Blog & News
New State Health Compare Measure: Medicaid Expenses as a Percent of State Budgets
March 24, 2021: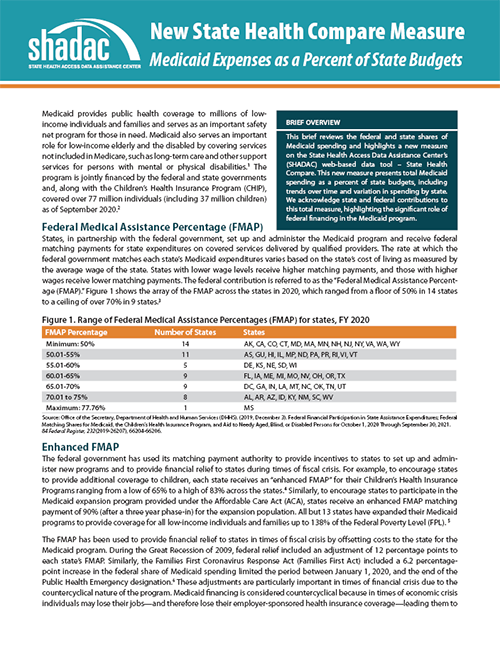 Medicaid provides public health coverage to millions of low-income individuals and families and serves as an important safety net program for those in need. Medicaid also serves an important role for low-income elderly and the disabled by covering services not included in Medicare, such as long-term care and other support services for persons with mental or physical disabilities.i The program is jointly financed by the federal and state governments along with the Children’s Health Insurance Program (CHIP).ii
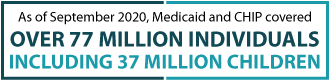
Medicaid provides public health coverage to millions of low-income individuals and families and serves as an important safety net program for those in need. Medicaid also serves an important role for low-income elderly and the disabled by covering services not included in Medicare, such as long-term care and other support services for persons with mental or physical disabilities.i The program is jointly financed by the federal and state governments along with the Children’s Health Insurance Program (CHIP).ii
This brief reviews the federal and state shares of Medicaid spending and highlights a new measure on State Health Access Data Assistance Center’s (SHADAC) web-based data tool – State Health Compare. Our measure presents total Medicaid spending as a percent of state budgets, including trends over time and variation in spending by state. We acknowledge both state and federal contributions to this total measure, highlighting the significant role of federal financing in the Medicaid program.
Click the image to read more about this new State Health Compare measure - Medicaid expenses as a percent of state budgets.
i Medicaid and CHIP Payment and Access Commission (MACPAC). (2011, March). Overview of Medicaid. https://www.macpac.gov/publication/ch-2-overview-of-medicaid/
ii Medicaid.gov. (n.d.). September 2020 Medicaid & CHIP Enrollment Data Highlights. https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html
Blog & News
Addressing Persistent Medicaid Enrollment and Renewal Challenges as Rolls Increase
September 2, 2020:Growth in Medicaid enrollment is expected to accelerate as a result of both the COVID-19 pandemic and the associated economic downturn. An analysis by the Kaiser Family Foundation (KFF), for example, shows that by January 2021, nearly 17 million people could be newly eligible for Medicaid.i In June, the Georgetown Center for Children and Families reported that Medicaid enrollment in 15 states had increased 5.8 percent over the past three months.ii The additional expected increase could mirror the surge seen during the first Patient Protection and Affordable Care Act (ACA) Open Enrollment Period (OEP1) in 2013, during which there was an influx of first-time applicants who were unfamiliar with Medicaid enrollment and renewal processes.
Although significant progress has been made in streamlining and simplifying these processes and systems for beneficiaries whose income eligibility is determined based on modified adjusted gross income (MAGI), states vary widely in their priorities and approaches.iii There are still many points along the enrollment and renewal paths where eligible individuals might remain uninsured or lose Medicaid coverage, and these challenges may be exacerbated by a surge in newly eligible individuals. Recently, some states have taken advantage of the flexibility in enrollment and eligibility determination offered by the COVID-19 Public Health Emergency (PHE) declared by Health and Human Services Secretary Alex Azar in order to streamline Medicaid enrollment processingiv v vi vii viii ix; however, this flexibility may be rolled back at the end of the PHE while widespread enrollment and renewal challenges will continue to persist.
Drawing on work done for the Medicaid and CHIP Payment and Access Commission (MACPAC), this blog provides a summary of documented, effective mitigation strategies states can use to address enrollment and renewal challenges in Medicaid and highlights strategies currently being used in four states: California, Idaho, Rhode Island, and Washington. Although this analysis pre-dates the coronavirus outbreak, these findings may offer helpful ideas about how states can address long-standing challenges in enrolling and renewing individuals in Medicaid as during current nationwide enrollment increases nationwide due to COVID-19 as well as in anticipation of returning to regular operations once the PHE expires. The findings, statements, and views expressed here are those of the authors and do not necessarily represent those of MACPAC.
Overview: Challenges and Mitigation Strategies
Trends in state Medicaid and CHIP eligibility, enrollment, and renewal policies over the past four years indicate that an increasing number of states are complying with ACA provisions designed to streamline program administration at enrollment and renewal.x States are also moving toward providing more application supports, which can make the process faster and more user-friendly, as shown in Table 1.
| Table 1. Application Supports Aimed at Streamlining Enrollment | ||||
| Indicator from Kaiser/Georgetown Survey | # of States as of | |||
| January 2017 | January 2018 | January 2019 | January 2020 | |
| Online application submission using mobile device | 28 | 31 | 38 | 44 |
| Online application has mobile-friendly design | 7 | 9 | 18 | 20 |
| Online beneficiary account supports uploading of verification documentation | 29 | 31 | 32 | 33 |
| Online secure portal for application assister | 26 | 27 | 27 | 30 |
Through document review and key informant interviews, we identified 30 ongoing Medicaid enrollment and renewal challenges, many of which are longstanding issues that predate state streamlining efforts and the COVID-19 outbreak. Exhibit 1 shows the different challenges states and beneficiaries may face at each point of the Medicaid application, income verification, and renewal processes, as well as the points between enrollment and renewal.
Exhibit 1. Remaining MAGI Medicaid Enrollment and Renewal Challenges

Source: State Health Access Data Assistance Center (SHADAC) document review and select key informant discussions 2020.
We also reviewed the robust body of literature on effective strategies for increasing MAGI Medicaid enrollment, and we compiled and organized some of the most effective strategies that states can implement at each point of the Medicaid enrollment and renewal processes (Exhibit 2).
| Exhibit 2. Summary of Effective Strategies for Mitigating Enrollment and Renewal Risks |
| Stage: Application |
|
| Stage: Verification and processing, including changes between enrollment and renewal |
|
| Stage: Renewal |
|
During our analysis we identified two persistent risk points that are especially relevant during the COVID-19 pandemic: verifying self-employment income and making eligibility determinations for complicated cases. Below we highlight effective mitigation strategies that California, Idaho, Rhode Island, and Washington have implemented to address these challenges.
Challenge: Verifying Self-Employment Income.
Income verification remains one of the biggest challenges states face when determining an individual’s financial eligibility for Medicaid.xi This is especially true for those with unstable incomes, such as individuals who are self-employed, seasonally employed, or frequently change jobs. In these cases, income may not be able to be confirmed with electronic income data sources due to data lags or other limitations. When electronic sources cannot be used, alternative documentation is required (e.g., pay stubs). Further, individuals reporting self-employment income often have to submit additional financial information, compared to those who are not self-employed, in order to verify their income. This information may include recent tax filings or profit and loss statements (i.e., summaries of revenues, costs, and expenses that were incurred during a specific period). Collecting and reporting this information can be confusing and difficult, especially for new Medicaid enrollees.
Mitigation Strategy: Offer multiple options for reporting and verifying self-employment income.
- Allow multiple forms of documentation (e.g., bank statements or self-created profit and loss statements, or self-attestation) to report self-employment income. California and Idaho both allow self-employed individuals to verify income by submitting their own self-generated profit and loss statement or a summary of their expected income generated by a certified public accountant. Both states have also created alternative forms that mirror the income and expense categories typical for self-employed individuals and can be used to help self-employed applicants or beneficiaries report their net income.
- Provide flexible tools that help self-employed individuals accurately calculate their income. Washington’s online Medicaid application includes a built-in income calculator, which assists individuals with accurately reporting their income in a variety of increments (e.g., hourly, monthly, quarterly, or annually) and then prompts individuals with additional questions in order to determine financial eligibility.
Mitigation Strategy: Clearly explain what individuals need to report and how to report it.
- Provide explicit direction about what counts as income for MAGI purposes. California has worked collaboratively with community stakeholders to create a “What Income Counts” documentxii that explains what income to report and how to report it. Similarly, Washington has a dedicated webpagexiii with guidance for self-employed individuals to calculate income and provides helpful examples of business expenses to deduct from this calculation.
- Provide education and referrals to help applicants collect needed documentation. Respondents indicated that in-person assistance from navigators and enrollment assistors remains a critical tool for individuals to successfully report their income upon initial application and at times of renewal. For example, in Idaho, navigators report success in scheduling pre-appointments with applicants to review what documents are needed for the application. Similarly, navigators in Washington indicate that tax accountants (e.g., United Way free tax preparers) have become an important referral for individuals who need help calculating profit and loss statements.
Challenge: Making Swift and Accurate Eligibility Determinations for Complex Cases.
Robust business rules engines (software systems that automate Medicaid rules as well as electronic access to data sources to verify various factors of eligibility) have been critical tools to support successful and real-time Medicaid eligibility determinations. This is especially true for simple cases, such as a single adult with relatively stable employment. Some states, however, continue to struggle with business rules engines making correct determinations in more complex enrollment situations, such as families with mixed health insurance coverage or individuals missing information on key eligibility factors.
Mitigation Strategy: Deploy a specifically trained workforce and formalize escalation procedures to resolve issues in the eligibility system.
- Create a category of navigators authorized to move more complex cases through the application or renewal process. Washington provides additional training to “enhanced” navigators who offer technical assistance to regular navigators in order to troubleshoot problems that arise when processing complex cases. Enhanced navigators attend additional training throughout the year to receive updates on processes and policies, and they have a higher level of access to the eligibility system.
- Provide a mechanism to escalate cases. Rhode Island provides navigators with the ability to escalate cases that appear to have received incorrect eligibility determinations, especially in situations where there is a quick-turnaround time needed—e.g., medical emergencies. Escalation teams within the state’s human services agency are designated to respond to navigators in a timely manner with a determination review.
Mitigation Strategy: Utilize community feedback mechanisms to identify enrollment challenges with complex cases and identify mitigation solutions.
- Interviewees in all four states (California, Idaho, Washington, and Rhode Island) highlighted the importance of community feedback mechanisms in providing a venue for navigators to bring developing challenges and areas of concern to the attention of the state and to suggest solutions. Specifically, stakeholders in California and Washington spoke positively about the increasing number of opportunities—such as formal consumer-focused stakeholder workgroup meetings or informal communication channels—for navigators, eligibility workers, and community organizations to collaborate regularly with state agency staff to discuss complex cases and consider ways to better address these situations.
Conclusion
Our analysis focused on identifying effective and innovative strategies for addressing Medicaid enrollment and renewal challenges and exploring specific strategies used by four states—California, Idaho, Washington, and Rhode Island. Since this study, the spread of the COVID-19 virus has simultaneously increased the need for medical coverage to cover fees associated with COVID treatment and triggered an economic downturn, and both of these issues are expected to increase enrollment in Medicaid programs nationwide.xiv While the administrative flexibilities mentioned earlier aim to facilitate the influx of new Medicaid enrollments for the time being, the main risk points of Medicaid enrollment and renewal can be expected to continue in some form and will no doubt return when the Public Health Emergency ends.xv The need to continue to explore and implement innovative enrollment and renewal approaches remains, and the findings from this analysis can offer a reminder to states of ongoing efforts to improve Medicaid enrollment and renewal processes.
Publication
2018 State-level Estimates of Medical Out-of-Pocket Spending for Individuals with Employer-sponsored Insurance Coverage
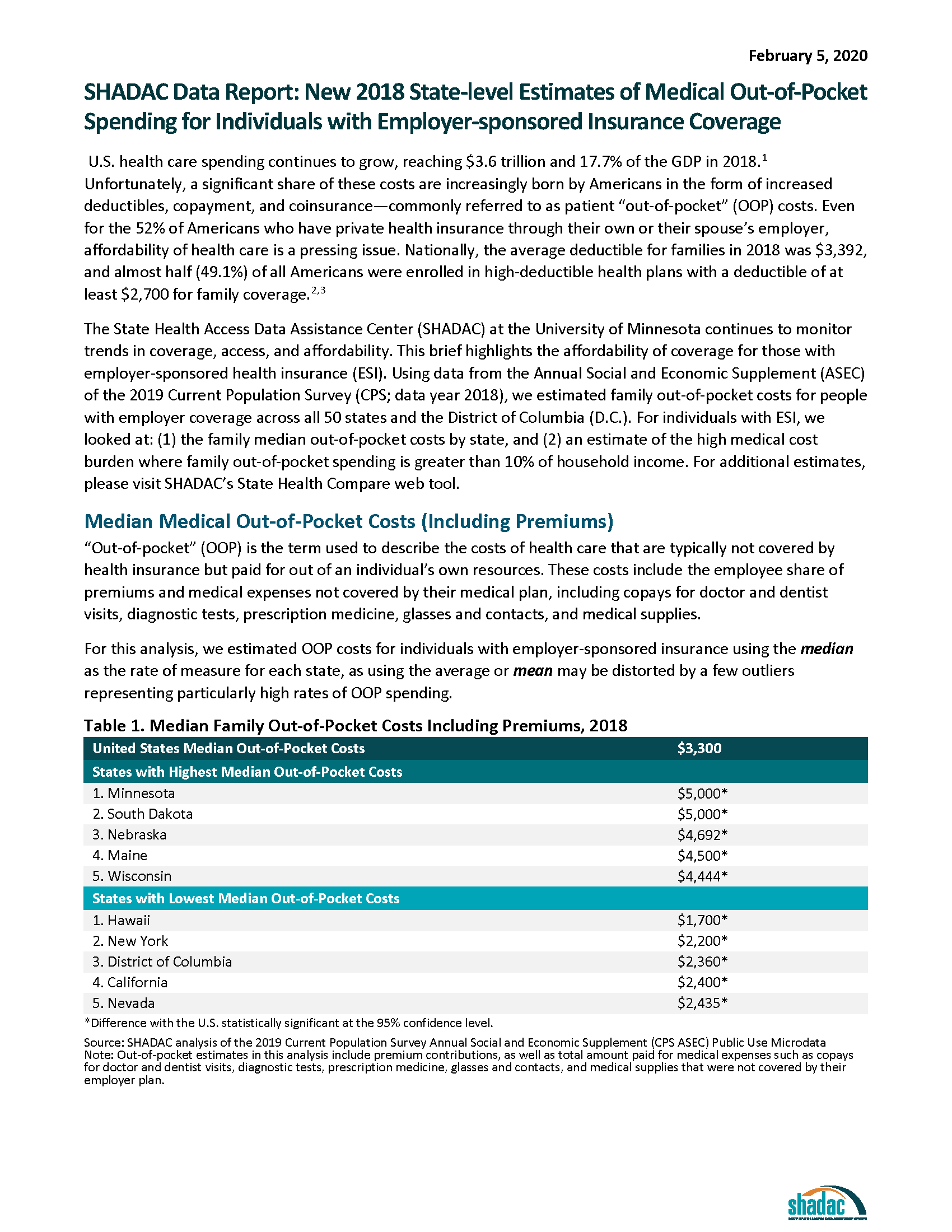 U.S. health care spending continues to grow, reaching $3.6 trillion and 17.7% of the GDP in 2018.[i] Unfortunately, a significant share of these costs are increasingly born by Americans in the form of increased deductibles, copayment, and coinsurance—commonly referred to as patient “out-of-pocket” (OOP) costs. Even for the 52% of Americans who have private health insurance through their own or their spouse’s employer, affordability of health care is a pressing issue. Nationally, the average deductible for families in 2018 was $3,392, and almost half (49.1%) of all Americans were enrolled in high-deductible health plans with a deductible of at least $2,700 for family coverage.[ii],[iii]
U.S. health care spending continues to grow, reaching $3.6 trillion and 17.7% of the GDP in 2018.[i] Unfortunately, a significant share of these costs are increasingly born by Americans in the form of increased deductibles, copayment, and coinsurance—commonly referred to as patient “out-of-pocket” (OOP) costs. Even for the 52% of Americans who have private health insurance through their own or their spouse’s employer, affordability of health care is a pressing issue. Nationally, the average deductible for families in 2018 was $3,392, and almost half (49.1%) of all Americans were enrolled in high-deductible health plans with a deductible of at least $2,700 for family coverage.[ii],[iii]
The State Health Access Data Assistance Center (SHADAC) at the University of Minnesota continues to monitor trends in coverage, access, and affordability. This brief highlights the affordability of coverage for those with employer-sponsored health insurance (ESI). Using data from the Annual Social and Economic Supplement (ASEC) of the 2019 Current Population Survey (CPS; data year 2018), we estimated family out-of-pocket costs for people with employer coverage across all 50 states and the District of Columbia (D.C.). For individuals with ESI, we looked at: (1) the family median out-of-pocket costs by state, and (2) an estimate of the high medical cost burden where family out-of-pocket spending is greater than 10% of household income. For additional estimates, please visit SHADAC’s State Health Compare web tool.
[i] Centers for Medicare & Medicaid Services (CMS). (2019, December 5). NHE Fact Sheet. Retrieved from https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet/
[ii] State Health Access Data Assistance Center analysis of the 2018 American Community Survey microdata.
[iii] State Health Access Data Assistance Center, State-level Trends in Employer-Sponsored Health Insurance, 2014-2018. Available at: https://www.shadac.org/ESIReport2019
SHADAC Expertise
Medicaid and CHIP Policy
SHADAC has worked both independently and under contract to the Robert Wood Johnson Foundation (RWJF) and the Medicaid and CHIP Payment Access Commission (MACPAC) to monitor and analyze changes in the Medicaid and CHIP policy landscape such as Medicaid expansion, eligibility, enrollment, and renewal, quality measurement, as well as states’ waiver application, implementation, and evaluation. SHADAC faculty and staff have exceptional knowledge of Medicaid and CHIP, including knowledge from the perspective of state policymakers and program administrators, as well as operational issues at the federal and state levels.
Related SHADAC work
Click on any title below to learn more about the project.
Tracking the Data on Medicaid’s Continuous Coverage Unwinding (State Health & Value Strategies)
A lack of publicly available data on Medicaid enrollment, renewal, and disenrollment makes it difficult to understand exactly who is losing Medicaid coverage and for what reasons. This issue brief lays out a phased set of priority measures and provides a model enrollment and retention dashboard template that states can use to monitor both the short-term impacts of phasing out public health emergency (PHE) protections and continuous coverage requirements, as well as longer-term enrollment and retention trends. Through its work with SHVS, SHADAC also published a series of issue briefs that tracked through an interactive map the format of state reporting of unwinding data, state-based marketplace transition data (i.e. people who no longer qualify for Medicaid but might be eligible for a qualified health plan offered through the marketplace), and Medicaid unwinding reinstatement data.
Supporting BDT’s Stabilizing Medicaid Enrollment Learning Collaborative
SHADAC collaborated with a new partner, Benefits Data Trust (BDT), on a small project to design and lead a webinar for its Medicaid Churn Learning Collaborative participants on the topic of monitoring and evaluation. The webinar took place as state Medicaid agency participants were implementing activities to redetermine all individuals enrolled in Medicaid and were meeting federal reporting requirements to monitor the end of the continuous coverage provisions.
Tracking Health Insurance Coverage During the Unwinding: Monthly Data from the Household Pulse Survey
The unwinding of the Medicaid continuous coverage requirement ("Medicaid Unwinding") represents the largest nationwide coverage transition since the Affordable Care Act. Since February 2020, enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) has increased by 23 million enrollees. Not only that, but analysis also indicates that as many as 15 million individuals will exit Medicaid to other coverage or become uninsured. Lack of publicly available data on Medicaid enrollment, renewal, and disenrollment makes it difficult to track the phenomenon of the 'Medicaid Unwinding'. As states “unwind” the Medicaid continuous coverage requirement and restart standard redetermination procedures, SHADAC researchers are using data from the U.S. Census Bureau’s Household Pulse Survey (HPS) to track trends in health insurance coverage rates. See our findings and frequent updates here.
Past Work
Assessment and Synthesis of Selected Medicaid Eligibility, Enrollment, and Renewal Processes and Systems in Six States
SHADAC worked as a contractor for the Medicaid and CHIP Payment Access Commission (MACPAC) to conduct an assessment of Medicaid eligibility, enrollment, and renewal processes and systems in six study states—Arizona, Colorado, Florida, Idaho, New York, and North Carolina. Utilizing a multi-case study methodology as well as key informant interviews with state and local agency staff and advocacy organizations, SHADAC collected and synthesized data on Medicaid enrollment processes and systems for individuals whose income eligibility is based on Modified Adjusted Gross Income (MAGI) in order to assess the extent to which states were achieving desired goals such as program efficiency and a simplified beneficiary experience. As a follow up, SHADAC identified the risks that remain for both individuals and state agencies that cause eligible individuals to remain uninsured or lose Medicaid coverage and conducted interviews with key stakeholders nationally and in four states to obtain additional input on potential risk points and strategies to improve eligibility determination and renewal accuracy.
SHADAC Advocates a Data-based Approach to Advancing Medicaid and CHIP Access Monitoring Plan
On February 17, 2022, the Centers for Medicare & Medicaid Services (CMS) released a request for information (RFI) regarding access to coverage and care in Medicaid and the Children’s Health Insurance Program (CHIP). SHADAC researchers focused our response on Objective 4: Question 1, which asked researchers to consider how CMS might develop a stronger Medicaid and CHIP access monitoring approach through data reporting and analysis. These comments are based on SHADAC’s experience providing data and evaluation technical assistance (TA) to states, and mirror recent testimony to the Medicaid and CHIP Payment Access Commission (MACPAC) provided by SHADAC’s Deputy Director.
Addressing Social Determinants of Health through Behavioral Health-focused 1115 Waivers: Implementation Lessons from Three States
Through the Robert Wood Johnson Foundation’s (RWJF) “Research in Transforming Health” program, SHADAC researchers conducted a study to understand how three states—Illinois, Texas, and Washington—were addressing the needs of justice-involved populations through implementation of Section 1115 Medicaid waiver programs. The specific aim of the study was to identify promising practices and lessons learned related to the development, implementation, and management of these innovative behavioral health policies with the purpose of informing policy development in states considering similar 1115 waivers.
Blog & News
Evaluations of Integrated Care Models for Dually Eligible Beneficiaries: Key Findings and Research Gaps from MACPAC
August 08, 2019:Under contract to the Medicaid and CHIP Payment and Access Commission (MACPAC), researchers at SHADAC recently compiled an inventory of evaluations of integrated care models for beneficiaries enrolled in both Medicare and Medicaid, for which both the inventory itself and a related issue brief have now been published.
About the Study
Currently, both the federal government and numerous states are testing a variety of models to integrate care for beneficiaries enrolled in both Medicare and Medicaid, including the Program of All-Inclusive Care for the Elderly, the Financial Alignment Initiative (FAI), Medicare Advantage dual eligible special needs plans and fully integrated dual eligible special needs plans, managed long-term services and supports programs, and demonstrations that pre-dated the FAI.
There is a limited but growing body of evidence examining the effects of these models on Medicare and Medicaid spending, health outcomes, and access to care. Broadly, studies to date have generally found a decrease in hospitalizations and readmissions for enrollees in the different models relative to those not enrolled in integrated models. Findings regarding the use of other services, such as use of the emergency department and long-term services and supports, were mixed—as are reports on beneficiary experience. It is often difficult to generalize from evaluations of specific models about the effects of integrated care more broadly.
This new inventory details a total of 51 studies, including those published between 2004 to November 2018 and formal evaluations on the FAI updated through July 2019, and gathers all available evidence on how programs have affected spending, quality, health outcomes, and access.
Access the Inventory of Evaluations of Integrated Care Programs for Dually Eligible Beneficiaries to read and download the full literature review and inventory compiled by SHADAC.
For a high-level summary on data methods and sources used for the review and inventory, see the companion brief, Evaluations of Integrated Care Models for Dually Eligible Beneficiaries: Key Findings and Research Gaps.











