Blog & News
State 1332 Waiver Reinsurance Proposals: News from Maine, Louisiana, Maryland, and Wisconsin
May 08, 2018:Since April, Maine, Louisiana, and Maryland have all released Draft 1332 Waiver Applications with proposals for state-based reinsurance programs, and Wisconsin has submitted its 1332 Waiver Application to CMS seeking approval and pass-through funding for its reinsurance program.
Tracking State 1332 Waiver Reinsurance Developments
We have updated our 1332 Waiver Reinsurance Proposals resources to include the newly released waivers in Maine, Louisiana, and Maryland, and to reflect changes to Wisconsin’s reinsurance proposal contained in its 1332 Waiver Application to CMS. We have expanded the side-by-side comparison table to incorporate the new waivers and also updated our Reinsurance Waiver timeline with further analysis of these waivers. We will continue to update these resources as new developments occur.
Blog & News
Kids' Health Data Highlight: Children Living in Neighborhoods with No Amenities in 2016 (Infographic)
May 1, 2018:It is increasingly clear that health is determined not just by biological and clinical factors but to a greater extent by socio-demographic factors. With this in mind, we need data for monitoring the social determinants of health just as we do for monitoring biological and clinical determinants. The U.S. Census Bureau recently released estimates from the 2016 National Survey of Children’s Health (NSCH), providing a data source that is ideal for precisely this purpose. The NSCH provides traditional measures of health status and access to care among children along with rich data on the social factors that determine health including family, neighborhood, school, and social context.
SHADAC is highlighting state-specific findings from the 2016 NCSH on measures that illustrate where states are closer to achieving a culture of health and where improvements can be made. As additional years of NCSH data are released, we will be able to monitor trends in these indicators to track progress in developing a culture of health over time.
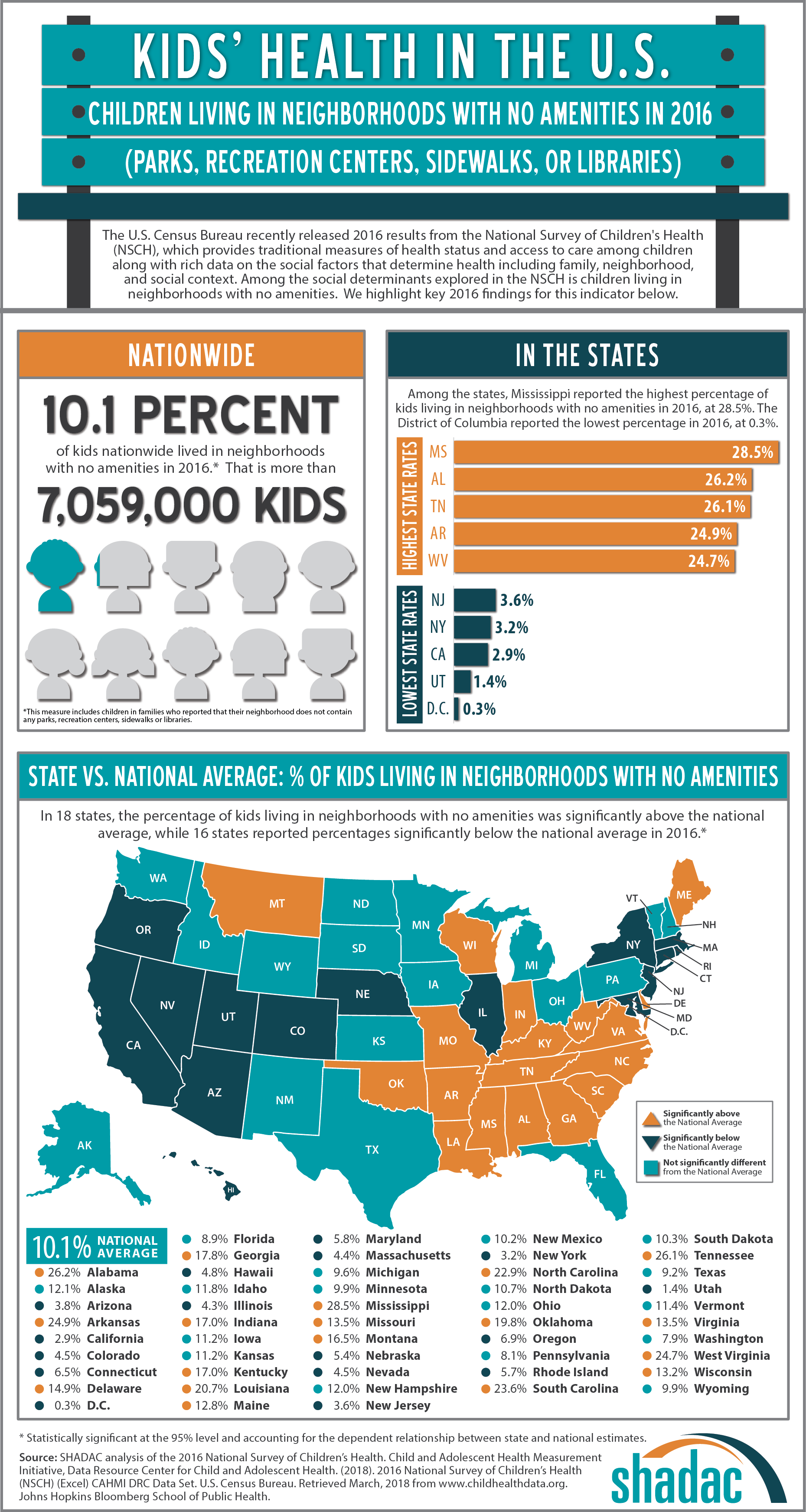 Kids Living in Neighborhoods with No Amenities
Kids Living in Neighborhoods with No Amenities
According to 2016 data from the NSCH, 10.1% of children nationwide (approximately 7,059,000 children) lived neighborhoods with no amenities in 2016, defined as a neighborhood without any parks, recreation centers, sidewalks, or libraries.
Among the states, the highest percentages of children living in neighborhoods with no amenities were found in Mississippi (28.5%), Alabama (26.2%), Tennessee (26.1%), Arkansas (24.9%), and West Virginia (24.7%). The lowest percentages were found in the District of Columbia (0.3%), Utah (1.4%), California (2.9%), New York (3.2%), and New Jersey (3.6%).
In all, 18 states were statistically above the national average of 10.1% of children living in neighborhoods with no amenities, and 16 were below the national average.[1]
Click on the infographic for additional state-level information about children living in neighborhoods with no amenities.
Additional Kids’ Health Data Highlights
Kids' Health in the U.S.: Difficulties Making or Keeping Friends in 2016
Kids' Health in the U.S.: Parental Attendance at Kids' Activities in 2016
Kids’ Health in the U.S.: Living in Supportive Neighborhoods in 2016
Kids’ Health in the U.S.: Living in Working Poor Households in 2016
Kids’ Health in the U.S.: Trouble Affording Nutritious Meals in 2016
More about the NSCH
The NSCH was administered three times prior to 2016 – in 2003, 2007, and 2011/12. However, the 2016 NSCH is different because it integrated the NSCH with the National Survey of Children with Special Health Care Needs (NS-CSHCN) and introduced a number of new survey items, establishing a new baseline. Going forward, the NSCH will be administered annually. The survey is administered online and via mail, and survey results are weighted to represent the population of non-institutionalized children ages 0-17 who live in housing units nationally and in each state.
The full 2016 NSCH public-use file (PUF) is available on the Census Bureau’s NSCH page.
[1] Statistically significant differences are calculated at the 95% level and account for the dependent relationship between state and national estimates.
Blog & News
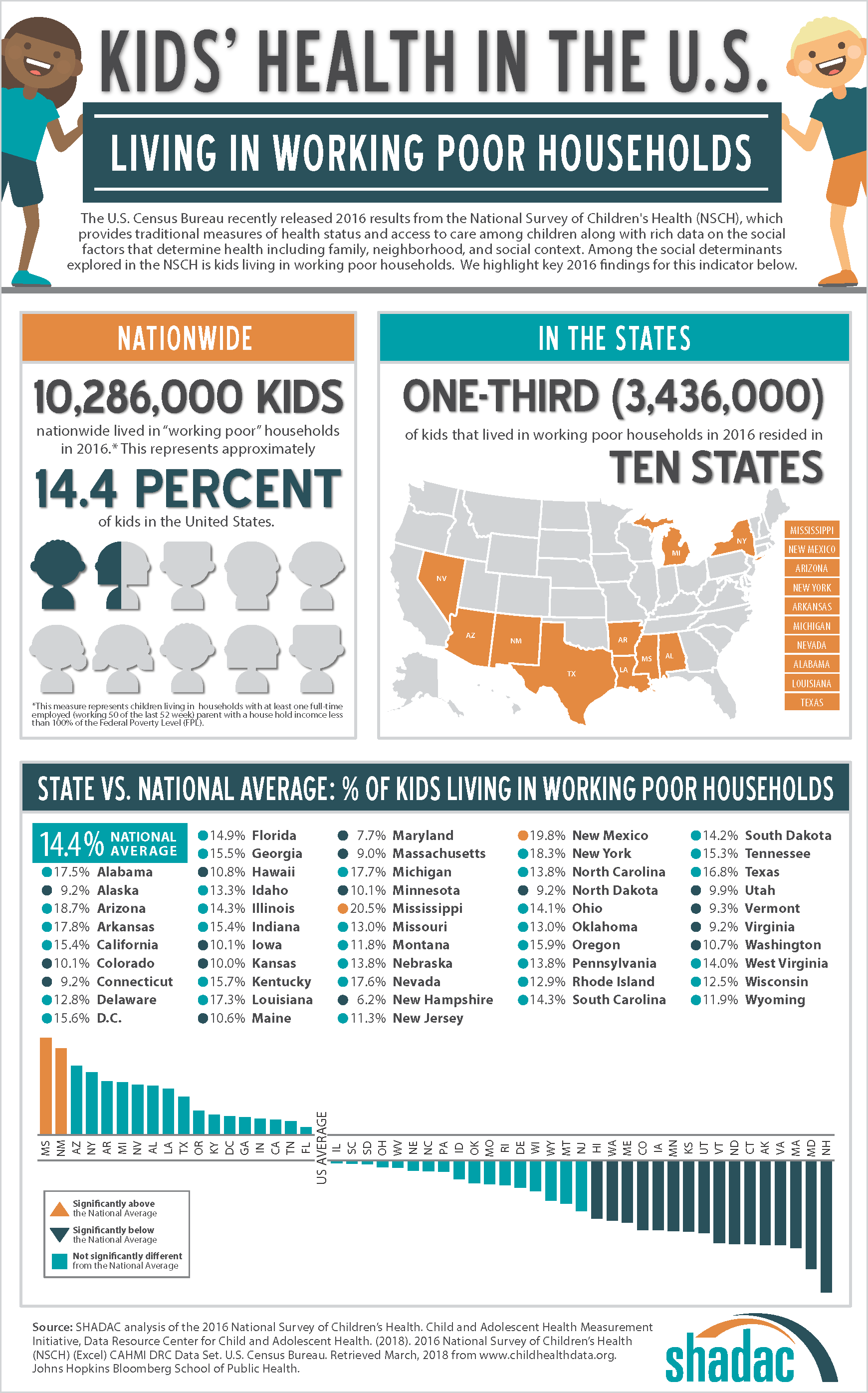
Kids' Health Data Highlight: Children Living in Working Poor Households in 2016 (Infographic)
April 13, 2018:It is increasingly clear that health is determined not just by biological and clinical factors but to a greater extent by socio-demographic factors. With this in mind, we need data for monitoring the social determinants of health just as we do for monitoring biological and clinical determinants. The U.S. Census Bureau recently released estimates from the 2016 National Survey of Children’s Health (NSCH), providing a data source that is ideal for precisely this purpose. The NSCH provides traditional measures of health status and access to care among children along with rich data on the social factors that determine health including family, neighborhood, school, and social context.
In the coming weeks, SHADAC will be highlighting state-specific findings from the 2016 NCSH on measures that illustrate where states are closer to achieving a culture of health and where improvements can be made. As additional years of NCSH data are released, we will be able to monitor trends in these indicators to track progress in developing a culture of health over time.
Kids Living in Working Poor Households
According to 2016 data from the NSCH, 14.4% of children nationwide (approximately 10,286,000 children) lived in working poor households in 2016.[1] Of these, roughly one-third (approximately 3,436,000) resided in ten states: Mississippi, New Mexico, Arizona, New York, Arkansas, Michigan, Nevada, Alabama, Louisiana, and Texas.
In all, the percentage of children that lived in working poor households was statistically above the national average in two states and statistically below the national average in 16 states.
At 20.5%, Mississippi had the highest percentage of children living in working poor households, while New Hampshire, at 6.2%, had the lowest percentage of children living in working poor households.
Click on the infographic for additional state-level information about children living in working poor households.
Additional Kids' Health Data Highlights
Kids' Health in the U.S.: Difficulties Making or Keeping Friends in 2016
Kids' Health in the U.S.: Parental Attendance at Kids' Activities in 2016
Kids'Health in the U.S.: Living in Neighborhoods with No Amenities in 2016
Kids’ Health in the U.S.: Living in Supportive Neighborhoods in 2016
Kids’ Health in the U.S.: Trouble Affording Nutritious Meals in 2016
More about the NSCH
The NSCH was administered three times prior to 2016 – in 2003, 2007, and 2011/12. However, the 2016 NSCH is different because it integrated the NSCH with the National Survey of Children with Special Health Care Needs (NS-CSHCN) and introduced a number of new survey items, establishing a new baseline. Going forward, the NSCH will be administered annually. The survey is administered online and via mail, and survey results are weighted to represent the population of non-institutionalized children ages 0-17 who live in housing units nationally and in each state.
The full 2016 NSCH public-use file (PUF) is available on the Census Bureau’s NSCH page.
[1] This estimate includes children living in households with at least one full-time employed (working 50 of the last 52 weeks) parent with a household income below 100% of the federal poverty level.
Blog & News
State 1332 Waiver Reinsurance Proposals: Wisconsin Releases Draft 1332 Waiver Seeking $170 Million in Pass-Through Funding
March 30, 2018:Please visit our 1332 Waiver Reinsurance resource page for the most current information about state 1332 Waiver Reinsurance activities. We will continue to update this resource as new developments occur.
Seven states—Alaska, Minnesota, Iowa, Oklahoma, New Hampshire, Oregon, and Wisconsin—have released 1332 State Innovation Waiver Applications seeking federal pass-through funding for state-based reinsurance programs.
| Three Types of Reinsurance Programs | |
|---|---|
|
The reinsurance programs proposed in the 1332 Waivers are of three different designs. Iowa, Minnesota, Oklahoma, New Hampshire, Oregon, and Wisconsin's proposals are traditional reinsurance programs where claims in a specified corridor (e.g. $50,000–$250,000) are paid, minus a coinsurance rate; Alaska’s program is condition specific, with the state paying all claims for individuals with one or more of 33 specific conditions; and Idaho’s program combines state-funded, condition-specific reinsurance; condition-specific Medicaid eligibility for individuals below 400% FPL with complex medical needs; and individual-market premium and cost-sharing subsidies for individuals below 100% FPL. |
A seventh state, Idaho, released 1332 and 1115 waivers requesting condition-specific Medicaid eligibility for individual-market enrollees with complex medical conditions; the state also created a state-funded, condition-specific individual market high-risk pool.
As of February 20, 2018, three states have received approval of their 1332 Waiver reinsurance proposals (AK, MN, and OR), two states (OK and IA) submitted and withdrew their applications, one state (NH) did not submit its application after releasing a draft for public comment, and one state (ID) has released dual 1332/1115 Waivers for comment with the intention of submitting formal applications to CMS in 2018.
Below is a table comparing the design details and waiver status for each state’s proposed reinsurance program and a timeline of 1332 Waiver reinsurance proposal developments..
|
1332 STATE INNOVATION WAIVERS FOR STATE-BASED REINSURANCE: PROPOSAL DESIGNS
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Alaska Comprehensive Health Insurance Fund | Minnesota Premium Security Plan | Iowa Stopgap Measure (ISM) | Oklahoma Individual Health Insurance Market Stabilization Program (OMSP) | New Hampshire 1332 Waiver Reinsurance Plan | Oregon Reinsurance Program (ORP) | Wisconsin Healthcare Stability Plan (WIHSP) | Idaho Complex Medical Needs Waiver | |
| REINSURANCE PROPOSAL | ||||||||
| Reinsurance Type | Condition-specific reinsurance | Traditional reinsurance | Traditional reinsurance | Traditional reinsurance | Traditional reinsurance | Traditional reinsurance | Traditional reinsurance | Condition-specific Medicaid eligibility, condition-specific reinsurance |
| Reinsurance Corridor | All claims from policyholders with one of 33 specific medical conditions | $50,000 – $250,000 | $100,000 – $3,000,000 | $15,000 – $400,000 |
$45,000 – $250,000 |
TBD – $1,000,000 | $50,000 – $250,000 | $25,000 – |
| Coinsurance Rate | 100% | 80% / 20% | 85% / 15% (Claims > $3 Million: 100%) |
80% / 20% | 40% / 60% | 50% / 50% | TBD (50% – 80%) | At least 20% |
| Legislation Enacted | HB 374 November 7, 2016 |
HF 5 April 4, 2017 |
No applicable state legislation | HB 2406 June 6, 2017 |
HB 469 July 10, 2017 |
HB 2391 July 5, 2017 |
SB 770 February 27, 2018 |
S1150 April 6, 2017 Enacting state legislation for waivers expected April 2018 |
| 1332 STATE INNOVATION WAIVER | 1115/1332 WAIVER | |||||||
| Waiver Status |
Submitted |
Submitted May 5, 2017 Approved September 22, 2017 Signed October 16, 2017 |
Submitted June 12, 2017 Submitted August 22, 2017 Amended September 22, 2017 Withdrawn October 23, 2017 |
Submitted August 16, 2017 Withdrawn September 29, 2017 |
Draft waiver released for public comment July 19, 2017 | Submitted August 31, 2017 Approved October 19, 2017 |
Draft waiver released March 13, 2018 | 1332 waiver released for public comment November 1, 2017 1115 waiver released for public comment November 22, 2017 |
| State Funding | $55 million annually (51.6% of total) |
$271 million annually (61.9% - 66.3% of total) |
$0 (0% of total) |
$16 million in 2018 $230 million over five years (14.2% of total) |
$32 million annually (71.4% of total) | $90 milion in 2018 $1.1 billion over ten years (68.5% of total) |
$30 million in 2019 | $16 million in 2019 for state-funded high risk pool |
| Source of State Funds | $55 million in initial funding from General Fund, then funded via assessments on all insurers: • Health: 6% of gross premiums less paid claims • Title: 1% of gross premiums • Other: 2.7% of gross premiums |
Dedicated funding from Health Care Access Fund (financed via 2% provider assessment) and General Fund | No state funding | Assessment on premiums charged by all health insurers and reinsurers | Annually-determined assessment on health insurers per covered life, necessary to fund reinsurance pool | 1.5% assessment on fully insured commercial major medical premiums | State general fund | Net losses of state reinsurance pool funded by annually-determined assessment on insurers |
| 1332 Funding Request | $51.6 million in pass-through funding (48.4% of total) |
$138 - $167 million in pass-through funding (33.7% - 38.1% of total) |
$70 million in pass-through funding for reinsurance in 2018 (100% of total) $396 million total waiver funding in 2018 |
$309 million in pass-through funding in 2018 $1,395 million over five years (85.8% of total) |
$12.8 million in pass-through funding for reinsurance (28.6% of total) | $35.66 million in 2018 $356.6 million over ten years (31.5% of total) |
$170 million in pass-through funding in 2019 (85% of total) | $0 for reinsurance. $613 million in 1332/1115 waiver funding |
| 1332 Funding Received | $58.5 million (2018) $332 million (2018-2022) |
$130.7 million (2018) $1.003 billion (2018-2020) |
$54.5 million (2018) | |||||
| INDIVIDUAL MARKET | ||||||||
| Marketplace Type 1 | Federally-facilitated Marketplace | State-based Marketplace | State-partnership Marketplace | Federally-facilitated Marketplace | Federally-facilitated Marketplace | State-based Marketplace with Federal Platform | Federally-facilitated Marketplace | State-based Marketplace |
| Medicaid Expansion Status | Expanded Medicaid 2 | Expanded Medicaid 3 |
Expanded Medicaid 4 | Did not expand Medicaid | Expanded Medicaid4 | Expanded Medicaid | Did not expand Medicaid | Did not expand Medicaid |
TIMELINE OF 1332 WAIVER REINSURANCE PROPOSAL DEVELOPMENTS
3-13-2018 Wisconsin releases Draft 1332 Waiver Application. Wisconsin released a draft of its 1332 Waiver Application, seeking $170 million in federal pass-through funding for its state reinsurance program, the Wisconsin Healthcare Stability Plan (WIHSP). The state anticipates that if approved, WIHSP would reduce 2019 individual market premiums by 10% relative to premiums if the plan were not approved.
2-6-2018 CMS sets Alaska and Oregon pass-through funding for 2018. CMS notified Alaska that the state would receive an estimated $58.5 million in pass-through funding for reinsurance in the 2018 calendar year. CMS had initially determined that Alaska would receive $48.3 million in pass-through funding for the state’s reinsurance program. Oregon will receive $54.5 million in pass-through funding for its reinsurance program, nearly $19 million more than the $35.7 million it was set to receive as of its waiver approval.
1-26-2018 CMS sets Minnesota pass-through funding for 2018. CMS notified Minnesota that the state would receive an estimated $130.7 million in pass-through funding for the state’s reinsurance program in calendar year 2018. This was $8.5 million less than the $139.2 million specified in CMS’s initial waiver approval.
11-2017 Idaho released its draft 1332 and 1115 Waiver Applications. Idaho released draft 1332 and 1115 Waiver Applications for public comment. The proposed program is a novel combination of a new Medicaid eligibility category for individuals below 400% FPL with complex medical conditions; a state-funded, condition-specific individual market high-risk pool; and extending individual-market premium tax credits and cost-sharing reductions to individuals below 100% FPL. The state projects that their proposal will cover an additional 21,000 individuals while reducing total federal expenditures by $2 million.
10-23-17 Iowa withdrew its 1332 Waiver Application. Iowa’s Insurance Commissioner Doug Ommen withdrew the state’s 1332 Waiver Application, citing overly restrictive 1332 Waiver requirements that prevented the state from implementing its Stopgap plan under terms that would be workable for the state.
10-16-17 Minnesota accepts 1332 Waiver terms. Minnesota Governor, Mark Dayton officially accepted the Special Terms and Conditions for the state’s 1332 Waiver, though he reasserted his strong disagreement with CMS’s interpretation of federal law that led to its decision to not pass through federal savings on funding for the state’s Basic Health Plan (BHP), MinnesotaCare. Gov. Dayton specified that in signing the STCs, he was not waiving Minnesota’s right to the full amount of its federal BHP funding based on the state’s argument outlined in an October 4 memo to CMS.
9-29-17 Oklahoma withdrew its 1332 Waiver Application. Oklahoma notified CMS that it was withdrawing its 1332 Waiver Application. Oklahoma blamed CMS for missing a mutually-agreed-upon September 25 deadline for approval necessary for the state to implement its reinsurance program before the 2018 plan year. CMS had previously determined the application to be complete and indicated that approval would be forthcoming by the September 25 deadline. The state plans to seek a 1332 Waiver for reinsurance in future years.
9-22-17 CMS approved Minnesota’s 1332 Waiver. CMS has approved Minnesota’s 1332 Waiver Application, giving the state $139 million in pass-through funding for reinsurance in 2018, and a total of $1 billion in funding over five years. This is the amount the federal government will save in premium tax credits and cost-sharing reduction payments due to Minnesota’s reinsurance program. However, as Gov. Mark Dayton anticipated in a September 19 letter to Secretary Price, CMS will not pass through the money it will save on funding for the state’s Basic Health Program (BHP), MinnesotaCare since BHP funding is based on 95% of the amount of premium tax credits and cost-sharing reductions that would have been provided to BHP enrollees. Though CMS does not specify how much funding the state will lose for MinnesotaCare, Gov. Dayton claims that the state would lose $369 million in BHP funding over two years, more than it would gain in pass-through funding for reinsurance. The state has 30 days from receipt of the approval letter to accept or reject the terms of approval.
9-17-17 Iowa submitted an amendment to its 1332 Waiver. Iowa provided a supplement to its 1332 Iowa Stopgap Measure to increase the cost sharing subsidies available to individuals with incomes between 133–150% FPL. The state expects that the additional subsidy will increase participation of young, healthy individuals in its individual market, improving the risk pool and keeping premiums down. Because of this improved risk pool, the state is decreasing its reinsurance pass-through funding request from $80 million to $70 million.
8-31-17 Oregon submitted its 1332 Waiver Application. Oregon’s waiver seeks pass-through funding for its reinsurance proposal. $90 million in annual state funding for reinsurance plan is paid for through a 0.3% assessment levied on major medical premiums and through excess fund balances in two state programs. The state is seeking more than $30 million annually in federal pass-through funding. The reinsurance plan has a coinsurance rate of 50% and a cap of $1 million. The attachment point is to be determined.
8-16-17 Oklahoma submitted its 1332 Waiver Application. The Department of Health and Human Services submitted Oklahoma’s 1332 waiver, the Individual Health Insurance Market Stabilization Program (OMSP). The OMSP will have a broad corridor of $15,000 – $400,000 and will be largely funded with federal pass-through funding, with a smaller portion coming from a state assessment on health insurers.
8-1-17 Minnesota released preliminary individual market premiums. The Minnesota Department of Commerce published anticipated premium increases by health plans with and without reinsurance. With state reinsurance, plans expect that 2018 premiums could be modestly higher (largest increase 11.4%) to substantially lower (largest decrease 40.8%) than 2017 premiums. Without state reinsurance, plans project much larger increases in 2018 premiums.
7-19-17 New Hampshire released its Draft 1332 Waiver Application. The New Hampshire Department of Insurance released a draft of its 1332 Waiver application for public comment. The waiver proposes a traditional reinsurance program with a corridor of $45,000 – $250,000 and a 40% / 60% coinsurance rate. The application seeks $12.8 million in federal pass-through funding.
7-14-17 Oklahoma released its Draft 1332 Waiver Application. The Oklahoma Department of Insurance released a draft of its 1332 Waiver Application for public comment. Oklahoma’s 1332 waiver proposal includes reinsurance along with broader reforms to its individual market. The state is awaiting further actuarial analysis before determining its reinsurance plan’s corridor, coinsurance rate, and level of pass-through funding. Oklahoma’s proposal is a traditional reinsurance plan funded by assessments on health insurers.
7-7-17 CMS approved Alaska’s 1332 Waiver Application. CMS notified Alaska that its 1332 Waiver Application had been approved. The state was awarded $48.3 million in federal pass-through funding in 2018, and a total of $322 million over five years.
1 Kaiser Family Foundation. “State Health Insurance Marketplace Types, 2017.” http://www.kff.org/health-reform/state-indicator/state-health-insurance-marketplace-types/.
2 Expanded Medicaid September 1, 2015
3 Minnesota also has MinnesotaCare, the Basic Health Program (BHP) for individuals 138–200% FPL.
4 Expanded Medicaid with Section 1115 Waiver
Blog & News
SHADAC Brief Examines Minnesota's Accountable Communities for Health
October 15, 2019:SHADAC researchers released a new brief that provides the context surrounding the development and implementation of Minnesota’s Accountable Communities for Health, or ACHs, and describes key components of ACH models implemented across the state. The following are highlights from the brief.
ACHs: Defined
Minnesota's ACHs are community-led models of delivering medical and non-medical care and services to improve the health of a target population with substantial health and social needs. ACHs bring together diverse community partners, driven by the specific needs of the target population and the prevailing health and social conditions in the community. [1] The state awarded grants to fund the creation of 15 ACHs under the federal State Innovation Model (SIM) Initiative.
ACH Requirements
Core requirements for ACHs were to (1) establish a collaborative leadership structure that involved community partners; (2) develop and implement a community-based care coordination system or team; and (3) implement a population-based health prevention plan. Other key elements of Minnesota’s ACH model include a sustainability plan, a measurement plan, and participation in Learning Collaborative and evaluation activities.
ACH Characteristics
-
In all, eight ACHs were anchored in urban areas, six were located in rural areas, and one had both an urban and rural presence (Figure 1).
-
Three of the ACHs were outgrowths of an earlier Minnesota grant program, called the Community Care Team (CCT) pilot, which was administered from 2012 to 2013 by the Minnesota Department of Health’s patient-centered medical home initiative and was meant to expand beyond the medical focus of health care homes.
-
Eight ACHs established care coordination models that focused broadly on the medical and social needs of their target populations without regard to a specific category of health condition; four were focused on mental and behavioral health (e.g., depression, substance abuse, serious and persistent mental illness, etc.) within their target populations; and three focused on specific or comorbid chronic medical conditions within their target populations.
ACH Leadership and Partners
-
In all, ACHs identified 279 organizational partners, including partners who held both leadership and operational roles. The number of partners involved in any individual ACH ranged from six to 34.
-
In nearly all (14) ACHs, an Accountable Care Organization (ACO) representative or provider participant served on the ACH Leadership team. When the ACH target population overlapped, select ACO partners provided data, data analytics, and connections with providers and have been a source of patients/referrals for the ACHs.
-
Two-thirds (10) of ACHs involved a local public health partner in their work. ACHs with a public health partner reported that public health organizations brought a health promotion focus, hired key coordination staff, conducted population health activities, contributed data and evaluation expertise, and supported community engagement and relationship building.
-
Nine ACHs included at least one community or target population member on their leadership teams.
ACH Community-Based Care Coordination Systems or Teams
-
Because of the flexibility of the ACH program, as a result of which the ACHs were working with a broad range of target populations across a variety of settings, no single care coordination model accurately captures the various ACH care coordination approaches. Instead, ACH care coordination models can best be conceptualized by looking at the locus/anchor of care coordination and the intensity of care coordination services provided.
-
Nine ACHs conducted care coordination from the starting point of a medical facility or organization (clinic, hospital, health plan); four initiated care coordination within a community organization (social service agency, school, group living community); and two used a combination of medical and community-based starting points.
-
The care coordination efforts of about half of the ACHs fall at multiple points along a continuum of intensity that increases in tandem with patient needs. In these cases, services ranged from the provision of information and resources to a referral and/or handoff to an extensive wraparound. Other ACHs tended to concentrate their work at certain points along the continuum, depending largely on the needs of their target populations. Four ACHs, for example, targeted particularly high-need individuals such as those with developmental disabilities and mental illness, and therefore focused on high-intensity coordination work.
-
ACHs varied in terms of care coordination reach, with the average number of individuals reached per quarter by a given ACH ranging from fewer than 100 to more than 300 in 2016.
ACH Population-Health Based Prevention Plans
-
In developing their population-based prevention plans, ACHs frequently built upon prevention work intiatied or underway through other community efforts. For example, six ACHs leveraged the Statewide Health Improvement Program, three leveraged Community Transformation Grants, and nine leveraged other local public health initiatives.
-
All ACHs focused in whole or in part on the same populations for both their care coordination and population health components, with frequent overlap between care coordination and population health activities.
-
Where data was provided/available, ACHs reported reaching anywhere from 201 to 3,000 individuals each through population health programming and activities.
Funding: The Federal SIM Initiative
ACHs in Minnesota were funded through a $45 million state’s State Innovations Model (SIM) cooperative agreement, awarded to the Minnesota Department of Human Services in 2013 by the Center for Medicare and Medicaid Innovation (The CMS Innovation Center). Administered by the Minnesota Departments of Health and Human Services, the funding was used to implement the Minnesota Accountable Health Model Framework, for which SHADAC was the state evaluator.
State-Led Evaluation: SHADAC
The Innovation Center required a federal multistate evaluation of the SIM initiative as well as individual state evaluations. The Minnesota Department of Human Services contracted with SHADAC to design and conduct the state evaluation of Minnesota’s SIM initiative. The evaluation was conducted between 2015 and 2017. The results of this evaluation are not endorsed by the federal government. These findings do not reflect the views of and may differ from the federal government’s evaluation.
[1] Awsumb, B., Dobbe, C., Ly-Xiong, S., Rodriguez-Hager, R., Rydrych, D., & Terrill, W. (October 2016). "Accountable Communities for Health: Perspectives on Grant Projects and Future Considerations." Retrieved from http://www.dhs.state.mn.us/main/groups/sim/documents/pub/dhs-290682.pdf