Publication
Mental Health and Substance Use Disorder Parity under the ACA: National and State Estimates of Parity Gains as of 2017
 In addition to expanding access to health insurance coverage for millions of Americans through subsidized individual market coverage and state Medicaid expansions, the federal Affordable Care Act (ACA) applied Mental Health (MH) and Substance Use Disorder (SUD) coverage and parity mandates to beneficiaries in the individual and small-group markets and to Medicaid expansion beneficiaries. The following brief details the mechanisms by which the ACA applied these mandates and presents national and state-level estimates of the number of people with insurance coverage that must newly provide MH/SUD parity under the ACA. These estimates provide important context for policymakers and others engaged in the ongoing debate about repealing, modifying, or replacing the ACA.
In addition to expanding access to health insurance coverage for millions of Americans through subsidized individual market coverage and state Medicaid expansions, the federal Affordable Care Act (ACA) applied Mental Health (MH) and Substance Use Disorder (SUD) coverage and parity mandates to beneficiaries in the individual and small-group markets and to Medicaid expansion beneficiaries. The following brief details the mechanisms by which the ACA applied these mandates and presents national and state-level estimates of the number of people with insurance coverage that must newly provide MH/SUD parity under the ACA. These estimates provide important context for policymakers and others engaged in the ongoing debate about repealing, modifying, or replacing the ACA.
Background
Before the ACA, national legislation regarding equitable coverage for MH/SUD treatments applied only to large-group (i.e., employer-sponsored) health plans, as a result of the Mental Health Parity Act of 1996 (MHPA) and the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA). The ACA extended these MH/SUD parity protections beyond the large-group market to the individual and small-group markets and to Medicaid expansion beneficiaries by making MH/SUD treatments an essential health benefit (EHB). Before this change, coverage and parity for MH/ SUD treatment in these markets were addressed unevenly across states through a patchwork of state laws.
Expanding Equitable Coverage of Mental Health and Substance Use Disorder Treatment under the ACA: Key Provisions
Findings
Mental Health
In total, an estimated 39 million individuals nationwide had health insurance that was subject to the ACA’s expanded MH parity requirements as of 2017. Of these, 12.1 million were enrolled in individual plans, 14.4 million were enrolled in small-group plans, and almost 13 million were newly eligible Medicaid expansion enrollees.
At the state level, California saw the greatest number of individuals affected at approximately 8.6 million. Other states that had high estimates of affected populations included New York with 2.1 million, Florida with 2.08 million*, Texas with 1.9 million*, and Pennsylvania with 1.87 million.
Vermont, which had pre-ACA parity in both the individual and small-group market and had expanded Medicaid in advance of the ACA, was the only state that saw no effect. Other states such as Wyoming*, Alaska, and Delaware, all had affected populations of less than 100,000 (44,000; 67,000; and 80,000, respectively).
Substance Use Disorder
In total, an estimated 36.4 million individuals nationwide had health insurance that was subject to the ACA’s expanded SUD parity requirements as of 2017. Of these, 9.8 million were enrolled in individual plans, 14 million were enrolled in small-group plans, and almost 12 million were newly eligible Medicaid expansion enrollees.
At the state level, California saw the greatest number of individuals affected at approximately 8.26 million, followed by New York (2.09 million), Florida* (1.79 million), Pennsylvania (1.79 million) and Texas* (1.7 million).
Massachusetts, which had pre-ACA parity in both the individual and small-group market and had expanded Medicaid in advance of the ACA, was the only state that saw no effect. Other states such as Delaware, Wyoming*, Maine*, and Alaska all had affected populations of less than 100,000 (12,000; 39,000; 52,000; and 64,000, respectively).
Discussion
Though the ACA mandated access to health insurance coverage with parity for treatment of mental health and substance use disorders for new groups, it is important to note that the expansion of coverage parity legislation does not guarantee access to equitable MH/SUD services unless the legislation is enforced. Responsibility for parity enforcement falls primarily to states, and the nature and extent of enforcement is consequently inconsistent across the country, with many parity violations continuing to occur as state regulators face limitations in their enforcement capacities.
Further Reading
Access and Cost Barriers to Mental Health Care, by Insurance Status, 1999-2010
Kathleen Rowan, Donna McAlpine, and Lynn Blewett
Section 1115 Waivers and ACA Medicaid Expansions: A Review of Policies and Evidence from Five States: May 2016
SHADAC Special Issue Brief
Medicaid Expansion: Comparing State Choices in Alternative Benefit Plan Design
Colin Planalp
To learn more about mental health and state-level estimates for the affected population who report mentally unhealthy days, see our recent blog post, and visit State Health Compare to learn more about the measure and its data sources.
[1] National estimates do not include a Medicaid expansion breakdown because expansion has only occurred at the state level.
* No Medicaid expansion
Publication
The Comparing Health Insurance Measurement Error (CHIME) Study: Sample and Design
The aim of this report is to describe the CHIME study design and sampling strategy and to report matching and response rates.
About the CHIME Study
Because there is no comprehensive administrative record of health insurance coverage in the United States, we must rely on household survey reports to estimate the uninsurance rate and, in many cases, coverage type. Studies of the accuracy of reporting are needed to examine the validity of these survey estimates. The CHIME (Comparing Health Insurance Measurement Error) study is an experimental reverse-record check study that compared survey responses to administrative insurance records to understand the magnitude, direction, and patterns of misreporting in two important national surveys conducted by the U.S. Census Bureau. The study surveyed a stratified random sample of households known to have health insurance through one large regional insurer in the Midwest. Half of the sample was asked the health insurance module from the recently redesigned Current Population Survey Annual Social and Economic Supplement (CPS), and the other half received the health insurance module from the American Community Survey (ACS). CHIME provides the first post-health reform assessment of the validity of two national survey instruments in capturing health insurance coverage and its sources. CHIME also serves as the first baseline for validation across a range of public and private coverage types in the CPS redesign as well as the first validation study for the ACS.
Publication
Minnesota LTSS Projection Model: MN-LPM
Blog & News
MACStats from MACPAC: 2018 Medicaid and CHIP Data Book Now Available
February 1, 2019: The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released the 2018 version of its Medicaid and CHIP Data Book. This data book is a collection of federal and state statistics regarding the Medicaid and CHIP programs that are compiled by MACPAC from multiple data sources on key topic areas including Medicaid and CHIP eligibility, enrollment, and expenditures, as well as beneficiary health, service use, and access to care. An excellent resource, the data book draws on a wide variety of data sources including Medicaid administrative data (e.g., CMS-64 data, MSIS data, Medicaid Managed Care enrollment reports, etc.) as well as federal survey data in order to compile policy relevant, but difficult to access, information about the Medicaid and CHIP programs into one comprehensive tool.
The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released the 2018 version of its Medicaid and CHIP Data Book. This data book is a collection of federal and state statistics regarding the Medicaid and CHIP programs that are compiled by MACPAC from multiple data sources on key topic areas including Medicaid and CHIP eligibility, enrollment, and expenditures, as well as beneficiary health, service use, and access to care. An excellent resource, the data book draws on a wide variety of data sources including Medicaid administrative data (e.g., CMS-64 data, MSIS data, Medicaid Managed Care enrollment reports, etc.) as well as federal survey data in order to compile policy relevant, but difficult to access, information about the Medicaid and CHIP programs into one comprehensive tool.
SHADAC is excited to be among the contractors that contributed to this product, providing MACPAC with estimates from the National Health Insurance Survey (NHIS) and the Medical Expenditure Panel Survey (MEPS) that highlight individual enrollment, primary source of insurance coverage, and service use and access to care with breakdowns available by age, demographics, and health characteristics. SHADAC produced these estimates using data for years 2016 and 2017, which are the latest available respectively for each survey.
For additional information on data methods and sources used in the data book, see MACPAC’s Technical Guide to MACStats, which provides supplementary information to help readers interpret the exhibits in the MACStats tables and figures as well as to understand the data sources and methods used.
Publication
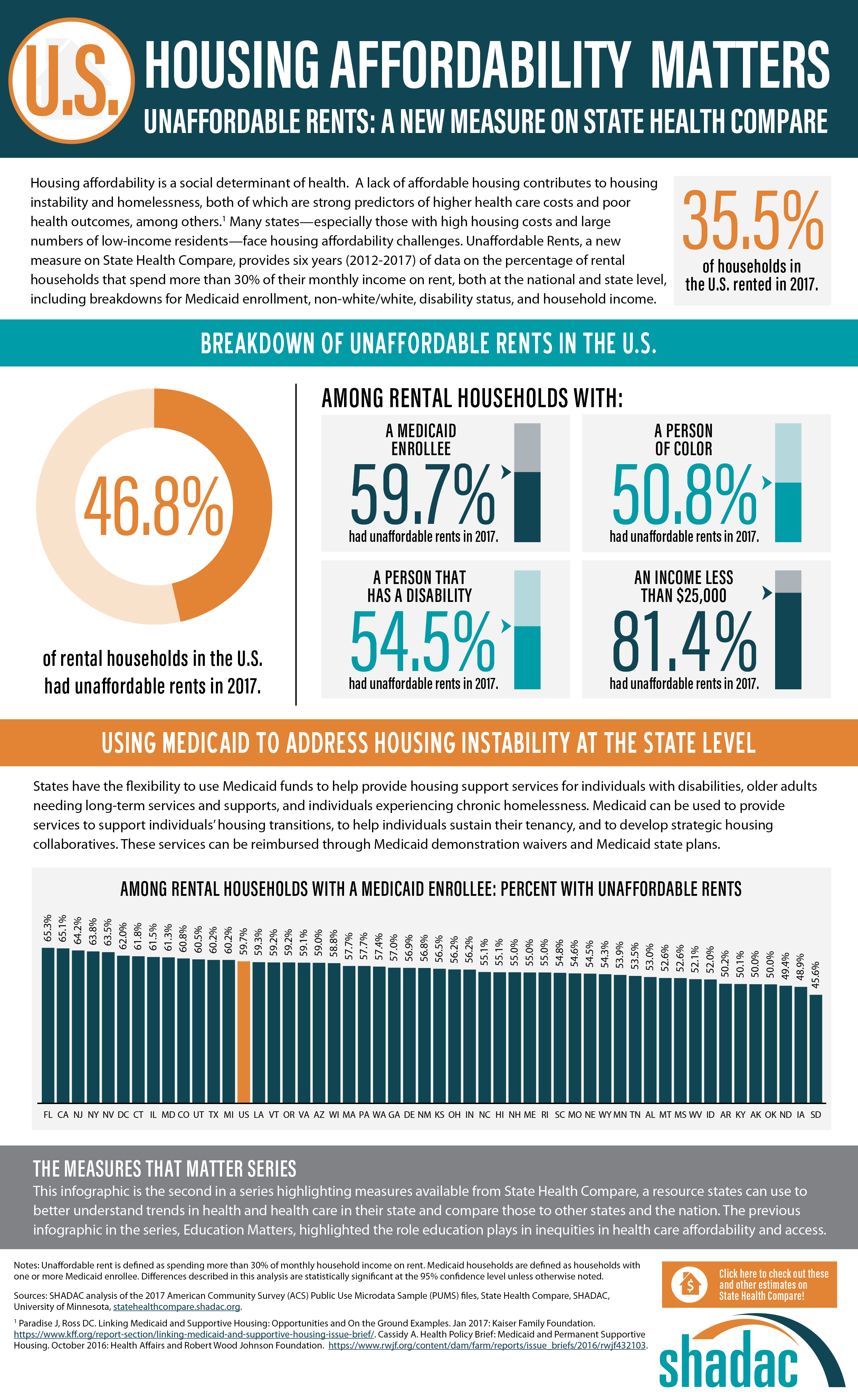
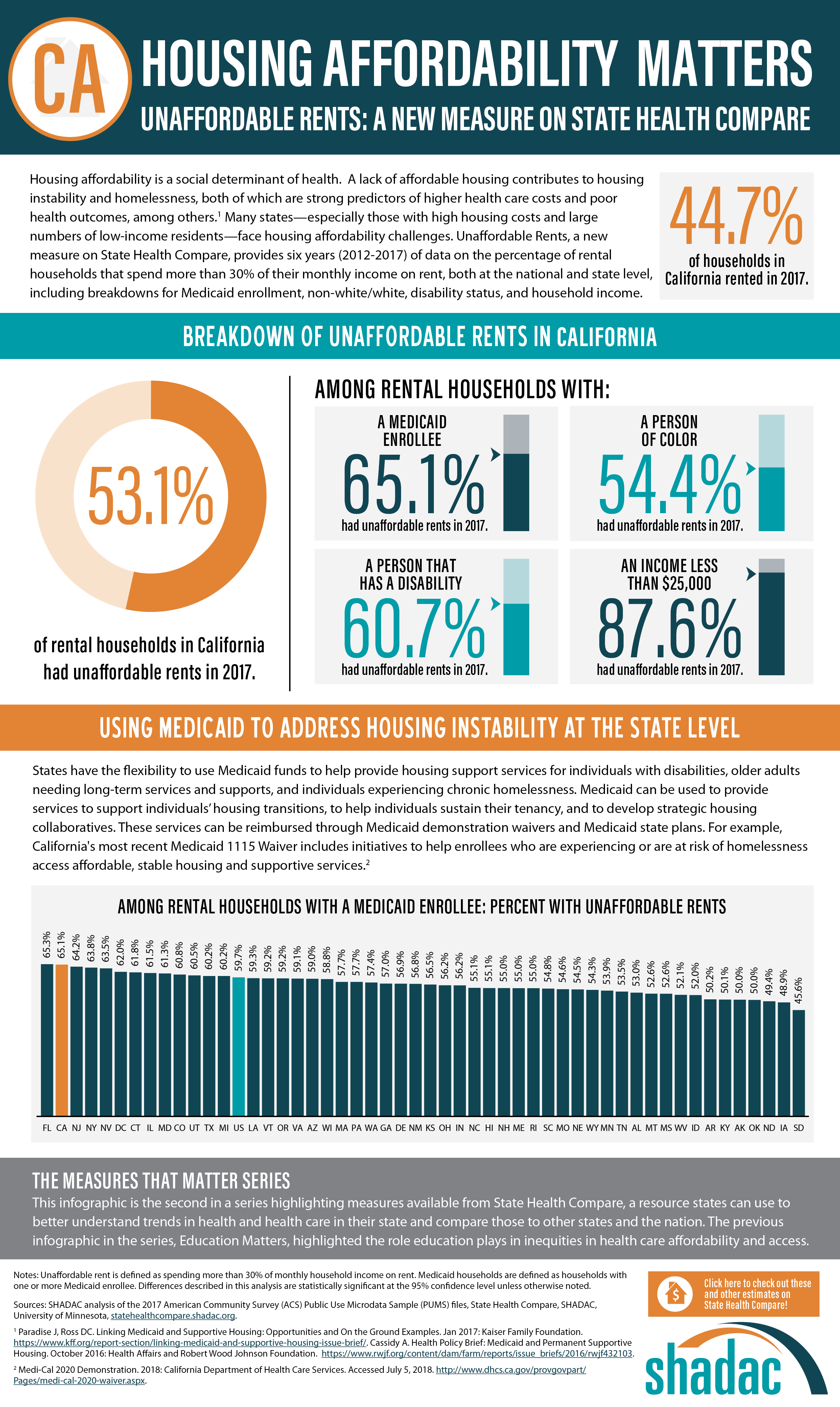
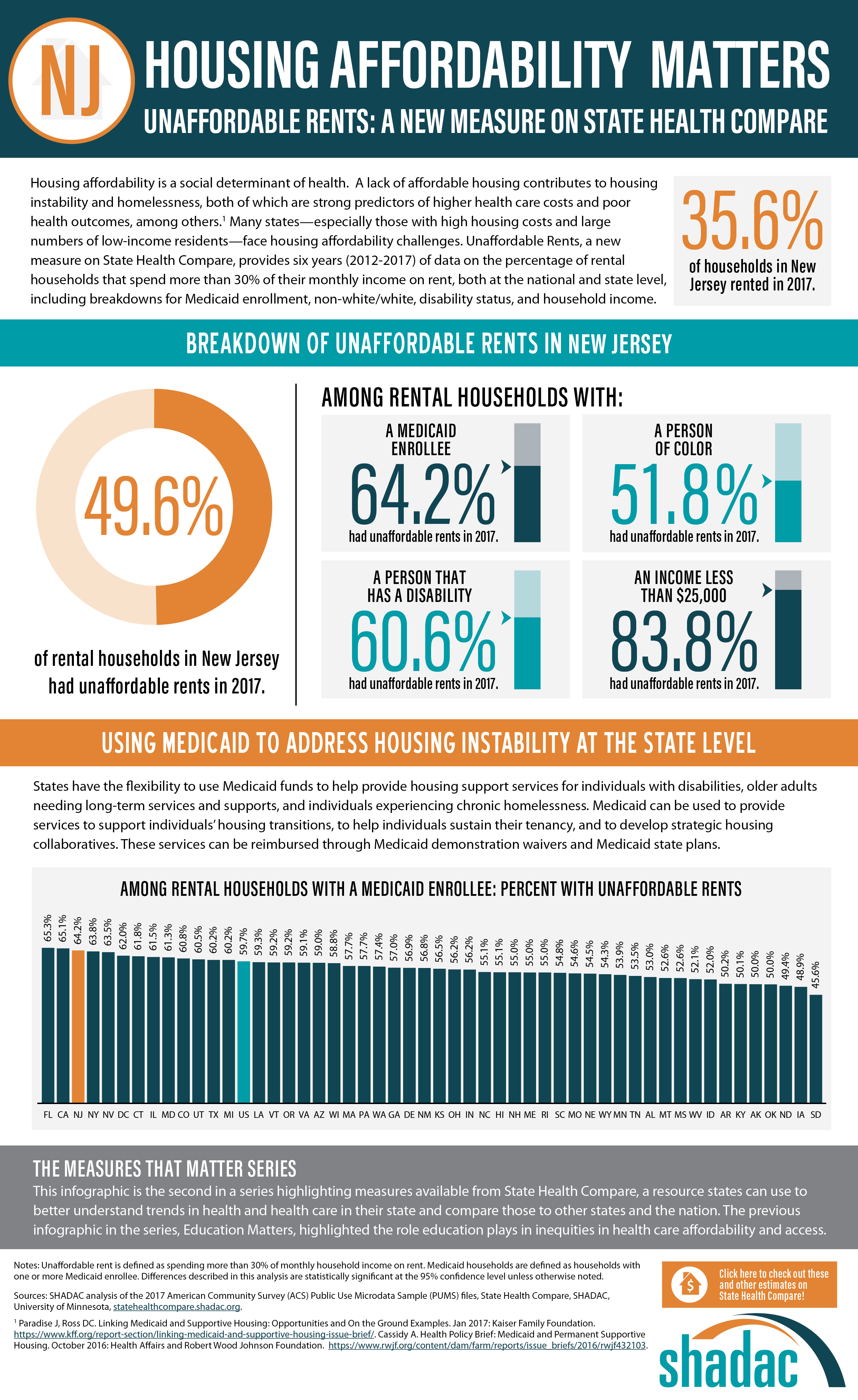
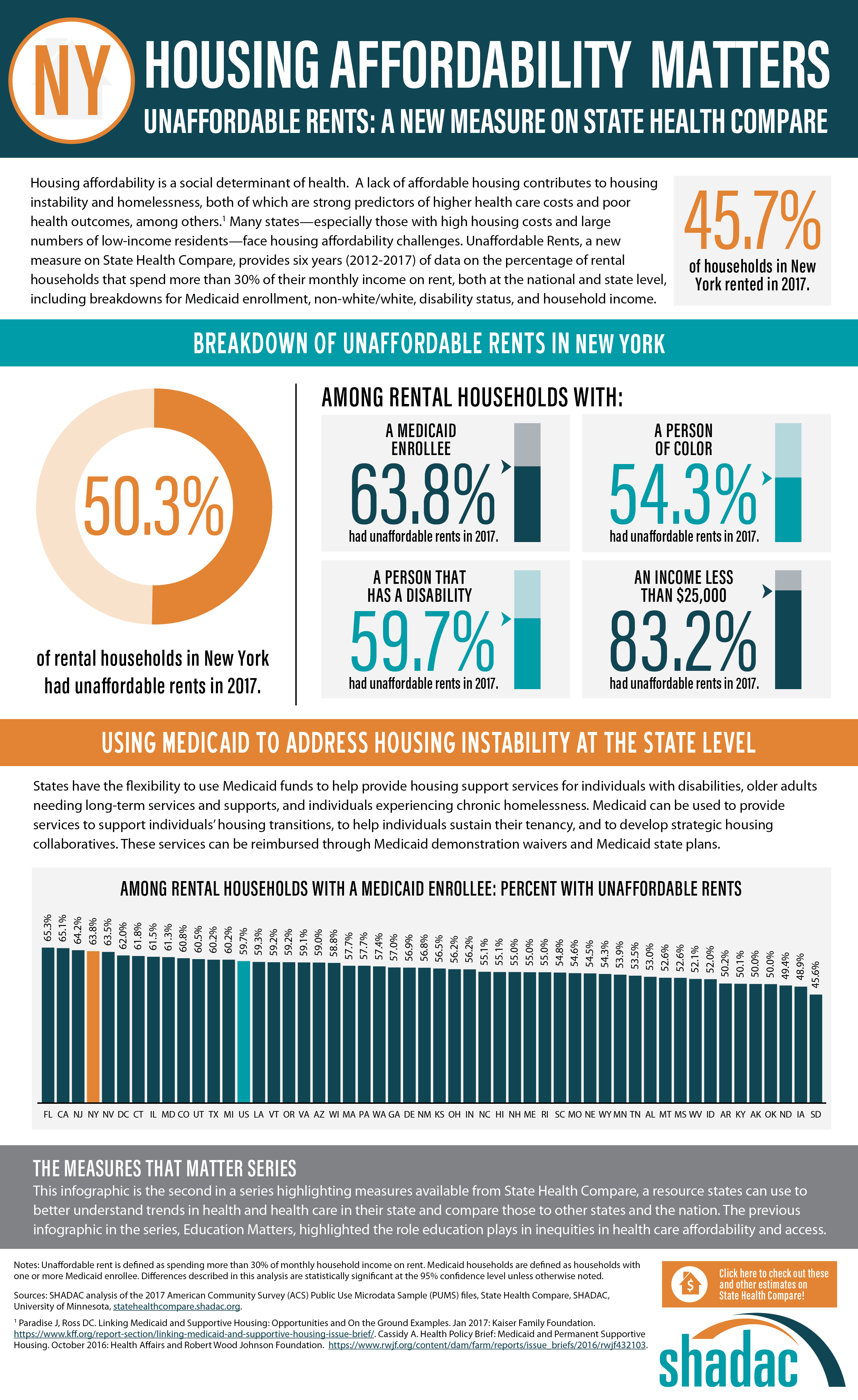
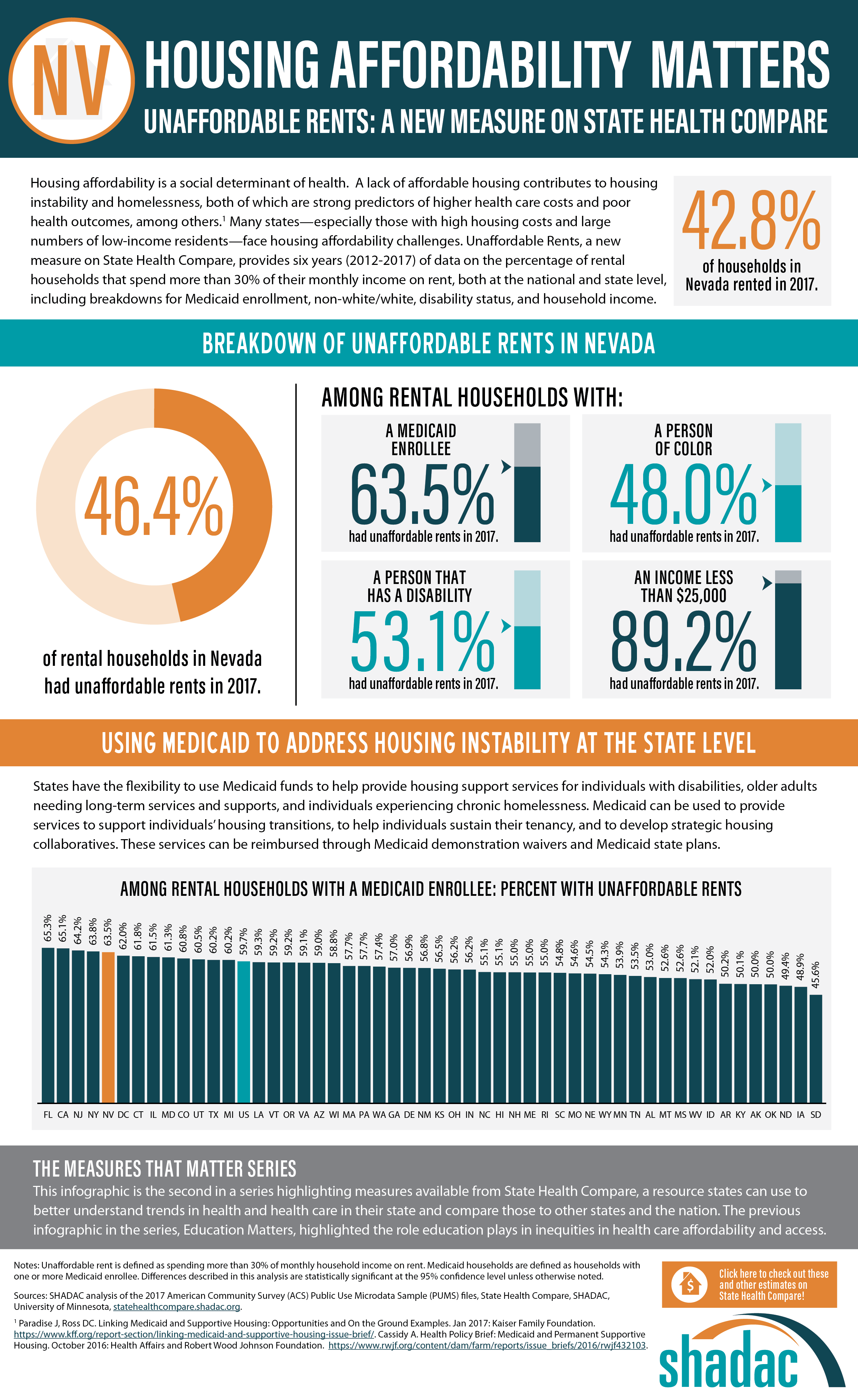
Housing Affordability Matters: Measuring and Addressing the Burden of Unaffordable Rents (Infographics)
An analysis by SHADAC examines housing affordability, looking specifically at the percent of rental households that spend more than 30% of their monthly income on rent. This measure is now available on SHADAC’s State Health Compare for all states from 2012 through 2017, and can be broken down by household income, Medicaid enrollment, race/ethnicity, and disability status.[1]
Background
SHADAC analyzed a key social determinant of health factor—housing affordability. A lack of affordable housing contributes to housing instability and homelessness, both of which are strong predictors of higher health care costs and poor health outcomes, among others.[2] Many states—especially those with high housing costs and large numbers of low-income residents—face housing affordability challenges.
Breaking Down the Issue of Unaffordable Rents
SHADAC looked at the percent of cost-burdened rental households in each state in 2017, examining unaffordable rents overall while also analyzing unaffordable rents among rental households with: a Medicaid enrollee, a person of color, a person that has a disability, and an income of less than $25,000. The infographic presented here shows these estimates for the U.S. SHADAC researchers have also created state infographics for the five states with the highest percentages of unaffordable rents among rental households that had a Medicaid enrollee—Florida (65.3%), California (65.1%), New Jersey (64.2%), New York (63.8%), and Nevada (63.5%).
Discussion: How State Medicaid Policy Can Alleviate the Burden of Unaffordable Rents
Since recent attention has been given to the idea of using Medicaid to address housing instability at the state level, the rate of unaffordable rents among rental households with Medicaid enrollees (59.7% nationally) is a particularly salient estimate, indicating that a substantial portion of this population could benefit from such efforts.
Though federal law directly prohibits federal-level matching of state Medicaid spending on housing (excepting nursing home facilities, which are already specified as a Medicaid coverage benefit), states can use Medicaid demonstration waivers and State Plan Amendments to leverage federal dollars for a wide range of housing-related services and activities, including support services for individuals with disabilities, older adults needing long-term services and supports, and individuals experiencing chronic homelessness. Medicaid can also be used to provide services to support individuals’ housing transitions, to help individuals sustain their tenancy, and to develop strategic housing collaboratives. In addition, several states, in an effort to integrate their separate yet related Medicaid and housing programs, have begun to reorganize part or all of their Medicaid delivery systems into accountable care organizations (ACOS) for more ease in using Medicaid dollars for non-medical “flexible services,” which include housing supports.[3]
Visit SHADAC and State Health Compare for More
The infographics presented here are part of SHADAC’s “Measures That Matter” product series. This series highlights measures available from State Health Compare, a web tool that states can use to explore measures related to health and health care within and across states and the nation.
The previous infographics in the series, “Education Matters,” highlighted the role education plays in inequities in health care affordability and access. Learn more about this analysis here.
Learn more about the estimates used in this analysis, as well as other measures related to social determinants of health, at State Health Compare.
[1] SHADAC. Analysis of the 2017 American Community Survey (ACS) Public Use Microdata Sample (PUMS) files. State Health Compare. statehealthcompare.shadac.org.
[2] Cassidy A. (2016). Health Policy Brief: Medicaid and Permanent Supportive Housing. Health Affairs and Robert Wood Johnson Foundation. https://www.rwjf.org/content/dam/farm/reports/issue_briefs/2016/rwjf432103.
[3] Paradise J, Ross DC. (2017). Linking Medicaid and Supportive Housing: Opportunities and On the Ground Examples. Kaiser Family Foundation. http://files.kff.org/attachment/Issue-Brief-Linking-Medicaid-and-Supportive-Housing-Opportunities-and-On-the-Ground-Examples.