SHADAC Director Lynn Blewett and David Anderson, a researcher at the Duke University Margolis Center, co-authored a Health Affairs blog that takes a look at the background of BHPs in Minnesota and New York, how this new order affects them, and what may happen with federal BHP financing going forward.
BHP Background and Financing
BHPs are optional state coverage programs designed to improve continuity of care and affordable coverage for low-income individuals who would otherwise be eligible for coverage on the health insurance Marketplace. Minnesota and New York both implemented BHPs in 2015, and their BHPs currently cover 89,000 and 700,000 people, respectively. BHPs must cover the ACA’s essential health benefits, and both New York and Minnesota offer low to no cost-sharing.
Federal funding for BHPs is based on 95 percent of the total advance premium tax credits (APTCs) and cost-sharing reductions that would have been provided if a state’s BHP population would have enrolled in the second-lowest-cost silver qualified health plan (QHP) on the state’s health insurance Marketplace. The methodology for determining payment is published annually and is based on BHP enrollment characteristics for each state, including age, geographic area, household size, and income. Minnesota estimated that approximately 25 percent of the federal funding for its BHP came from cost-sharing reductions.
Major Changes to BHP Federal Financing
In October 2017, the Centers for Medicare and Medicaid Services (CMS) announced it would stop paying cost-sharing reductions to insurers, who remain legally obligated to pay for these same reductions to cover costs of deductibles, coinsurance, and co-payments for individuals at 100 to 250 percent FPL in states that did not expand Medicaid, and 138 to 250 percent FPL in Medicaid expansion states. Many insurers chose to offset the elimination of cost-sharing reduction by increasing premiums in order to secure higher premium tax credits for consumers.
State and Federal Responses
Minnesota and New York were notified that the CMS would stop funding the cost-sharing reductions of their BHPs in December 2017, and payments were subsequently halted in the first quarter of 2018. Both Minnesota and New York initially requested that CMS revise its calculations to account for a higher premium tax credit component of BHP payments to make up for the cost-sharing elimination. CMS did not initially respond, and the states moved to sue CMS.
CMS responded to the litigation by providing an interim settlement of $169 million to the states and establishing a new BHP payment methodology that provides an 18.8 percent adjustment to the BHP payment for both Minnesota and New York based on a survey of health insurers on the extent of their 2018 premium increase attributed to the discontinuation of cost-sharing reduction funding. Both Minnesota and New York questioned the revised BHP payment methodology. However, the new methodology currently only holds for 2018, and it is yet unknown if it will be used to calculate payments for 2019 and 2020.
Learn More
Read the full Health Affairs blog to learn more about the future of BHPs for Minnesota and New York.
Blog & News
Now Available: SHADAC Presentations from the 2018 AcademyHealth Annual Research Meeting
July 19, 2018:SHADAC presentation materials from the 2018 AcademyHealth Annual Research Meeting (ARM) are now available. Click on the presentation titles below to view and download the materials.
- “The Intersection of Structural Risk Factors and Insurance-Based Discrimination on Healthcare Access Inequities”
Presenter: Kathleen Call
Co-Authors: Rhonda Jones-Webb, Brooke Cunningham, Giovann Alarcón, Sarah Hagge, Alisha Simon - “Who Gets It Right? Characteristics Associated with Accurate Reports of Health Insurance Coverage”
Presenter: Kathleen Call
Co-Authors: Angela Fertig, Joanne Pascale, Don Oellerich - “Minnesota LTSS Projection Model: MN-LPM”
Presenter: Giovann Alarcón
Co-Authors: Robert Hest, Lynn A. Blewett - “Modeling Financial Eligibility for Medicaid Payment of LTSS”
Presenter: Robert Hest
Co-Authors: Giovann Alarcón, Lynn A. Blewett - “Modeling State-based Reinsurance: One Option for Stabilization of the Individual Market"
Presenter: Brett Fried
Co-Authors: Lynn A. Blewett, Coleman Drake - “Advancements in Care Coordination: Findings from an Evaluation of Minnesota’s State Innovation Model Initiative”
Presenter: Carrie Au-Yeung
Co-Authors: Christina Worrall, Donna Spencer, Emily Zylla, Kelli Johnson, Lacey Hartman - “Section 1115 Medicaid Expansion Waivers: Implementation Experiences of Arkansas, Indiana, Iowa, & Michigan”
Presenter: Carrie Au-Yeung
Co-Authors: Emily Zylla, Elizabeth Lukanen, Colin Planalp