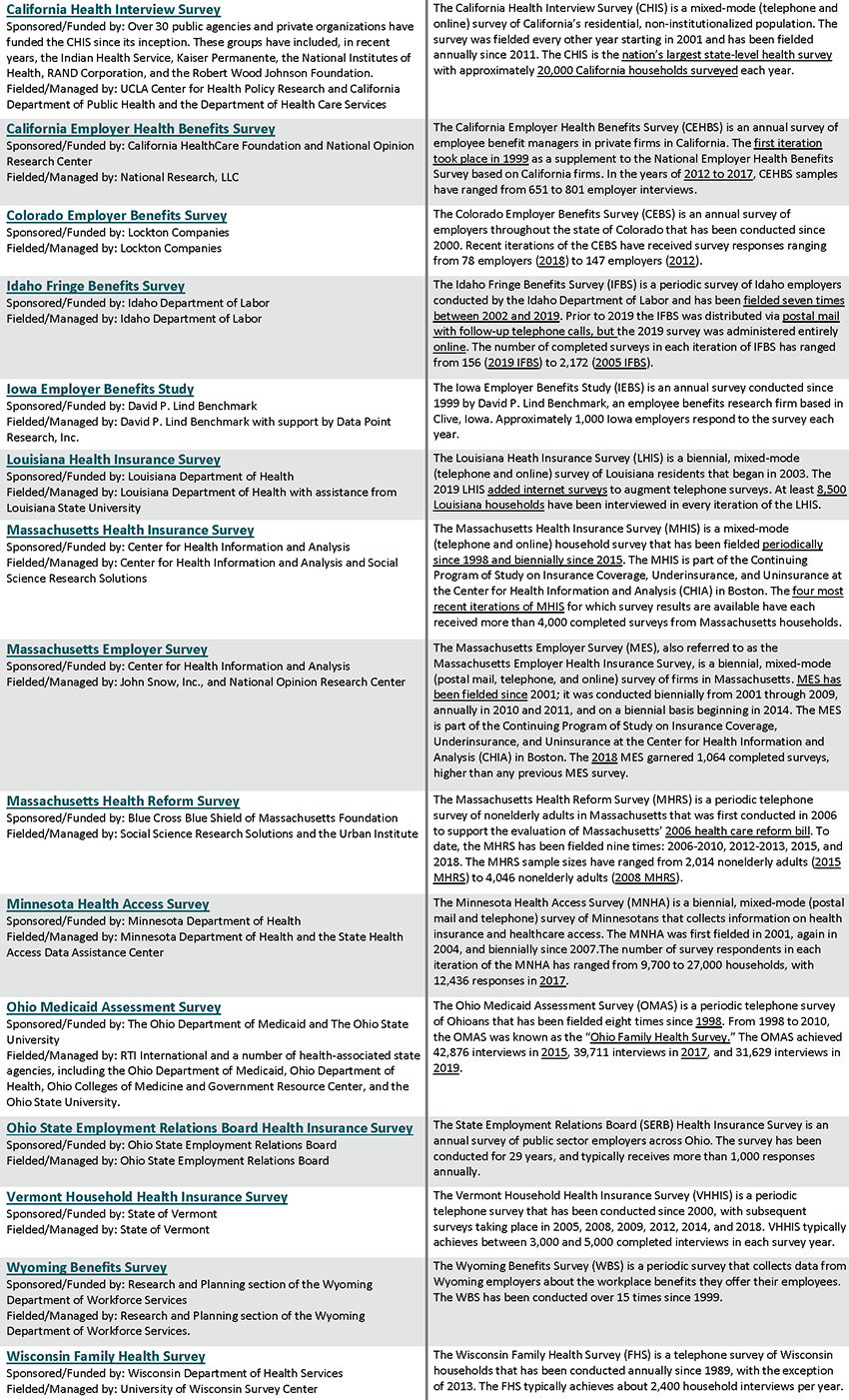
Publication
Overview of SHADAC's Minnesota Community and Uninsured Profile for MDH's Health Equity Data Community of Practice
On September 19, 2022, SHADAC investigator Kathleen Thiede Call presented at the Minnesota Department of Health's Health Equity Data Community of Practice Meeting. This presentation included a guided tour of SHADAC's Minnesota Community and Uninsured Profile, along with a brief history of how this resource was created. Click the image below to download the slide deck from this presentation.
Blog & News
Understanding the Medicaid MAGI and CHIP Application Process Time Performance Indicator
July 21, 2022:The speed and accuracy with which state Medicaid programs process applications will become increasingly important as the COVID-19 Public Health Emergency (PHE) comes to an end. Once states phase out the PHE, they will have to manage new Medicaid and Children’s Health Insurance Program (CHIP) applications at the same time they start processing the unprecedented volume of redeterminations and renewals that were on hold due to the continuous enrollment condition of the Families First Coronavirus Response Act (FFCRA). One performance indicator that provides a window into how efficiently state Medicaid programs process their Medicaid Modified Adjusted Gross Income (MAGI) and CHIP applications is Medicaid MAGI and CHIP Application Processing Times. This indicator was developed in 2013 to improve both programs through the provision and analysis of quality data. The Centers for Medicare and Medicaid Services (CMS) released its fourth update of this indicator in April 2022, which also appears as a measure of State Administrative Accountability on the Medicaid & CHIP Scorecard. In this blog, we provide an overview of the performance indicator and highlight the following themes that have emerged since the last reporting period (February – April 2021):
- Many states saw improvements in their processing times even as timeliness standards were relaxed during the PHE. Nearly 71 percent of all determinations on applications were conducted in less than 7 days.
- More than 51 percent of all determinations on applications were conducted in under 24 hours. On average, expansion states had a larger percentage of applications being processed under 24 hours than non-expansion states.
- 31 states either improved the number of applications processed within seven days, or stayed the same from 2020.
- Only 5 percent of all determinations do not meet CMS standards because they were conducted in over 45 days.
Overview of Performance Indicator and Data Quality
Every month, CMS relies on state Medicaid and CHIP agencies to collect and submit eligibility and enrollment data as part of CMS’ Performance Indicator Project. The MAGI and CHIP application processing times performance indicator provides an understanding of how many calendar days it takes between when the state agency receives an application and when it made a final eligibility determination using the MAGI standard. Determinations must be made within 45 days for new MAGI Medicaid applicants, and once the PHE ends, state agencies will have 4 months to resume timely application processing for both MAGI and non-MAGI Medicaid applications. States are not required to meet the timeliness standards for application processing due to COVID-19, which provides important context for these performance indicator findings: with increased applications and relaxed rules, many states were still able to make improvements to processing times during a time of crisis.1
The CMS provides technical assistance to ensure timely and accurate eligibility determinations – states are continuously improving their data quality for Medicaid MAGI and CHIP application times. Only three states - California, Nevada, and South Dakota - are not reporting on this indicator in 2021 (based on CMS’ specifications), which is a marked improvement from five states not reporting in 2020. However, it is important to note that this report only shows three months out of the year, and these data are constantly fluctuating based on policy changes and other factors that may or may not be state-specific.
Changes to MAGI Medicaid and CHIP Processing Times in 2021 by State
On average, close to 71 percent of applications were processed within seven days, which is well-above the CMS standard and an increase from 2020. Additionally, 19 states and the District of Columbia have processed their applications quicker than the seven day national average (see Figure 1). More than 51 percent of all determinations on applications were conducted in under 24 hours, which increased from 2020 as well.
Figure 1. Average Percent of MAGI Medicaid and CHIP Applications Processed within 7 days, States vs National, 2021

Source: SHADAC analysis of CMS Medicaid MAGI and CHIP Application Processing Times, 2021, available here: https://www.medicaid.gov/state-overviews/medicaid-modified-adjusted-gross-income-childrens-health-insurance-program-application-processing-time-report/index.html
In 2021, 31 states either improved the number of applications processed within seven days or stayed the same from 2020. (Almost the same number – although a slightly different mix – of states showed improvements in this indicator between 2019 and 2020 as well.) Oklahoma was one of two states that stayed the same (the other being Maryland) and had the highest number of applications (100%) processed; this was also achieved within 24 hours. Texas saw the greatest improvement, with a 46.7 percentage point [pp] increase. Texas’ level of improvement was followed by Iowa (43.7pp increase with 66.8 percent of applications processed within seven days in 2021), Georgia (42.6pp increase; 55.1 percent of applications processed within seven days), Missouri (41.5pp increase; 58.6 percent of applications processed within seven days), and Vermont (39.0pp increase; 96 percent of applications processed within seven days). In general, there are still nearly 5 percent of applications processed after 45 days (therefore not meeting the CMS standard) though this indicator has decreased from 2020.
On average, states that adopted the Affordable Care Act (ACA) Medicaid expansion had a larger percentage of processed applications within 24 hours than non-expansion states–an average of 40.5 percent of applications were processed within 24 hours by expansion states, compared to an average of 22.9 percent processed within 24 hours by non-expansion states. However, the average percentage of processed applications from both expansion and non-expansion states are comparable within 7 days, at 62.8 percent and 61.1 percent respectively.2
Medicaid enrollment grew significantly during the COVID-19 pandemic, driven by job and income loss as well as maintenance of eligibility (MOE) requirements. From February 2020 to April 2021, enrollment grew by 15.5 percent, and a rapid mini-survey of Medicaid directors from 44 states showed 8.9 percent enrollment growth for the 2022 fiscal year overall.3,4 However, application increases varied widely state-by-state. In general, application growth was significant, as 17 states saw an increase in applications in 2020 compared to 2019 (according to a national survey conducted by the Kaiser Family Foundation and the Georgetown University Center for Children and Families). Seven of those states reported increases higher than 10 percent.5, Of the 17 states experiencing application increases, over half saw a greater share of those applications being processed within 7 days.6 In addition, few of these states reported application backlogs.
However, there were nearly 29 percent fewer applications during the February to April 2021 reporting period compared to 2020. States that did not experience application increases could attribute this to a number of factors, including “smaller than expected declines in employer-sponsored insurance, [or] a drop in applications early in the pandemic due to office closures and the elimination of reapplications (where an individual loses coverage, often due to procedural reasons, then reapplies a short time later) due to the MOE requirements”.7
Conclusion
The CMS’ latest update on MAGI and CHIP application processing shows an overall improvement regarding processing times, despite significant increases in application volumes and the relaxation of timeliness standards during the PHE. While processing times have improved, there are still challenges with streamlined eligibility, enrollment, and renewal processes. CMS recently released a resource to remind states on best practices to process new applications, challenges to anticipate, and how to meet the requirements associated with submitting their data after the PHE. SHADAC has previously highlighted enrollment and renewal challenges that predated the pandemic as well as mitigation strategies. As we take these challenges into consideration alongside the end of the COVID-19 PHE, it will be necessary to continue monitoring this indicator for improvements and setbacks.
1 CMS. (2021, January 6). Covid-19 Frequently Asked Questions (FAQs) for State Medicaid and Children's Health Insurance Program (CHIP) Agencies. https://www.medicaid.gov/state-resource-center/downloads/covid-19-faqs.pdf
2 CMS. (2022, April 21). Medicaid MAGI and CHIP Application Processing Time Report. https://www.medicaid.gov/state-overviews/downloads/magi-application-time-report-2021.pdf
3 Williams, E. (2021, October 27). Medicaid Enrollment & Spending Growth: FY 2021 & 2022. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2021-2022/
4 Williams, E., & Hinton, E. (2022, April 4). Medicaid Spending and Enrollment: Updated for FY 2022 and Looking Ahead to FY 2023. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/medicaid-spending-and-enrollment-updated-for-fy-2022-and-looking-ahead-to-fy-2023/
5 Brooks, T., Gardner, A., Tolbert, J., Dolan, R., & Pham, O. Medicaid and CHIP Eligibility and Enrollment Policies as of January 2021: Findings from a 50-State Survey. Kaiser Family Foundation. https://www.kff.org/report-section/medicaid-and-chip-eligibility-and-enrollment-policies-as-of-january-2021-findings-from-a-50-state-survey-report/
6 SHADAC analysis of CMS Medicaid MAGI and CHIP Application Processing Time Report. https://www.medicaid.gov/state-overviews/downloads/magi-application-time-report-2021.pdf
7 Brooks, T., Gardner, A., Tolbert, J., Dolan, R., & Pham, O. Medicaid and CHIP Eligibility and Enrollment Policies as of January 2021: Findings from a 50-State Survey. Kaiser Family Foundation. https://www.kff.org/report-section/medicaid-and-chip-eligibility-and-enrollment-policies-as-of-january-2021-findings-from-a-50-state-survey-report/
Blog & News
SHADAC Advocates a Data-based Approach to Advancing Medicaid and CHIP Access Monitoring Plan (Response to CMS Request for Information)
April 29, 2021:On February 17, 2022, the Centers for Medicare & Medicaid Services (CMS) released a request for information (RFI) regarding access to coverage and care in Medicaid and the Children’s Health Insurance Program (CHIP).
SHADAC researchers focused our response on Objective 4: Question 1, which asked researchers to consider how CMS might develop a stronger Medicaid and CHIP access monitoring approach through data reporting and analysis, and is copied for reference below.
Portions of SHADAC’s response were also included as part of a larger commentary on each of the RFI’s five total objectives submitted to CMS by President and CEO Richard Besser, MD, of the Robert Wood Johnson Foundation (RWJF) on April 18, 2022.
|
Centers for Medicare & Medicaid Services (CMS) – Request for Information (2022) Objective 4: CMS has data available to measure, monitor, and support improvement efforts related to access to services (i.e., potential access; realized access; and beneficiary experience with care across states, delivery systems, and populations). CMS is interested in feedback about what new data sources, existing data sources (including Transformed Medicaid Statistical Information System [T-MSIS], Medicaid and CHIP Core Sets, and home and community based services (HCBS) measure set), and additional analyses could be used to meaningfully monitor and encourage equitable access within Medicaid and CHIP programs. 1. What should CMS consider when developing an access monitoring approach that is as similar as possible across Medicaid and CHIP delivery systems (e.g., fee-for-service and managed care programs) and programs (e.g., HCBS programs and dual eligibility in Medicaid and Medicare) and across services/benefits? Would including additional levels of data reporting and analyses (e.g., by delivery system or by managed care plan, etc.) make access monitoring more effective? What type of information from CMS would be useful in helping states identify and prioritize resources to address access issues for their beneficiaries? What are the most significant gaps where CMS can provide technical or other types of assistance to support states in standardized monitoring and reporting across delivery systems in areas related to access? |
Response from SHADAC
Thank you for the opportunity to help inform the development of an improved Medicaid and CHIP access monitoring plan. These comments are based on SHADAC’s experience providing data and evaluation technical assistance (TA) to states, which has given us a unique view into the day-to-day challenges and barriers that states encounter related to these issues. These comments mirror recent testimony to the Medicaid and CHIP Payment Access Commission (MACPAC) provided by SHADAC’s Deputy Director.
We present five points for your consideration, each of which are guided by the same principle, which is: That any monitoring plan should seek to minimize burden on state agencies.
First, consider an iterative approach that starts with a limited number of measures and expands over time. This will require difficult tradeoffs regarding priorities, but these tradeoffs will be worth it if the first iteration is achievable for a wide range of states. As the plan develops and more complicated measurement concepts are added, it should engage leading states by including them in additional measure selection and incentivizing them to participate in pilots that test the collection and analysis of data – sharing concrete implementation lessons with other states.
Second, support states in efforts to improve existing data with a focus on the ability to disaggregate. There are existing data streams to draw on (as documented by Urban Institute in 2017 and discussed at a recent MACPAC meeting), and while none are perfect, a successful plan should first focus on improving those. One tangible way to improve states’ existing data is to support data disaggregation efforts. There is a renewed focus and energy to promote equity within Medicaid and calls from stakeholders to see data about important groups of interest. This includes an interest in better data by race, ethnicity, sexual orientation, gender identity, disability, and geography. Improving existing data streams to better support disaggregation is a good investment and one that will meet multiple demands.
For example, the Transformed Medicaid Statistical Information System (T-MSIS) will likely play a role in monitoring service use, but there are concerns regarding the existing quality and completeness of the race and ethnicity data. We have worked with several states who are trying to improve the collection of race and ethnicity data in Medicaid—modifying question wording and expanding response options to better represent the populations they serve, making technical changes to better capture the data, and modifying instructional language and scripts for enrollment assisters to make them stronger partners in data collection. And, most importantly, they are doing this with community input. But they continue to face challenges in this work. For example, current OMB standards for demographics are dated and do not align with the most current research. Additionally, rules for collecting race and ethnicity data are not uniform across federal programs. A new access monitoring effort could serve as further impetus for federal agencies to revise the guidance on race and ethnicity and for states to take action to improve existing data collection to address this critical data gap.
Third, states need both direct funding and hands-on technical assistance to support this work. We appreciate CMS’s understanding that states will need assistance to implement the access monitoring framework. However, based on our work with states, we think this needs to go beyond documentation and uniform measure specifications. To do this well, states should have access to experts who can provide practical, hands-on advice that is responsive to their specific needs. The type of assistance needed will vary and needs to be flexible, from states who are further along in their process and may seek help troubleshooting a particular coding challenge to other states whose request might require more fundamental support, such as walking through the requirements to assess staff and training needs, setting priorities, and help developing contract amendments or RFPs. We would also recommend that any TA effort include a forum for states to discuss implementation challenges with their peers.
The funding provided to states for this effort should also be flexible. It should support direct costs like system modifications, but also things like stakeholder engagement, which is critical to the iteration and improvement of the monitoring plan, and related data collection, but will also allow the results of this monitoring to be shared in a meaningful way.
Fourth, some areas of Medicaid access monitoring are best addressed through federal data collection. We believe that the access monitoring effort would benefit from periodic fielding of a 50-state Medicaid Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey aimed at both children and adults and administered by the federal government. The federal government has a long and successful track record of fielding high-quality surveys that produce estimates for all 50 states, including a one-time National Medicaid Adult CAHPS survey.
While this undertaking would be resource intensive, it seems to us to be the most efficient way to collect comparable information on important facets of access, like enrollee experience, and a starting point for comparing individuals enrolled in fee-for-service versus managed care.
Finally, it is critical to treat states as a full partner in this process, including the communication of results. It goes without saying that states should be consulted in the development of the monitoring plan, but they should also be consulted when the data are being released, preferably beforehand. Ideally, they should have access to analytic files so that they can do their own data runs and share customized findings with stakeholders. Finally, once the data are collected, there should be a commitment that the data be published or released in some format in a timely manner.
Blog & News
NHIS: National Rates of Health Insurance Coverage for Third Quarter of 2021 Statistically Unchanged from 2020
January 25, 2022:On Wednesday, January 19, the National Center for Health Statistics (NCHS) announced that health insurance coverage estimates from the National Health Interview Survey (NHIS) Early Release Program are now available for Quarter 3 of 2021 (July-September)
At a high level, the new estimates show no significant changes in coverage type (public, private) or uninsured rate across all ages and income groups when compared to the same time period in 2020, as discussed below.
Age
Among nonelderly adults (ages 18 to 64) surveyed between July and September of 2021, 13.0% were uninsured at the time of interview, 21.1% had public coverage, and 67.3% had private coverage. Comparatively, these rates measured at 14.1%, 20.3%, and 67.4% from July to September in 2020, as shown in Figure 1.
Figure 1. Type of Health Insurance Coverage Nonelderly Adults (18-64 years), Q3 2020 and Q3 2021

Poverty Level
Again among nonelderly adults at three differing thresholds of family income as a percentage of the federal poverty level (less than 100% FPL, 100%-199% FPL, and 200%+ FPL), rates of uninsurance as well as public and private coverage remained statistically unchanged in Q3 2021 from Q3 2020.
Looking at the below than 100% FPL category for nonelderly adults from July-September 2021, 21.7% were uninsured, 52.3% had public coverage, and 27.2% had private coverage. These rates were 28.6%, 51.3%, and 22.3%, respectively in 2020 (Figure 2).
Figure 2. Type of Health Insurance Coverage (<100% FPL) Nonelderly Adults (18-64 years), Q3 2020 and Q3 2021

COVID-19 and Cautions for 2020 NHIS Estimates
As has been extensively documented in reports from both SHADAC and NCHS, COVID-19 caused numerous disruptions to federal survey data collection and production efforts. For the NHIS in particular, personal visits were suspended beginning on March 19, 2020, and data collection in late Q1 and for all of Q2 in 2020 switched to a telephone-only mode. Personal visits (with telephone attempts first) resumed in all areas in September 2020.
Data collection methodologies were not the only casualty of the pandemic, however. While the initial NCHS report examined preliminary nonresponse bias in Q1 and Q2 of 2020, the same team published a follow-up report in September 2021 looking at effects of the pandemic on estimates for the entire year, including July to December 2020. Though in-person operations resumed, lingering concerns about low response rates and possible loss of coverage caused survey conductors to replace approximately half of the usual sample for the last 5 months of 2020 with a longitudinal component where a subset of the 2019 sample adults were re-interviewed over the telephone using the 2020 NHIS questionnaire. This process change means that comparisons between estimates from July–December 2020 and other time periods may be impacted by these differences in survey mode and methodology.
About the Numbers
The above estimates provide a point-in-time measure of health insurance coverage, indicating the percent of persons with that type of coverage at the time of the interview. The 2021 estimates discussed in this blog are only from Q3 (July-September) as well as the same period in 2020.
Differences described in this post are statistically significant at the 95% confidence level unless otherwise specified.
Citations
Cohen, R.A. & Cha, A.E. (2022, January 19). Health Insurance Coverage: Early Release of Quarterly Estimates from the National Health Interview Survey, July 2020–September 2021. National Center for Health Statistics (NCHS). https://www.cdc.gov/nchs/data/nhis/earlyrelease/Insur201902.pdf.
Dahlhamer, J.M., Bramlett, M.D., Maitland, A., & Blumberg, S.J. (February 2021). Preliminary evaluation of nonresponse bias due to the COVID-19 pandemic on National Health Interview Survey estimates, April-June 2020. National Center for Health Statistics (NCHS). https://www.cdc.gov/nchs/data/nhis/earlyrelease/nonresponse202102-508.pdf
Bramlett, M.D., Dahlhamer, J.M., & Bose, J. (September 2021). Weighting procedures and bias assessment for the 2020 National Health Interview Survey. National Center for Health Statistics (NCHS). https://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2020/nonresponse-report-508.pdf
Blog & News
SHADAC’s New State Survey Research Resource Page
December 10, 2021:Early this fall, SHADAC updated its State Survey Research Activity web page using an interactive infographic (preview to the right) to allow users to easily identify the type and frequency of state-level health insurance surveys (household and/or employer) available for all 50 states and the District of Columbia. The surveys accessible through the page were collected from 2010 through 2021, with surveys that predate 2010 housed in SHADAC’s archives and available upon request.
State Surveys in Summary
In all, 27 states field and report ongoing household and/or employer surveys, and 6 of these states have conducted surveys nearly every year since 2010. Ohio has the longest continuous record with 11 iterations of its employer survey fielded since 2010.
Available Information
The updated State Survey web page uses an infographic to enable quick navigation to PDF-format state survey materials, including survey questionnaires, findings, methodology reports, technical documentation, and summary briefs. The update includes surveys that are accessible online and free of charge. SHADAC will be adding additional surveys, including the 2021 Massachusetts Health Insurance Survey and 2021 Oregon Health Insurance Survey (both of which are currently underway), as they become available.
State Health Insurance Surveys Highlights
Since 2019, twenty states have conducted household or employer surveys. Eleven of these states have conducted their surveys multiple times over the course of at least a fifteen-year period, and even longer in some cases. The long-standing surveys conducted by states including California, Colorado, Idaho, Iowa, Louisiana, Massachusetts, Minnesota, Ohio, Vermont, Wisconsin, and Wyoming are highlighted below.