SHADAC Expertise
Medicaid and CHIP Policy
SHADAC has worked both independently and under contract to the Robert Wood Johnson Foundation (RWJF) and the Medicaid and CHIP Payment Access Commission (MACPAC) to monitor and analyze changes in the Medicaid and CHIP policy landscape such as Medicaid expansion, eligibility, enrollment, and renewal, quality measurement, as well as states’ waiver application, implementation, and evaluation. SHADAC faculty and staff have exceptional knowledge of Medicaid and CHIP, including knowledge from the perspective of state policymakers and program administrators, as well as operational issues at the federal and state levels.
Related SHADAC work
Click on any title below to learn more about the project.
Tracking the Data on Medicaid’s Continuous Coverage Unwinding (State Health & Value Strategies)
A lack of publicly available data on Medicaid enrollment, renewal, and disenrollment makes it difficult to understand exactly who is losing Medicaid coverage and for what reasons. This issue brief lays out a phased set of priority measures and provides a model enrollment and retention dashboard template that states can use to monitor both the short-term impacts of phasing out public health emergency (PHE) protections and continuous coverage requirements, as well as longer-term enrollment and retention trends. Through its work with SHVS, SHADAC also published a series of issue briefs that tracked through an interactive map the format of state reporting of unwinding data, state-based marketplace transition data (i.e. people who no longer qualify for Medicaid but might be eligible for a qualified health plan offered through the marketplace), and Medicaid unwinding reinstatement data.
Supporting BDT’s Stabilizing Medicaid Enrollment Learning Collaborative
SHADAC collaborated with a new partner, Benefits Data Trust (BDT), on a small project to design and lead a webinar for its Medicaid Churn Learning Collaborative participants on the topic of monitoring and evaluation. The webinar took place as state Medicaid agency participants were implementing activities to redetermine all individuals enrolled in Medicaid and were meeting federal reporting requirements to monitor the end of the continuous coverage provisions.
Tracking Health Insurance Coverage During the Unwinding: Monthly Data from the Household Pulse Survey
The unwinding of the Medicaid continuous coverage requirement ("Medicaid Unwinding") represents the largest nationwide coverage transition since the Affordable Care Act. Since February 2020, enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) has increased by 23 million enrollees. Not only that, but analysis also indicates that as many as 15 million individuals will exit Medicaid to other coverage or become uninsured. Lack of publicly available data on Medicaid enrollment, renewal, and disenrollment makes it difficult to track the phenomenon of the 'Medicaid Unwinding'. As states “unwind” the Medicaid continuous coverage requirement and restart standard redetermination procedures, SHADAC researchers are using data from the U.S. Census Bureau’s Household Pulse Survey (HPS) to track trends in health insurance coverage rates. See our findings and frequent updates here.
Past Work
Assessment and Synthesis of Selected Medicaid Eligibility, Enrollment, and Renewal Processes and Systems in Six States
SHADAC worked as a contractor for the Medicaid and CHIP Payment Access Commission (MACPAC) to conduct an assessment of Medicaid eligibility, enrollment, and renewal processes and systems in six study states—Arizona, Colorado, Florida, Idaho, New York, and North Carolina. Utilizing a multi-case study methodology as well as key informant interviews with state and local agency staff and advocacy organizations, SHADAC collected and synthesized data on Medicaid enrollment processes and systems for individuals whose income eligibility is based on Modified Adjusted Gross Income (MAGI) in order to assess the extent to which states were achieving desired goals such as program efficiency and a simplified beneficiary experience. As a follow up, SHADAC identified the risks that remain for both individuals and state agencies that cause eligible individuals to remain uninsured or lose Medicaid coverage and conducted interviews with key stakeholders nationally and in four states to obtain additional input on potential risk points and strategies to improve eligibility determination and renewal accuracy.
SHADAC Advocates a Data-based Approach to Advancing Medicaid and CHIP Access Monitoring Plan
On February 17, 2022, the Centers for Medicare & Medicaid Services (CMS) released a request for information (RFI) regarding access to coverage and care in Medicaid and the Children’s Health Insurance Program (CHIP). SHADAC researchers focused our response on Objective 4: Question 1, which asked researchers to consider how CMS might develop a stronger Medicaid and CHIP access monitoring approach through data reporting and analysis. These comments are based on SHADAC’s experience providing data and evaluation technical assistance (TA) to states, and mirror recent testimony to the Medicaid and CHIP Payment Access Commission (MACPAC) provided by SHADAC’s Deputy Director.
Addressing Social Determinants of Health through Behavioral Health-focused 1115 Waivers: Implementation Lessons from Three States
Through the Robert Wood Johnson Foundation’s (RWJF) “Research in Transforming Health” program, SHADAC researchers conducted a study to understand how three states—Illinois, Texas, and Washington—were addressing the needs of justice-involved populations through implementation of Section 1115 Medicaid waiver programs. The specific aim of the study was to identify promising practices and lessons learned related to the development, implementation, and management of these innovative behavioral health policies with the purpose of informing policy development in states considering similar 1115 waivers.
SHADAC Expertise
State and Federal Health Policy and Strategies
Our faculty and staff are nationally recognized experts on collecting and applying sound data to inform public health, health care reform strategies, federal healthcare policy, and health policy decisions at both the state and federal levels. We rely on both qualitative and quantitative data sources to identify and frame policy options and bring long-standing qualifications in tapping federal survey data sources. We provide direct technical assistance to individual states, create forums to support state-to-state peer learning, and more broadly conduct targeted research and policy analysis as well as translate technical information into content that is accessible and informative to decision-makers.
Related SHADAC work:
Click on any title below to learn more about the project.
State Health & Value Strategies Technical Assistance
SHADAC provides technical assistance as part of the Robert Wood Johnson Foundation’s (RWJF's) State Health & Value Strategies (SHVS), a program that connects state officials with experts in the field to support them in transforming their health care systems to be affordable, equitable, and innovative. SHADAC provides analytic and evaluation support with the goal of helping states use sound data to inform policy decisions on topics such as Medicaid, state health policy, federal healthcare policy, health equity, multi-payer delivery system and payment reform, quality measurement, coverage and access expansions, health insurance exchanges, and population health. Recent work has focused on the unwinding of the Medicaid continuous coverage requirement, where SHADAC has worked closely with several states to model the enrollment impacts of unwinding. Another ongoing area of support is helping state agencies improve the quality and collection of enrollee demographic data (e.g. race, ethnicity, language, disability, sexual orientation and gender identity) with a goal of improved health equity programming. This is done both by working with states one-on-one, but also through a peer-learning group aimed at discussing specific operational challenges related to data collection, coding and analysis.
State-Based Reinsurance Programs via 1332 State Innovation Waivers
SHADAC maintains a frequently updated resource highlighting state reinsurance policies passed using a 1332 waiver. This information is presented in an interactive map that provides an overview of the different stages of states' 1332 waiver reinsurance applications.
Public Health Implications of Cannabis Policy in Minnesota
SHADAC and the University of Minnesota’s Cannabis Research Center (CRC) have released a brief using data from the National Survey on Drug Use and Health (NSDUH) to understand issues related to public health implications of Minnesota cannabis use prior to its 2023 legalization. Along with providing key background information and context on cannabis policy in the United States, this brief specifically examines three oft cited concerns with cannabis legalization: the prevalence of cannabis use; cannabis abuse and dependence (i.e., addiction); and driving under the influence of cannabis. The data in this brief are intended to serve as starting points for discussions on the public health impacts of Minnesota cannabis policy. Read the brief in full here along with this accompanying blog post.
Minnesota Long-Term Services and Supports: Demographics Report, Future Utilization & Payments, Projection Model
Lynn Blewett, founding Director of SHADAC, worked alongside researchers at Purdue University to author a report on utilization, cost, and demographics of populations that use Long-Term Services and Supports (LTSS) in Minnesota. This was conducted as part of a larger study, Own Your Future 3.0: Planning for Minnesotans’ LTSS Needs, sponsored by Minnesota’s Department of Human Services, Aging and Adult Services Division. SHADAC researchers and collaborators on this project worked towards the objectives of studying current and future use of Long-Term Services and Supports (LTSS) for older Medicaid enrollees and the general older population in Minnesota, describing LTSS service utilization and expenditures for Minnesota’s older population in 2016-2021, and estimating future Medicaid LTSS utilization and expenditures using demographic data, areas of need, and other information. SHADAC has also collaborated with the Minnesota Department of Human Services to develop a model estimating future Medicaid utilization and spending in Minnesota for long-term services and supports (LTSS). The spreadsheet model leveraged data from the American Community Survey (ACS), the state’s Medicaid Management Information System (MMIS), and the state’s Survey of Older Minnesotans to define current Medicaid cohorts and use, calculate projections of future eligibility, and delineate predictors of LTSS service use under different economic and policy assumptions.
Past Work
Leveraging 1332 State Innovation Waivers to Stabilize Individual Health Insurance Markets
Funded by the Robert Wood Johnson Foundation (RWJF), SHADAC researchers documented the strategies and rationale of the first three states to receive federal approval to establish state reinsurance programs with federal funding—Alaska, Minnesota, and Oregon—via Section 1332 State Innovation Waivers in order to address the volatility of their individual health insurance markets. SHADAC identified challenges, facilitators, and lessons learned during the waiver application and implementation processes that could be helpful for states considering similar state health policy action and for federal regulators interested in supporting similar state initiatives.
Strategies to Increase Access to Medications for Opioid Use Disorder during the COVID-19 Pandemic and Beyond
SHADAC researchers, along with Hennepin Healthcare researcher Tyler Winkelman, authored a Milbank Foundation policy brief that examines the federal healthcare policy and state policy changes put in place to improve access to medications for opioid use disorder (MOUD) during the COVID-19 pandemic, during which time MOUD became especially challenging to access because MOUD patients are typically required to have as many as six in-person clinic visits a week. The authors conclude with federal and state policy recommendations based on their analysis.
Assessment of State Health Information Exchange Policy
On behalf of the Connecticut Health Foundation, SHADAC authored a policy brief exploring the launch of a new statewide health information exchange (HIE)—the Health Information Alliance— in Connecticut. In addition to providing context for the state’s new HIE, the brief also offers an overview of the current landscape in Connecticut related to information exchange and describes opportunities and potential obstacles going forward, such as the need for robust provider participation, provision of incentives to ensure participation, and the development of a long-term funding and patient engagement strategy. To inform this work, SHADAC researchers conducted a review of select national and state literature and organized interviews with key stakeholders both in Connecticut and in other states that are further along with statewide HIE efforts, with the goal of helping policymakers and those interested in patient care and population health understand where the state is today, what’s coming, and what to consider for success.
Blog & News
New Report for Connecticut Explores “What’s Happening with Health Information Exchange in the State”
November 25, 2019:Under contract with the Connecticut Health Foundation, SHADAC Senior Researchers Christina Worrall, MPP, and Emily Zylla, MPH, have authored a new policy brief exploring the launch of a new statewide health information exchange in Connecticut—called the Health Information Alliance—and the next steps and key questions to ask to ensure success.
About the Report
A long-time goal for Connecticut (and many other states) has been the development of a secure way to effectively share up-to-date patient information electronically between providers. In forming a new, statewide non-profit health information exchange (HIE), Connecticut plans to connect providers and disparate health information exchange networks in order to reduce fragmentation. The new HIE will allow authorized users to see where and when individual patients have received care, which could help improve care coordination and quality and reduce duplicative tests. In addition, the new health information exchange will be able to use the data from multiple sources to identify and analyze health outcomes and population health trends, which could both help meet the requirements of new care delivery and payment approaches as well as pinpoint and address health disparities.
In addition to providing context for the state’s new HIE, the brief also offers an overview of the current landscape in Connecticut related to information exchange and describes opportunities and potential obstacles going forward, such as the need for robust provider participation, provision of incentives to ensure participation, and the development of a long-term funding and patient engagement strategy. To inform this work, SHADAC researchers conducted a review of select national and state literature and organized interviews with key stakeholders both in Connecticut and in other states that are further along with statewide HIE efforts with the goal of helping policymakers and those interested in patient care and population health understand where the state is today, what’s coming, and what to consider for success.
Access the “Connecting Connecticut: What’s Happening with Health Information Exchange in the State” brief in full to read and download the latest on HIE.
Publication
The Art of Listening: Working with an Advisory Committee to Improve Outreach and Communication to Reach the Remaining Uninsured in Minnesota
Presentation by Brett Fried at the 2019 ACS Data Users Conference. May 15, 2018 in Washington, D.C.
Blog & News
Measuring Health Care Affordability with State Health Compare: Trouble Paying Medical Bills
June 18, 2019:The cost of health care continues to grow nationwide, with U.S. health care spending reaching $3.5 trillion, or an average of $10,739 per person, in 2017.[1] As these expenditures have grown, the cost of health insurance has grown as well, such that Americans are increasingly enrolling in health plans with large deductibles and other cost sharing in order to avoid the expense of rising premiums. Rising enrollment in these health plans, combined with the ongoing problem of “surprise medical bills” (bills from providers who are out of network unbeknownst to consumers) across all plan types, has increased the health care cost burden for many Americans and has drawn increasing attention to the affordability of health care for consumers.[2]
Exploring Health Care Affordability at the State Level with State Health Compare
SHADAC’s State Health Compare includes a measure “Had Trouble Paying Medical Bills” that assesses changes and patterns in health care affordability across the country by tracking the percent of Americans that had difficulty paying off medical bills or that were paying off medical bills over time. The measure is available at both the state and national level for 2011-2016 and can be broken down by age and insurance coverage type.
This post highlights states that experienced changes in the percent of residents by age that had trouble paying medical bills between 2015 and 2016 and shows the substantial amount of variation across states on this measure.
Trouble paying medical bills among the states, 2015-2016: Some rate increases, no decreases
Nationally, the percent of nonelderly adults (age 19-64) reporting trouble paying medical bills increased from 29.2% in 2015 to 31.3% in 2016 (2.1 points). This pattern was mirrored among children (age 0-18), who experienced an increase of 2.8 points, from 32.5% in 2015 to 35.3% in 2016.
Eight states experienced statistically significant increases in the share of nonelderly adults reporting trouble paying medical bills between 2015 and 2016, as shown below. Montana had the largest increase at 11.4 points (from 28.0% in 2015 to 39.4% in 2016), followed by Nevada at 10.4 points (from 18.2% to 26.8%), and New Hampshire at 7.4 points (from 26.8% to 34.2%). No state experienced a statistically significant decrease in the percent of non-elderly adults reporting trouble paying medical bills.
Among children, four states saw significant increases in the share reporting trouble paying medical bills, also shown below. The largest of these increases was in Arkansas, which experienced a rise of 18.0 points from 30.2% to 48.2% between 2015 and 2016. No state saw a significant decrease in the percent of children whose family reported trouble paying medical bills.
Among elderly adults (65+), only Alabama and Montana experienced significant increases in the share reporting trouble paying medical bills. Those states saw increases of 8.4 and 7.1 percentage points, respectively. No state saw a significant decrease in the percent of elderly adults reporting trouble paying medical bills.
2016: Large variation across states in percent with trouble paying medical bills
As shown below, there was substantial variation across states in 2016 in the percent that had trouble paying medical bills among nonelderly adults, children, and elderly adults. In general, states with median incomes registering below the national median[3] tend to have higher shares of residents reporting trouble paying medical bills, regardless of age group, and vice versa.
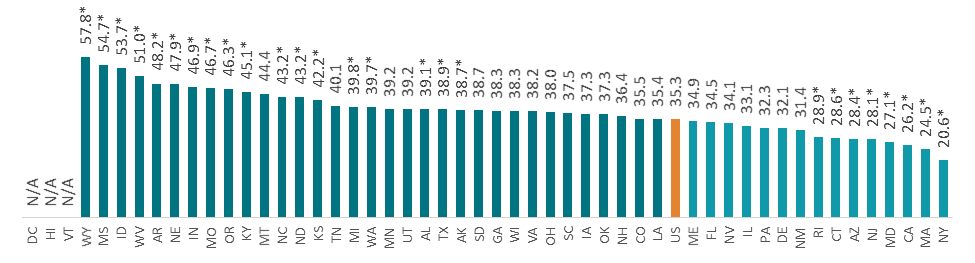
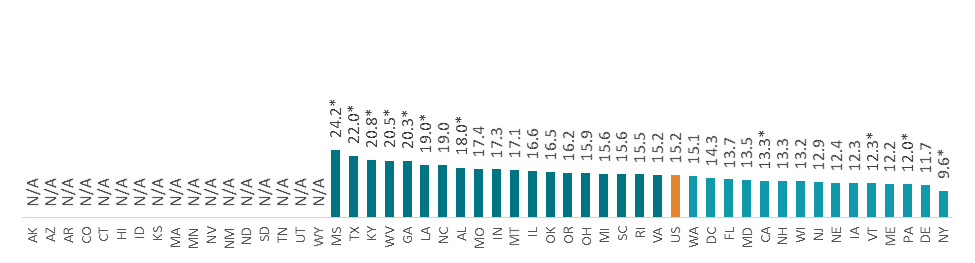
The percent of nonelderly adults who had trouble paying medical bills ranged from 13.3% in the District of Columbia to 49.0% in Mississippi (a difference of 35.7 points); the percent of children in families that had trouble paying medical bills ranged from 20.6% in New York to 57.8% in Wyoming (a difference of 37.2 points); and the percent of elderly adults who had trouble paying medical bills ranged from 9.6% in New York to 24.2% in Mississippi (a difference of 14.6 points).
Percent That Had Trouble Paying Medical Bills by State, 2016
Notes and Definitions
“Had Trouble Paying Medical Bills” is defined as the rate of individuals that had trouble paying off medical bills during past twelve months or were currently paying off medical bills among the civilian non-institutionalized population.
The source of the estimates is SHADAC analysis of NHIS data, National Center for Health Statistics (NCHS). The NHIS sample is drawn from the Integrated Health Interview Survey (IHIS, MN Population Center and SHADAC). Data were analyzed at the University of Minnesota's Census Research Data Center because state identifiers were needed to produce results and these variables were restricted.
Estimates were created using the NHIS survey weights, which are calibrated to the total U.S. Civilian non-institutionalized population for estimates broken down by age, and to the civilian non-institutionalized population age 18 to 64 for estimates broken down by coverage type.
Though SHADAC goes to great effort to produce as many state-level estimates as possible for our measures, due to sample size restrictions many state estimates of this measure are suppressed when broken down by subgroup. Namely, estimates are suppressed if the number of sample cases was too small or the estimate had a relative standard error greater than 30 percent.
Other State Health Compare estimates that use data from the NHIS
Had Trouble Paying Medical Bills is one of eight State Health Compare measures that SHADAC produces using data from the NHIS listed below. State Health Compare is the only source for state-level estimates of these measures.
- Made Changes to Medical Drugs
- Trouble Paying Medical Bills
- No Trouble Finding Doctor
- Told that Provider Accepts Insurance
- Had Usual Source of Medical Care
- Had General Doctor or Provider Visit
- Had Emergency Department Visit
- Spent the Night in a Hospital
[1] Centers for Medicaid & Medicaid Services (CMS). 2018. National Health Expenditure Data: Historical. Retrieved from https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html
[2] Pollitz, K. (2016, March 17). Surprise Medical Bills. Kaiser Family Foundation. Retrieved from https://www.kff.org/private-insurance/issue-brief/surprise-medical-bills/
[3] See U.S. Census Bureau, Table S1903. Median Income in the Past 12 Months (In 2016 Inflation-Adjusted Dollars): 2016 American Community Survey 1-Year Estimates. Retrieved from https://factfinder.census.gov/bkmk/table/1.0/en/ACS/16_1YR/S1903/0100000US|0100000US.04000
* Difference from the U.S. significant at the 95% confidence level
N/A indicates that data were suppressed because the number of sample cases was too small or the estimate had a relative standard error greater than 30%
Universe: Civilian non-institutionalized population
Source: SHADAC analysis of the National Health Interview Survey (NHIS) data, National Center for Health Statistics (NCHS)