Blog & News
To Improve Health Equity, Treat Disparities in Adverse Childhood Experiences
February 15, 2023:Twenty-five years ago, a watershed study on adverse childhood experiences (ACEs) first established a relationship between childhood trauma and long-term health impacts that can last well into adulthood.1 Since then, numerous related studies have corroborated the association between ACEs and mental health and substance use disorders as well as diseases such as cancer, diabetes, and heart disease.2
Today, many public health experts recognize childhood trauma as a public health threat, not so different from the threat posed by infectious diseases such as COVID-19. And, similar to the way that medical science has developed tools such as vaccines to prevent illness caused by pathogens, research has identified strategies that can prevent childhood trauma or provide children and families with tools to limit more lasting harms.3
As with other public health strategies, identifying populations most at risk for harm can help focus interventions to improve people’s health and lives. To do that for ACEs, it is critical to understand disparities in children’s exposure to traumatic experiences.
Disparities in ACEs exposure
In a recent SHADAC study, researchers used data from the federally sponsored National Survey of Children’s Health, which includes questions on several experiences generally considered to be ACEs, such as children’s separation from parents due to death, incarceration, or divorce; exposure to violence in the home or neighborhood; and difficulty affording basic necessities, such as food and housing. Because our aim was to produce estimates of ACEs exposure for different demographic groups, we combined multiple years of the survey (2016-2019) to enhance our ability to produce reliable estimates.
The findings of our analysis were deeply troubling. Nationally, almost half of U.S. children had exposure to at least one ACE, and more than half of children had an ACE exposure in 13 states. There was no state where ACEs were rare; even in Minnesota, the state with the lowest rate, more than one-third of children had exposure to at least one ACE.
Disparities in exposure to potentially traumatic childhood experiences were even larger across demographic groups than across the states. By race and ethnicity, Black children and American Indian and Alaska Native children had the highest rates of ACEs exposure, at 63.7 percent and 63.0 percent, respectively. Meanwhile, Asian children and White children had the lowest rates of ACEs exposure, at 25.0 percent and 40.9 percent, respectively. There were similarly large disparities by family income. Children from households with the lowest incomes (200 percent of Federal Poverty Guideline [FPG] or less) had an ACEs exposure rate of 61.9 percent, while those from families with the highest incomes (400 percent of FPG or higher) had a much lower rate of 26.4 percent. Our analysis also found differences by children’s health insurance coverage status and type, as well as by age groups.
ACEs as a health equity issue
Our study showed clear patterns of disparities in exposure to experiences that can create childhood trauma across a multitude of demographic groups—a finding that, in combination with research demonstrating a link between ACEs and long-term health, suggests that working to reduce the prevalence of ACEs and the harm that they cause could pay dividends in improving health equity.
Fortunately, there is a growing body of research that points to strategies for addressing ACEs. For instance, the U.S. Centers for Disease Control and Prevention (CDC) suggests strengthening economic supports for families and promoting family-friendly work policies; ensuring access to high quality childcare and early childhood education; and giving parents and children a toolbox of healthy skills for coping with short-term stress using social-emotional learning and other evidence-based approaches.4
Improving people’s health and lives by addressing the pernicious harm of ACEs will necessarily entail a broader “culture of health” strategy that extends beyond the traditional health care system. But attempting such new approaches may be necessary to break longstanding health equity logjams and provide all children a fair chance at growing into healthy and productive adults.
Download new SHADAC brief "The Kids Aren't Alright: Adverse Childhood Experiences and Implications for Health Equity."
1 Felitti, V.J. et al. (May 1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine, 14(4), P245-258. https://doi.org/10.1016/S0749-3797(98)00017-8
2 Centers for Disease Control and Prevention Vital Signs (2019). Adverse Childhood Experiences (ACEs) Preventing early trauma to improve adult health. https://www.cdc.gov/vitalsigns/aces/pdf/vs-1105-aces-H.pdf
3 Centers for Disease Control and Prevention (2019). Preventing Adverse Childhood Experiences: Leveraging the Best Available Evidence. https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf
4 Centers for Disease Control and Prevention (2019). Preventing Adverse Childhood Experiences: Leveraging the Best Available Evidence. https://www.cdc.gov/violenceprevention/pdf/preventingACES.pdf
Publication
The Kids Aren't Alright: Adverse Childhood Experiences and Implications for Health Equity
Authors: Colin Planalp, MPA and Andrea Stewart, MA
 Drawing on data from the National Survey of Children’s Health, this brief investigates the prevalence of adverse childhood experiences (ACEs) and disparities in ACEs exposure by children’s race, family income, age and health insurance coverage. The disproportionate impact of ACEs has deep ramifications on health equity due to related research showing that ACEs exposure is associated with increased risk for numerous short- and long-term health impacts, varying from mental health and substance use disorders to heart disease and cancer.
Drawing on data from the National Survey of Children’s Health, this brief investigates the prevalence of adverse childhood experiences (ACEs) and disparities in ACEs exposure by children’s race, family income, age and health insurance coverage. The disproportionate impact of ACEs has deep ramifications on health equity due to related research showing that ACEs exposure is associated with increased risk for numerous short- and long-term health impacts, varying from mental health and substance use disorders to heart disease and cancer.
To learn more about disparities in ACEs:
- Download State-level data tables of ACEs prevalence by race and ethnicity, family income, age, and health insurance coverage status;
- Check out the accompanying SHADAC blog "To Improve Health Equity, Treat Disparities in Adverse Childhood Experiences"; or
- Visit the Adverse Childhood Experiences measure on State Health Compare.
Blog & News
Navigating Data on State Health Compare (Video)
January 2023:
Check out our new video to learn tips and tricks for using SHADAC’s State Health Compare |
SHADAC’s State Health Compare is a go-to resource for more than 45 data measures on a range of health topics including insurance coverage; cost of care; health behaviors; health outcomes; access to and utilization of care; care quality; public health; and social and economic determinants of health. Estimates are regularly updated from more than 17 data sources and can be broken down across subcategories such as age, education level, race/ethnicity, and other characteristics.
This new video walks through how to create customized data sets and visualizations of state-level health estimates on State Health Compare, allowing analysts, policymakers, and other data users to seamlessly view and download their state’s estimates.
Additional Resources
The SHADAC website is home to numerous blogs detailing ways to use State Health Compare data. Take a deep dive on data related to excessive alcohol use, explore state-level public health funding, observe trends within the opioid epidemic, learn more about physician acceptance of Medicaid patients, or understand rates of unhealthy days for U.S. adults.
Blog & News
Neighborhood Support Matters for Child Health
November 22, 2022:Where people live, work, and play has been shown to have important impacts on health. In addition to one’s physical environment (e.g., access to safe schools, parks, and sources of nutritious food), the extent to which people feel connected to a supportive community with a network of resources is an important factor for health. This concept is known as “social capital," and has been linked with a broad range of health outcomes including mortality.
Neighborhood support is a form of social capital that can be measured with available survey data. The National Survey of Children’s Health (NSCH) is nationally representative and includes children (age 0-17) in all 50 states and the District of Columbia. The data from this survey provide information on family perceptions of neighborhood support and a broad range of child sociodemographic and health characteristics. NSCH data also allow researchers to study the association between supportive neighborhoods and key children’s health outcomes.
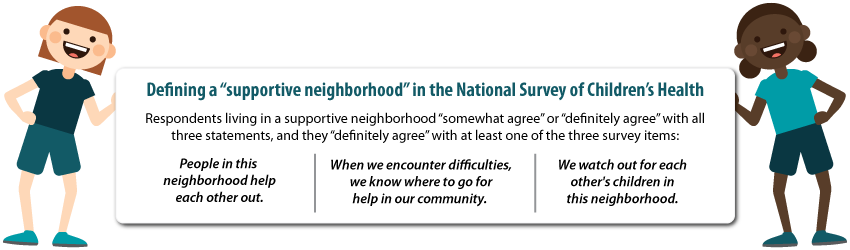
Only about half (55%) of children lived in a supportive neighborhood. As shown in the figure below, the likelihood of living in a supportive neighborhood also varied across population subgroups. Perceived neighborhood support was less likely for non-English households, children of color, children with special health care needs (CSHCN), families with less education or income, and children with public health insurance coverage or who were uninsured.
Percent of children living in supportive neighborhoods, by child characteristics
Source: SHADAC analysis of the National Survey of Children’s Health, 2018-2019
We found that neighborhood support matters for a child’s health. Family perceptions of neighborhood support were significantly associated with four of the five outcomes we examined, after adjusting for child characteristics. Children in supportive neighborhoods were less likely to have a past year emergency department visit or unmet care needs and were more likely to have a preventive dental visit and better parent-reported oral health status (Table below).
| Past year ED visit odds ratio | Unmet health needs odds ratio | Preventive dental visit odds ratio | Fair/poor health odds ratio | Fair/poor oral health odds ratio | |
| Neighborhood support | 0.89* | 0.52*** | 1.16** | 0.72 | 0.65*** |
Notes: *** p<0.001, ** p<0.01, * p<0.05 Unmet health care needs included medical, dental, hearing, vision, or mental health needs. All models were adjusted for demographic characteristics (age, sex, race/ethnicity, household language, income, parental education), children with special healthcare needs (based on a five-item screener), health insurance coverage, and a composite measure of family resilience. Resilience was defined by how families face problems, with ‘all of the time’ or ‘most of the time’ responses to four items: talk together, work together, draw on strengths, stay hopeful.
Our study provides evidence that neighborhood cohesion is correlated with better child health outcomes. Policies that support healthy neighborhoods and build social capital are essential for the wellbeing of children. This includes policies that benefit child development, such as neighborhood schools, playgrounds, and early childhood education. Community-based programs and health care also play a role in fostering neighborhood support by strengthening networks and linking community members to needed care and resources.
NSCH dataset provided by the Data Resource Center:
Child and Adolescent Health Measurement Initiative. 2018-2019 National Survey of Children’s Health (NSCH) Stata Constructed DataSet. Data Resource Center for Child and Adolescent Health supported by Cooperative Agreement U59MC27866 from the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Retrieved from www.childhealthdata.org.
Blog & News
Charting Two Decades of the Evolving Opioid Crisis
November 18, 2022:
In more than 20 years, the overdose crisis has shifted and grown from prescription opioids to a range of illicitly trafficked drugs |
Just over a decade after the U.S. Centers for Disease Control and Prevention (CDC) declared an “epidemic” of overdoses from prescription painkillers in 2011, the opioid crisis is worse than ever—yet it only vaguely resembles those earlier days. While people are still dying of overdoses tied to prescription opioids, the problem has largely shifted to illicitly trafficked opioids, such as fentanyl, and is now deeply intertwined with other non-opioid substances, such as methamphetamine and cocaine.
This blog examines the history and evolution of the opioid crisis through several charts based on data from SHADAC’s State Health Compare.
Changing attitudes in opioid prescribing
Today, it is broadly accepted that the over-prescribing of opioid painkillers—such as the blockbuster drug Oxycontin (a brand-name version of oxycodone produced by Purdue Pharma) and related semi-synthetic opioid hydrocodone—sparked what became an epidemic of overdoses and deaths. Over more than 10 years, deaths from overdoses involving those medications gradually crept upward until they finally capture widespread attention. When the toll of overdose deaths from prescription opioids was fully recognized and the U.S. healthcare system started to grapple with the problem, efforts to curb prescribing began.
In the first chart, data from the U.S. Drug Enforcement Agency show how legal sales of oxycodone and hydrocodone began the early days of the crisis at about 5 kilograms per 100,000 people in 2000. But within a decade, oxycodone sales roughly quadrupled and hydrocodone sales almost tripled (Figure 1). Following growing awareness of the problem, legal sales of both drugs—driven by prescriptions written by healthcare providers—have declined substantially. In 2021, hydrocodone sales had fallen to about 5 kilograms per 100,000 people, and oxycodone sales to less than 10 kilograms per 100,000 people.
Figure 1: Prescription opioid painkiller sales, 2000-2021
Source: SHADAC analysis of U.S. Drug Enforcement Agency's Automated Reports and Consolidated Ordering System (ARCOS) Retail Drug Summary Reports, obtained from statehealthcompare.shadac.org.
These data demonstrate that legal sales of prescription opioid painkillers are down dramatically from their heights when the CDC first rang alarm bells over the issue. However, some experts and advocates argue that the abrupt pivot in opioid prescribing practices was not done carefully enough, with many people who were already addicted to opioids suddenly cut off without sufficient screening for addiction or access to treatment. And data show that although deaths from prescription opioids have essentially plateaued since prescribing of opioid painkillers dropped, opioid overdose deaths have still continued to climb.
Persistently growing rates of opioid overdose deaths
Because overdose deaths were driven largely by prescription opioid painkillers in the early days of the epidemic, the hope and expectation was that death rates would drop as healthcare providers curtailed their prescribing of the risky medications. But this next set of charts shows that this hope was not fully realized.
In fact, the enhanced scrutiny on opioid prescribing and declining sales of prescription opioid painkillers appears to have marked a turning point in the epidemic. While deaths from prescription opioid painkillers have not declined dramatically, their growth trend leveled off and has remained relatively steady, around 4 deaths per 100,000 people, for almost a decade (Figure 2).
Figure 2: Prescription opioid painkiller death rates, 1999-2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
But to the shock and horror of many, overall overdose death rates—including prescription opioid painkillers as well as all other kinds of opioids—only continued to accelerate.
Figure 3: Death rates from all opioid types, 1999-2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
In less than a decade, the overdose death rate from all opioids roughly tripled, from 7.3 deaths per 100,000 people in 2011 to 21.4 deaths per 100,000 people in 2020 (Figure 3). But this time, the growth came from different types of opioids. First came heroin—an opioid that is without legal medical uses in the U.S. and is only available through the illicit drug trade. This was followed by fentanyl (and other closely related synthetic opioids), which does have legal medical uses but has been adopted by traffickers as a new drug of choice.
Figure 4: Death rates from fentanyl and other synthetic opioids, 1999-2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
In just a few years, the opioid crisis had transformed. What began as a problem rooted in widespread availability of prescription opioid painkillers shifted to illicitly trafficked opioids as legal opioid sales started to fall. By 2020, heroin overdose death rates had more than tripled since the CDC declared an opioid epidemic. And overdose death rates from fentanyl and similar synthetic opioids had grown more than 20 times (Figure 4).
In some ways, those developments may not be surprising. Economics tells us that when a good becomes scarce—such as prescription opioids after recognition of the crisis—people tend to cut back their consumption. But when people can’t simply stop their consumption, as in the case of addiction, they often turn to substitutes. With opioids, that unfortunately left many people to seek out substances such as heroin on the illicit market, where the purity and potency is unreliable, making them even riskier than prescription opioids. And once drug traffickers embraced the potent opioid fentanyl, it pervaded the illegal drug trade and became entangled with non-opioid substances, such as cocaine and methamphetamine.
A metastatic phase of the crisis
The opioid crisis is complex, and definitive evidence of how the epidemic evolved is hard to find. That is particularly the case in understanding the role of the illicit drug trade. However, it is widely accepted that some people shifted to heroin as prescription opioid painkillers became harder to obtain. Afterward, drug traffickers incorporated fentanyl into their supplies, sometimes to cheaply boost the potency of their heroin or simply to pass fentanyl off as heroin. Another approach was manufacturing counterfeit prescription medications, such as fake Oxycontin pills that actually contained fentanyl rather than the less-potent opioid oxycodone.
Over time, fentanyl became ubiquitous in the U.S. illicit drug market. Non-opioid illicitly trafficked substances, particularly cocaine and methamphetamine, are now often contaminated with fentanyl and related powerful opioids. And various kinds of illicitly trafficked counterfeit medications are found to contain fentanyl. In some cases, those counterfeit pills may mimic prescription opioid painkillers, but other counterfeit pills may contain fentanyl, even if the legitimate version does not. For instance, law enforcement agencies have reported interdicting fake stimulants (e.g., Ritalin and Adderall pills) that are mixtures of methamphetamine and fentanyl, even though the genuine medications do not contain opioids.
Ultimately, the pernicious impact of fentanyl and related synthetic opioids have transformed the opioid crisis. The prescription opioid painkillers that sparked this epidemic now only account for a fraction of drug overdose deaths in the U.S. (Figure 5), dwarfed by the toll of synthetic opioids such as fentanyl. And largely because of the pervasiveness of fentanyl in the market for illicit substances, deaths involving non-opioids also have grown to historic levels.
Figure 5: National Death rates for opioid and non-opioid substances, 2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
Lessons from opioids data
More than two decades into the opioid crisis, the main consistency is that the problem is continually evolving. When the role of prescription opioids in overdose deaths led the health care system to curtail dangerously generous prescribing of those medications, some people seemingly transitioned to illicitly trafficked opioids. When drug traffickers saw an opportunity to enhance their profits on heroin sales by using fentanyl and by manufacturing counterfeit pills, the epidemic became even deadlier. And as fentanyl became more pervasive, it also became intertwined with non-opioid substances, such as cocaine and methamphetamine—further extending the deadly reach of opioids.
To better understand and address the opioid crisis, it is important to use data to identify evolving patterns and trends and to anticipate new developments before they snowball into larger public health threats. Examining the history of the opioid crisis may prove useful to avoid recurrences of similar situations in the future, but it is also important to recognize the limitations of retrospective data for designing solutions to a dynamic situation. For instance, an overemphasis on prescribing of opioid painkillers now, when the vast majority of drug overdose deaths are caused by illicitly trafficked substances, could be considered akin to driving down a busy interstate highway while fixed on the rearview mirror.
Related Reading:
Blog: 2020 U.S. alcohol-involved deaths climbed by 26.6%, and drug overdose deaths by 30.6%
Resource Page: The Opioid Epidemic in the United States












