Blog & News
SHADAC Releases 50-State Analysis of the Evolving Opioid Crisis (Infographics)
February 11, 2019:Much of the attention paid to the national opioid crisis in recent years has focused on the national toll of the crisis, such as the more than 44,000 opioid overdose deaths reported nationally in 2017.[1] However, the dynamics of the crisis vary widely across states, both in the prevalence of opioid overdose deaths and the types of opioids associated with those deaths.
To make state-specific information on opioid overdose deaths more easily accessible, SHADAC has used estimates from our State Health Compare online data tool to create a set of two-page infographics for all 50 states and the District of Columbia that include new data on drug overdose deaths for 2017.
Additionally, because of growing concern and evidence that the opioid crisis may be expanding to other non-opioid illicit drugs, we also have included data on drug overdose deaths from two types of drugs that are commonly involved in opioid overdoses: cocaine and psychostimulants (such as methamphetamine). [2],[3]
HIGHLIGHTS
Background: U.S. trends in drug overdose deaths
At the national level, data on opioid overdose deaths show multiple, evolving phases of the overdose epidemic. From 2000 to approximately 2011, the growth in opioid overdose deaths was driven primarily by natural and semi-synthetic opioids (i.e., prescription opioid painkillers); but that death rate has since largely plateaued. Beginning around 2011, deaths from heroin began to increase more rapidly and were responsible for the highest overdose death rates in 2015. Since around 2013, however, deaths from synthetic opioids, such as fentanyl, have grown precipitously, and in 2017 the overdose death rate from synthetic opioids was nearly double the rate for all other drug types.
Around the same time that death rates from heroin and synthetic opioids began to increase, deaths from cocaine and psychostimulants also began to increase. Evidence suggests that this relationship is driven, at least in part, by an increase in deaths that involve multiple drugs. Since 2011, when deaths from heroin began to rise, death rates from cocaine have nearly tripled, from 1.5 per 100,000 people to 4.3 per 100,000 people in 2017; and death rates from psychostimulants have more than quadrupled, from 0.7 per 100,000 people to 3.2 per 100,000 people in 2017.
State variation in overdose deaths
Opioid Overdose Deaths
Although most states have experienced measurable increases in opioid overdose deaths since 2000, the scale of the crisis has varied widely across states. For example, West Virginia’s rate of deaths from synthetic opioids in 2017 was more than 30 times the rate of Nebraska and Texas (37.4 deaths versus 1.3 deaths per 100,000 people).
The types of opioids most commonly associated with overdoses also vary across states. For instance, Utah had the second-highest rate of deaths from natural and semi-synthetic opioids in 2017, at 10.0 deaths per 100,000 people; however, contrary to the U.S. trend, the state has experienced relatively little growth in deaths from synthetic opioids, and the state’s 2017 death rate from synthetic opioids (3.1 per 100,000 people), fell well below the U.S. rate of 9.0 per 100,000 people.
Overdose Deaths from Cocaine and Psychostimulants
The scale of overdose deaths from non-opioid illicit drugs also varies widely across states. For example, the 2017 overdose death rate from cocaine in the District of Columbia (17.6 deaths per 100,000 people) was 22 times the rate of Arkansas and Kansas (0.8 deaths per 100,000 people). Similarly, the 2017 overdose death rate from psychostimulants in West Virginia (13.6 deaths per 100,000 people) was more than 15 times the rate of 0.9 deaths per 100,000 people in New Jersey.
Regional Patterns in Drug Overdose Death Rates
Despite the evidence of state variation in drug overdose death rates, further analysis does illustrate some broader patterns:
Heroin and synthetic opioids
Death rates from heroin and synthetic opioids are generally higher east of the Mississippi River, particularly among states in the Northeast, the Appalachian region, and the industrial Midwest.
Natural and semi-synthetic opioids
Higher death rates from natural and semi-synthetic opioids are more geographically dispersed than those from heroin and synthetic opioids. While some states in the eastern U.S. have particularly high rates of deaths from natural and semi-synthetic opioids (e.g., Kentucky, Ohio, and West Virginia), there are other states in the western U.S. that also have similarly high death rates from these drugs (e.g., Utah, New Mexico, and Nevada).
Cocaine
An examination of cocaine death rates reveals a pattern similar to that of death rates from heroin and synthetic opioids, with states east of the Mississippi River exhibiting higher rates of cocaine overdose deaths.
Psychostimulants
Death rate patterns from psychostimulants appear to be almost the opposite of those for heroin and synthetic opioids, with relatively low death rates in the Northeast and particularly high rates of deaths in the western U.S. and the Southeast. Only a group of three state—Kentucky, Ohio, and West Virginia—shows strong overlaps between psychostimulant and heroin and synthetic opioid deaths.
Access the state-level infographics on drug overdose deaths.
Explore the data on drug overdose deaths on State Health Compare.
Further Reading and Resources
New Data on Drug Overdose Death Highlight the Need for State-Level Analysis
SHADAC Blog, December 2018
Exploring the New State-Level Opioid Data on SHADAC’s State Health Compare
SHADAC Webinar (Recording and Presentation Materials), September 2018
The Changing Opioid Epidemic: State Trends, 2000-2016
SHADAC Blog, August 2018
The Changing Opioid Epidemic: National Trends, 2000-2016
SHADAC Blog, July 2018
The Opioid Epidemic: National and State Trends in Opioid-Related Overdose Deaths, 2000-2016
SHADAC Issue Briefs, June 2018
[1] This number includes deaths from natural and semi-synthetic opioids (e.g., prescription opioid painkillers), heroin and synthetic opioids (e.g., fentanyl), but it excludes some opioids with relatively fewer deaths, such as methadone.
[2] Although reports of illicit drugs being tainted with synthetic opioids are relatively common, it is unclear whether deaths involving multiple drugs are typically the result of drugs being intentionally mixed by or unintentionally contaminated through traffickers’ sloppiness, or because individual drug users are concurrently abusing multiple different drugs of their own volition.
[3] U.S. Centers for Disease Control and Prevention. (2018, December 12). Drugs Most Frequently Involved in Drug Overdse Deaths: United States, 2011-2016. National Vital Stastics Report, 67(9), 1-14. Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_09-508.pdf
Publication
Leveraging 1332 State Innovation Waivers to Stabilize Individual Health Insurance Markets: Experiences of Alaska, Minnesota, and Oregon (Final Report)
 In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key requirements under the law in order to experiment with different policies in the individual and small group insurance market within certain guardrails. A new SHADAC analysis, prepared for the Robert Wood Johnson Foundation, examines the use of 1332 State Innovations Waivers to stabilize individual health insurance markets within these states. SHADAC researchers compared the use of this strategy in Alaska, Minnesota, and Oregon, assessing how the 1332 waiver process was navigated; identifying lessons learned about this process and about different reinsurance models; and pinpointing future concerns about the use of reinsurance programs.
In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key requirements under the law in order to experiment with different policies in the individual and small group insurance market within certain guardrails. A new SHADAC analysis, prepared for the Robert Wood Johnson Foundation, examines the use of 1332 State Innovations Waivers to stabilize individual health insurance markets within these states. SHADAC researchers compared the use of this strategy in Alaska, Minnesota, and Oregon, assessing how the 1332 waiver process was navigated; identifying lessons learned about this process and about different reinsurance models; and pinpointing future concerns about the use of reinsurance programs.
SHADAC conducted an in-depth document review and qualitative interviews with individuals - including state agency and executive staff, legislators, actuarial analysts, health plan representatives, program administrators, and other stakeholders - across the three study states who were involved in the design and/or implementation of state reinsurance programs and the 1332 waiver application process. Each of the states faced numerous challenges in their individual health insurance markets (high costs, increasing premiums, shifting marketplace makeup and plan availability, etc.) that led them to establish state-based reinsurance programs. However, as the report details, state policymakers found unique ways to facilitate both the waiver application and implementation processes, including working hand-in-hand with insurance companies, leveraging existing infrastructure and experience within their own agencies, having mechanisms in place to get analysis done quickly, and engaging with the state’s congressional delegation.
Alaska, Minnesota, and Oregon: Reinsurance Models
In 2017, Alaska, Minnesota, and Oregon became the first three states to receive federal approval to establish state reinsurance programs with federal funding via section 1332 State Innovation Waivers, which authorize states to waive key ACA requirements in order to experiment with different policies in the individual and small group insurance market within certain guardrails.
- Alaska’s state reinsurance program is condition-based, paying 100% of claims from policyholders who have one of 33 possible specific medical conditions.
- The Minnesota Premium Security Plan (MPSP) is a traditional reinsurance model with an attachment point of $50,000 and a cap of $250,000 with payment of claims at an 80/20 coinsurance rate.
- The Oregon Reinsurance Program is a traditional reinsurance model with a 50/50 coinsurance rate, as well as an attachment point and cap to be determined at a later date.
Challenges and Facilitators of the 1332 Waiver Application Process
Interviewees across all stated noted numerous challenges during the 1332 waiver application process, including:
- Securing a state funding source
- Navigating rapid shifts in the political climate that affected the application process
- Being able to access timely data to support their applications
- Identifying a waivable requirement of the ACA
Respondents agreed, however, on common facilitators that aided the application process, which they listed as:
- Working hand-in-hand with insurance companies to keep them in the market
- Leveraging existing infrastructure and experience to support the state-based programs
- Using previously existing mechanisms to get analysis done quickly
- Engaging with the state’s congressional delegation
Lessons Learned about 1332 Waiver Application and Implementation Processes
Interview respondents also identified a number of lessons learned by the states as they navigated both the application and implementation stages for their 1332 waivers. A few key points are listed below.
- There are both pros and cons to condition-based vs. traditional reinsurance models.
States noted that they chose reinsurance models that would be easy to implement in a short timeframe. Traditional models were less complex, but condition-based models maximized cost of care options. - Robust communication efforts with multiple stakeholders were needed.
Respondents consistently emphasized the need for dedicated communication between state agencies, legislators, health insurers, congressional delegations, CMS officials, and community stakeholders in order to put together a successful waiver application. - Microsimulation models allowed states to be responsive to rapidly shifting policies.
States were required to submit actuarial and economic analyses as part of their waiver applications, and the microsimulation models used by Alaska and Oregon allowed them to respond to several real-time policy changes (such as the repeal of the individual mandate).
Future Concerns
Though respondents in all three states felt that state-based reinsurance was necessary to help stabilize the markets, they did report a number of concerns for the future of these programs.
- It is difficult to measure the impact of reinsurance programs beyond premium rates.
All three states reported a reduction in premium costs in the individual market as a result of implementing a reinsurance program, but other evaluations of program impacts have not been clear, often due to lack of data. - No accountability measures were included.
Due to the short turnaround time to both apply for and implement their 1332 waivers, none of the study states included accountability measures within their reinsurance programs for the individual market. - Reinsurance is only a short-term fix and does not address the underlying problem of health care costs.
Although interviewees from Alaska, Minnesota, and Oregon felt that state-based reinsurance was an important tool to stabilize the individual market, all questioned the viability of such programs as a long-term solution, commenting that individual marketplaces were only part of the whole, and only when the larger picture is addressed can the root of the issue of high health care cost be properly addressed.
Related Readings and Resources
Modeling State-based Reinsurance: One option for Stabilization of the Individual Market
Minnesota’s 13332 Reinsurance Waiver Dilemma
Resource: 1332 State Innovation Waivers for State-Based Reinsurance
Publication
Housing Affordability Matters: Measuring and Addressing the Burden of Unaffordable Rents (Infographics)
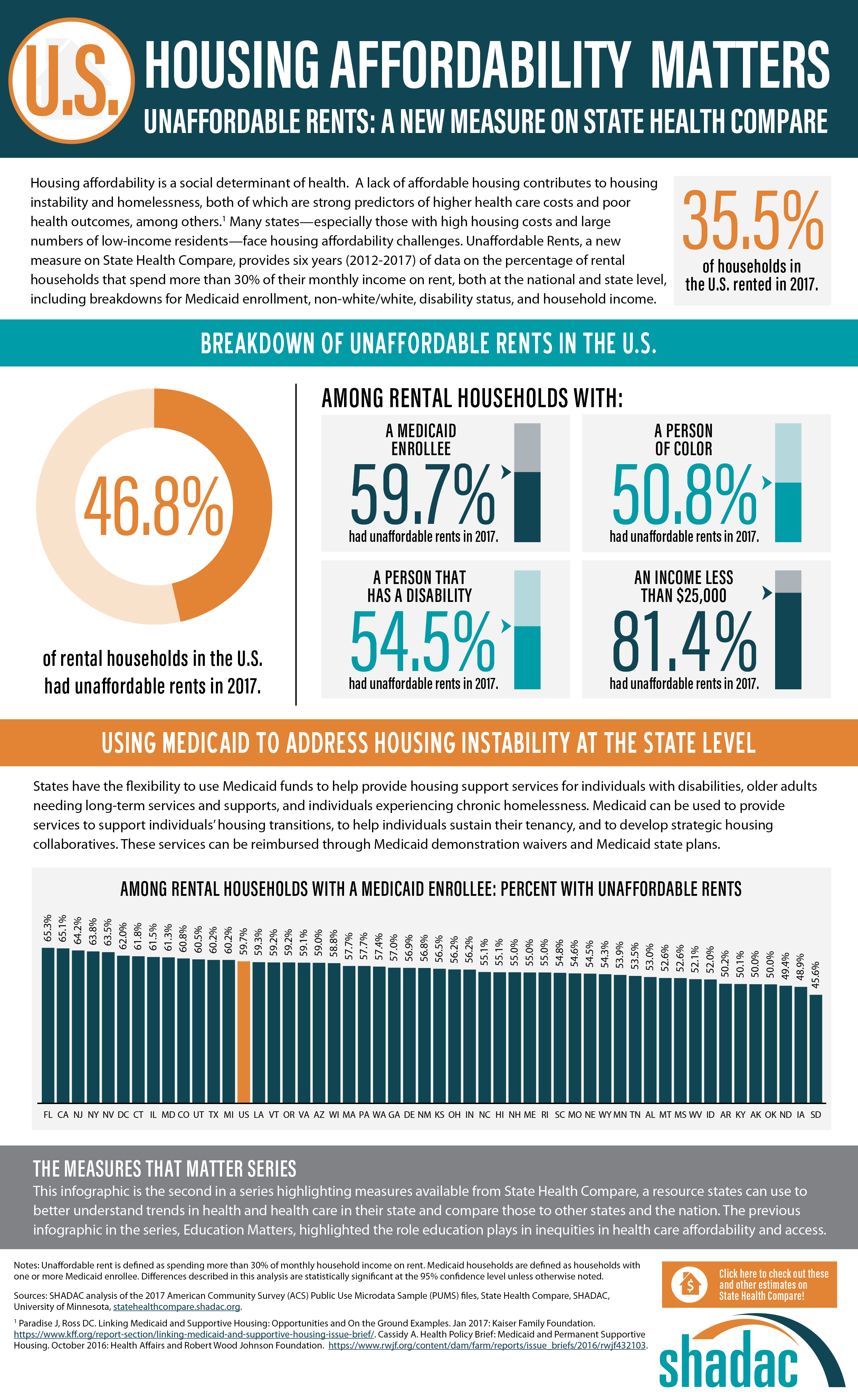
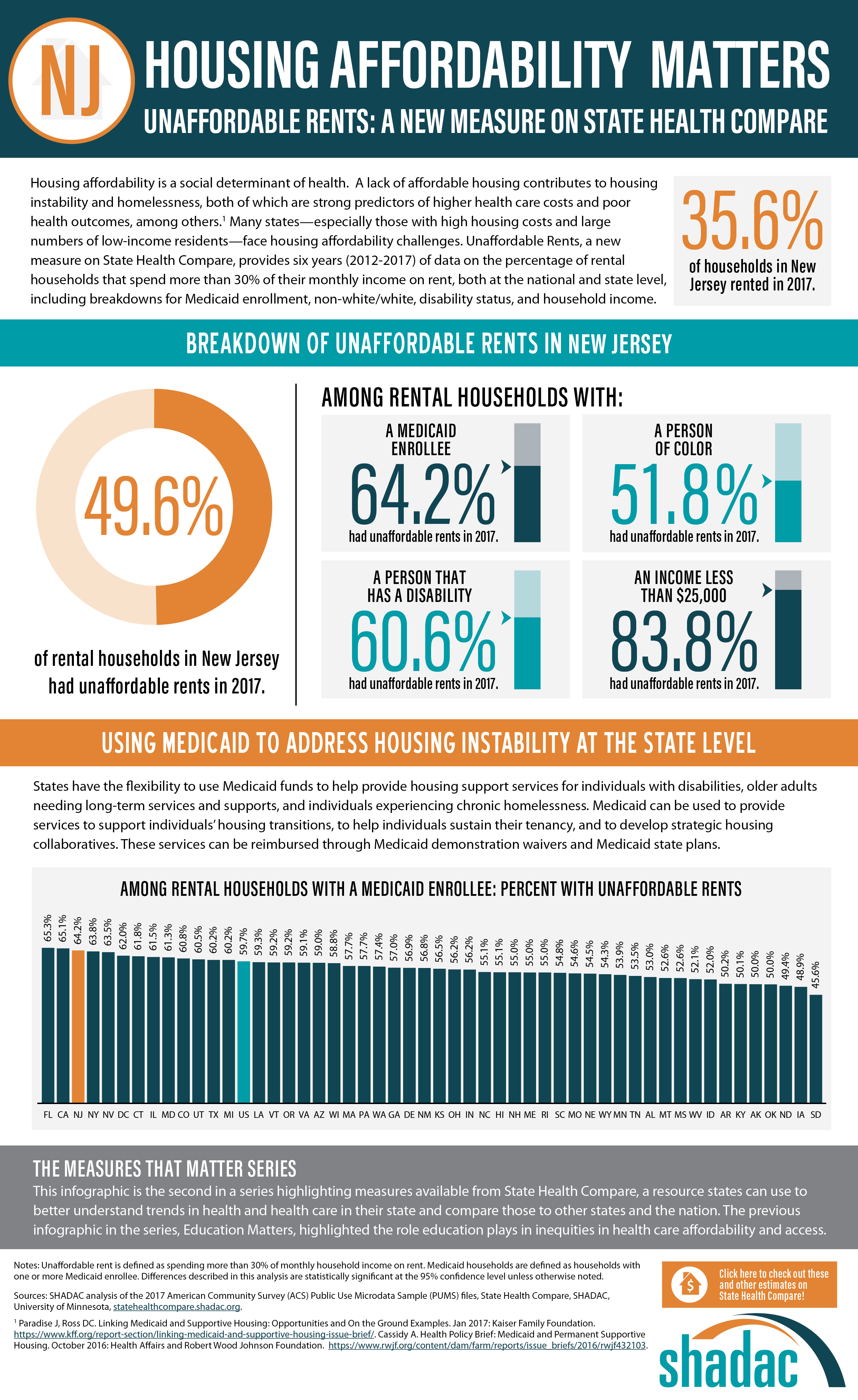
An analysis by SHADAC examines housing affordability, looking specifically at the percent of rental households that spend more than 30% of their monthly income on rent. This measure is now available on SHADAC’s State Health Compare for all states from 2012 through 2017, and can be broken down by household income, Medicaid enrollment, race/ethnicity, and disability status.[1]
Background
SHADAC analyzed a key social determinant of health factor—housing affordability. A lack of affordable housing contributes to housing instability and homelessness, both of which are strong predictors of higher health care costs and poor health outcomes, among others.[2] Many states—especially those with high housing costs and large numbers of low-income residents—face housing affordability challenges.
Breaking Down the Issue of Unaffordable Rents
SHADAC looked at the percent of cost-burdened rental households in each state in 2017, examining unaffordable rents overall while also analyzing unaffordable rents among rental households with: a Medicaid enrollee, a person of color, a person that has a disability, and an income of less than $25,000. The infographic presented here shows these estimates for the U.S. SHADAC researchers have also created state infographics for the five states with the highest percentages of unaffordable rents among rental households that had a Medicaid enrollee—Florida (65.3%), California (65.1%), New Jersey (64.2%), New York (63.8%), and Nevada (63.5%).
Discussion: How State Medicaid Policy Can Alleviate the Burden of Unaffordable Rents
Since recent attention has been given to the idea of using Medicaid to address housing instability at the state level, the rate of unaffordable rents among rental households with Medicaid enrollees (59.7% nationally) is a particularly salient estimate, indicating that a substantial portion of this population could benefit from such efforts.
Though federal law directly prohibits federal-level matching of state Medicaid spending on housing (excepting nursing home facilities, which are already specified as a Medicaid coverage benefit), states can use Medicaid demonstration waivers and State Plan Amendments to leverage federal dollars for a wide range of housing-related services and activities, including support services for individuals with disabilities, older adults needing long-term services and supports, and individuals experiencing chronic homelessness. Medicaid can also be used to provide services to support individuals’ housing transitions, to help individuals sustain their tenancy, and to develop strategic housing collaboratives. In addition, several states, in an effort to integrate their separate yet related Medicaid and housing programs, have begun to reorganize part or all of their Medicaid delivery systems into accountable care organizations (ACOS) for more ease in using Medicaid dollars for non-medical “flexible services,” which include housing supports.[3]
Visit SHADAC and State Health Compare for More
The infographics presented here are part of SHADAC’s “Measures That Matter” product series. This series highlights measures available from State Health Compare, a web tool that states can use to explore measures related to health and health care within and across states and the nation.
The previous infographics in the series, “Education Matters,” highlighted the role education plays in inequities in health care affordability and access. Learn more about this analysis here.
Learn more about the estimates used in this analysis, as well as other measures related to social determinants of health, at State Health Compare.
[1] SHADAC. Analysis of the 2017 American Community Survey (ACS) Public Use Microdata Sample (PUMS) files. State Health Compare. statehealthcompare.shadac.org.
[2] Cassidy A. (2016). Health Policy Brief: Medicaid and Permanent Supportive Housing. Health Affairs and Robert Wood Johnson Foundation. https://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf432103.
[3] Paradise J, Ross DC. (2017). Linking Medicaid and Supportive Housing: Opportunities and On the Ground Examples. Kaiser Family Foundation. http://files.kff.org/attachment/Issue-Brief-Linking-Medicaid-and-Supportive-Housing-Opportunities-and-On-the-Ground-Examples.
Publication
Assessment and Synthesis of Selected Medicaid Eligibility, Enrollment, and Renewal Processes and Systems in Six States
 This SHADAC contractor report was produced for the Medicaid and CHIP Payment and Access Commission (MACPAC). The purpose of the analysis was to examine Medicaid eligibility, enrollment, and renewal practices in six states in light of the Affordable Care Act goals of making the Medicaid program more efficient; reducing complexity and effort for enrollees and program administrators; and integrating Medicaid with the health insurance exchanges. The report summarizes how MAGI Medicaid populations apply to and are determined eligible for the Medicaid program in the study states, and it describes the study states’ approaches to streamlining enrollment and renewal for these populations, common themes among the states, and the states’ future plans to further streamline enrollment and renewal.
This SHADAC contractor report was produced for the Medicaid and CHIP Payment and Access Commission (MACPAC). The purpose of the analysis was to examine Medicaid eligibility, enrollment, and renewal practices in six states in light of the Affordable Care Act goals of making the Medicaid program more efficient; reducing complexity and effort for enrollees and program administrators; and integrating Medicaid with the health insurance exchanges. The report summarizes how MAGI Medicaid populations apply to and are determined eligible for the Medicaid program in the study states, and it describes the study states’ approaches to streamlining enrollment and renewal for these populations, common themes among the states, and the states’ future plans to further streamline enrollment and renewal.
Individual Case Study Reports
- Eligibility, Enrollment, and Renewal: Arizona Case Study Findings
- Eligibility, Enrollment, and Renewal: Colorado Case Study Findings
- Eligibility, Enrollment, and Renewal: Florida Case Study Findings
- Eligibility, Enrollment, and Renewal: Idaho Case Study Findings
- Eligibility, Enrollment, and Renewal: New York Case Study Findings
- Eligibility, Enrollment, and Renewal: North Carolina Case Study Findings
About the Study
SHADAC’s study sought to both understand how the selected states—with varied Medicaid policy, program priorities, and ages and capabilities of their eligibility systems—enacted different approaches to streamlining their Medicaid enrollment and renewal processes for individuals whose income eligibility is based on Modified Adjusted Gross Income (MAGI), and to assess the extent to which states were achieving desired goals such as program efficiency and a simplified beneficiary experience.
SHADAC used a multi-case study methodology and key informant interviews with 48 individuals representing state and local agencies and advocacy organizations to collect data on eligibility, enrollment, and renewal processes and systems for MAGI Medicaid populations. MACPAC was specifically interested in auto-enrollment and auto-renewal practices for MAGI Medicaid, the use of electronic data sources to verify beneficiary information, and the degree to which MAGI Medicaid enrollment and renewal is integrated with enrollment and renewal for non-MAGI Medicaid and other public benefit programs. SHADAC found that some states prioritized real-time, no-touch enrollment and renewal, while others prioritized eligibility worker involvement. All study states, however, focused on the transition to MAGI-based eligibility determinations and the use of electronic data sources to verify beneficiary information called for under the ACA.
Key Themes
Interview responses across the six states revealed several key themes related to Medicaid program and beneficiary experiences:
- Multi-benefit online applications enhanced beneficiary access to programs and reduced burden, but back-end eligibility systems are complicated to maintain.
- Electronic data interfaces facilitated high rates of real-time eligibility determinations, auto-renewal, and reduced churn.
- Robust rules engines were critical to support successful streamlined eligibility determinations, but workers still need to understand policy.
- Complex and varied program rules remained a challenge for integration of MAGI Medicaid and other programs.
- Despite streamlined application processes, demand for enrollment assistance was high.
Areas of Ongoing Activity
The work of study states to accurately and efficiently enroll and renew Medicaid eligible populations into the program is not static, but rather focused on continuous improvement over time. Areas of ongoing activity include the following:
- Monitoring of Medicaid and related policy changes continues. Respondents were closely monitoring potential Medicaid policy changes in their states, such as Medicaid expansion proposals in Idaho and proposed Medicaid work requirements in Arizona.
- Efforts to improve beneficiary and inter-agency correspondence are important and ongoing. Four of the study states (Arizona, Colorado, Florida, New York) reported beneficiary confusion arising from correspondence about eligibility determination and renewal, and three of these states (Colorado, Florida, New York) reported plans to improve this correspondence. Half the study states also reported ongoing efforts to improve inter-agency correspondence as well.
- States continue to invest staff resources and funding to improve application and eligibility system infrastructure. All six states are currently working to increase the usability of their application platforms and enhance their eligibility systems—shifting away from legacy mainframe systems toward rules-based systems and modular, cloud-based platforms.
Related Content: MACPAC Summary Issue Brief
Publication
Eligibility, Enrollment, and Renewal: North Carolina Case Study Findings
 SHADAC produced this case study for the Medicaid and CHIP Payment and Access Commission (MACPAC) as part of a contract to examine Medicaid eligibility, enrollment, and renewal practices in six states in light of the Affordable Care Act goals of making the Medicaid program more efficient; reducing complexity and effort for enrollees and program administrators; and integrating Medicaid with the health insurance exchanges.
SHADAC produced this case study for the Medicaid and CHIP Payment and Access Commission (MACPAC) as part of a contract to examine Medicaid eligibility, enrollment, and renewal practices in six states in light of the Affordable Care Act goals of making the Medicaid program more efficient; reducing complexity and effort for enrollees and program administrators; and integrating Medicaid with the health insurance exchanges.
This case study presents findings from telephone interviews with key respondents in North Carolina, conducted in May and June of 2018. The report summarizes how MAGI-Medicaid populations apply to and are determined eligible for the Medicaid program in North Carolina, and describes Northa Carolina’s approach to streamlining enrollment and renewal for these populations, Medicaid program and beneficiary experiences, and the state's future plans to further streamline enrollment and renewal.
Download a PDF of the case study.
Related Content: Synthesis Report
Related Content: Individual Case Study Reports
- Eligibility, Enrollment, and Renewal: Arizona Case Study Findings
- Eligibility, Enrollment, and Renewal: Colorado Case Study Findings
- Eligibility, Enrollment, and Renewal: Florida Case Study Findings
- Eligibility, Enrollment, and Renewal: Idaho Case Study Findings
- Eligibility, Enrollment, and Renewal: New York Case Study Findings
Related Content: MACPAC Summary Issue Brief