Publication
UPDATE State Health Insurance Program Names: 2023
 This Excel file includes the names of state-sponsored health insurance programs for all 50 states and the District of Columbia. It documents program names familiar to enrollees; therefore it includes colloquial as well as official names. The document has two tabs – the first includes names of traditional state-sponsored insurance programs such as Medicaid and CHIP. The second tab includes information on insurance marketplaces.
This Excel file includes the names of state-sponsored health insurance programs for all 50 states and the District of Columbia. It documents program names familiar to enrollees; therefore it includes colloquial as well as official names. The document has two tabs – the first includes names of traditional state-sponsored insurance programs such as Medicaid and CHIP. The second tab includes information on insurance marketplaces.
The purpose of the document is to act as a resource for researchers interested in state health care programs. This list was compiled by the State Health Access Data Assistance Center (SHADAC).On an annual basis, SHADAC contacts state Medicaid staff to verify the names of public health insurance programs within each state. SHADAC compiles and delivers these program names to the U.S. Census Bureau for use in federal surveys that measure health insurance coverage, such as the Current Population Survey (CPS).
Information on program names was collected between September and October of 2021 and includes all comprehensive state-sponsored health insurance programs that were in operation during 2021. Therefore, it includes programs that were scheduled to cease operations. Information on marketplace type was confirmed using HealthCare.gov and the Kaiser Family Foundation's 2022 table found here.
We welcome any suggestions for modifications or corrections. Please share them through our email address at shadac@umn.edu.
Blog & News
A New Brief Examines the Collection of Sexual Orientation and Gender Identity (SOGI) Data at the Federal Level and in Medicaid
October 2021:Thirteen million people identify as part of a sexual or gender minority (SGM) in the United States, with an estimated 1.17 million who have Medicaid as their primary source of health insurance coverage.[1],[2] While the COVID crisis shed a unique light on the need for more equitable health data collection across all populations, one area in which efforts are still falling short is sexual orientation and gender identity (SOGI) data – especially for those covered by Medicaid. However, change is happening, and states are leading the way.
A new State Health and Value Strategies brief, authored by SHADAC researchers, documents a few examples of SOGI data collection efforts occurring at the federal level and in Medicaid, and highlights the efforts of an Oregon community stakeholder process that identified several key areas for SOGI data improvement.
 SOGI Data at the Federal Level
SOGI Data at the Federal Level
Unfortunately, there is no current federal data standard for sexual orientation and gender identity. The data standard from the Department of Health and Human Services (HHS), released in 2011, defines the category of “sex” only as biological sex and makes no mention of gender or gender identity. Additionally, when SOGI data collection efforts have been made over the past decade, certain aspects have been more routinely measured than others. For instance, most of the research to-date has focused on how to collect sexual orientation, and very little continues to be known about the best way to collect gender identity. A review in 2016, for example, found that of the 12 federal surveys that collect various aspects of SOGI information, only half of those collect information on gender identity.
SOGI Data in Medicaid
The collection of SOGI data in Medicaid is even less common than in federal surveys. SHADAC’s review of state Medicaid applications identified only two states that provided applicants an opportunity to select something other than “male” or “female” when asked to indicate their sex/gender (these terms were used interchangeably to refer to biological sex). Connecticut’s paper application has an open-text write-in option for “gender.” Oregon asks applicants to indicate their “sex assigned at birth” as well as their “gender identity.”
Improving the Collection of SOGI Data – The Oregon Model
There are still many unresolved methodological and conceptual issues when it comes to the collection of SOGI information, and very limited research assessing the validity of SOGI data specifically collected via the Medicaid application process. But one state leading the way in this effort is Oregon.
In 2018, the Oregon Health Authority (OHA) Office of Equity and Inclusion convened a SOGI Data Collection Workgroup, composed of stakeholders who interact with the Lesbian, Gay, Bisexual, Transgender, Queer, and other (LGBTQ+) community and health systems, many of whom also identify as LGBTQ+ themselves, to develop a set of SOGI data standards. The group recommended a key set of five demographic questions and response options, some open-ended for the respondent to be able to write an answer and some with the ability to check more than one categorical box, if appropriate. Options were also given for the respondent to say that they either did not want to answer or did not know what the question was asking. The workgroup also identified that a set of additional questions were needed in order to ensure respectful communication.
Soon these standards will be put into practice. A bill requiring OHA and the Oregon Department of Human Services to expand their existing race, ethnicity, language and disability data collection standards to include SOGI was recently passed by the state legislature. The state plans to convene a rule-making advisory committee in the winter of 2022 to finalize SOGI standards using the work group’s draft standards as a starting point.
Looking Forward
There continues to be very limited research assessing the validity of SOGI data specifically collected via the Medicaid application process. Absent any type of federal standard, states looking to explore different options to address their SOGI data collection gaps may need to modify SOGI questions depending on a variety of factors including the age, cultural background, and language preferences of their target population; as well as be mindful of the evolving terminology used to identify gender identity. Oregon serves as an excellent model for how to undertake a thoughtful community stakeholder process that can inform efforts to establish new data collection on a topic that is fluid and rapidly changing, yet vitally important for the health of Medicaid populations.
[1] Conron, K.J. & Goldberg, S.K. (April 2020). LGBT people in the US not protected by state non-discrimination statutes. UCLA School of Law, The Williams Institute. https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGBT-ND-Protections-Update-Apr-2020.pdf
[2] 3. Conron, K.J. & Goldberg, S.K. (January 2018). Over half a million LGBT adults face uncertainty about health insurance coverage due to HHS guidance on Medicaid requirements. UCLA School of Law, The Williams Institute. https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGBT-Medicaid-Coverage-US-Jan-2018.pdf
Publication
Impacts of the Affordable Care Act Medicaid Expansion in California (CJPP)
This Journal article was originally published in the California Journal of Politics and Policy.
Introduction
A cornerstone aim of the Affordable Care Act (ACA) was to make health insurance coverage readily available to more people in the United States through policies such as new federal subsidies to help people with moderate incomes purchase private insurance through new Marketplaces and expanding Medicaid’s reach to many more low-income adults. Key components of the ACA were implemented in 2014, including state-level expansions of Medicaid. Studies that compared states that opted for and against expanding their Medicaid programs have documented gains in coverage, access, and health status particularly among low-income and childless adults, who were the main subpopulation beneficiaries of Medicaid expansion in states that adopted it.i However, few of these studies have focused specifically on California. To our knowledge, past studies on the effects of Medicaid expansion in California have not examined self-reported general health and physical/mental health for low-income adults. Self-reported health measures are important for monitoring population health over time, quantifying individual satisfaction with health, and complementing objective long-term outcomes such as mortality.ii
This journal article authored by SHADAC researchers Natalie Schwehr, Giovann Alarcón, and Lacey Hartman examines the impact of the Affordable Care Act (ACA) on healthcare coverage, access, health status, and affordability, as well as disparities in these outcomes by race/ethnicity among low-income Californians.
Using nationally representative survey data from the Behavioral Risk Factor Surveillance Survey 2011-2019 and a difference-in-differences approach that compared California with nonexpansion states, they examined the impact of Medicaid expansion on health insurance coverage, having a usual source of care, self-reported health status, frequent (≥14) unhealthy days in the past month (physical, mental, and both), and foregone care due to cost.
The sample population included low-income Californians (<100% of the federal poverty guidelines) aged19-64 and low-income childless adults.
Key Findings
- Low-income adults, childless adults, and white childless adults in California saw post-ACA gains in six of seven outcomes, including a 7.7 percentage point increase in having a usual source of care for all low-income adults.
- Childless adult people of color (POC) reported significant improvements in three measures, with a 6.6 percentage point increase in having a usual source of care (CI: 0.013 to 0.120).
- All groups examined had coverage gains, ranging from 3.9 percentage points for all low-income adults, to 8.4 percentage points for white childless adults.
- All groups reported improved mental health, including an 8.2 percentage point decrease in frequent mental distress for childless adults.
These findings indicate that the ACA coverage expansion benefitted the targeted population of low-income Californians. Additionally, the disparity between white and non-white Californians decreased for the unadjusted mean rate of having a usual source of care. However, unadjusted means showed that white low-income adults remained more likely to have health insurance coverage and a usual source of care compared with POC in both California and nonexpansion states.
Read the full article in the California Journal of Politics and Policy, or download it here.
Suggested Citation
Schwehr, N., Alarcón, G., & Hartman, L. (2021). Impacts of the Affordable Care Act Medicaid Expansion in California. California Journal of Politics and Policy, 13(1). http://dx.doi.org/10.5070/P2cjpp13154573 Retrieved from https://escholarship.org/uc/item/17d520j7
i Simon, Kosali, Aparna Soni, and John Cawley. 2017. “The Impact of Health Insurance on Preventive Care and Health Behaviors: Evidence from the First Two Years of the ACA Medicaid Expansions.” Journal of Policy Analysis and Management36 (2): 390–417. https://doi.org/10.1002/pam.21972
ii Dwyer-Lindgren, Laura, Johan P. Mackenbach, Frank J. van Lenthe, and Ali H. Mokdad. 2017. “Self-Reported General Health, Physical Distress, Mental Distress, and Activity Limitation by US County, 1995-2012.” Population Health Metrics15 (1): 1–12. https://doi.org/10.1186/s12963-017-0133-5.
Blog & News
Explore Physician Acceptance of New Medicaid Patients through Two New Measures on SHADAC’s State Health Compare and in a New MACPAC Factsheet
August 5, 2021:Authors: Robert Hest and Julia Ngep
In order for the more than 80 million Medicaid beneficiaries to access needed care in a timely manner, there must be a sufficient number of health care providers to serve these patients. There has long been concern that providers are less likely to accept Medicaid patients than patients with other types of health insurance coverage. Because Medicaid policies—and providers’ responses to those policies—differ substantially across states, state-level data is critical for monitoring the providers’ decisions to accept Medicaid patients and for understanding the factors that influence those decisions.
Using data from the 2011-2017 National Electronic Health Records Survey (NEHRS),1 SHADAC performed an analysis to examine and compare physician acceptance of new Medicaid patients at the state level and by physician and practice characteristics. This analysis was performed under contract with the Medicaid and CHIP Payment and Access Commission (MACPAC) and is presented in two new measures on SHADAC’s State Health Compare web tool as well as in a new MACPAC factsheet.
State Health Compare Measures
 Physicians who accept new patients
Physicians who accept new patients
Physicians who accept new patients measures the percent of physicians who accept new patients by type of coverage: private, Medicare, and Medicaid. Data years were pooled where single-year estimates were not possible and are available for 2011-2013 and 2014-2017.
In 2014-2017, state-level physician acceptance of Medicaid patients ranged from 42.2 percent in New Jersey to 99.4 percent in North Dakota, acceptance of Medicare patients ranged from 77.1 percent in Georgia to 98.3 percent in North Dakota, and acceptance of private patients ranged from 80.3 percent in the District of Columbia (D.C.) to 100.0 percent in Nebraska.
Physicians who accept new Medicaid patients
Physicians who accept new Medicaid patients measures the percent of physicians who accept new Medicaid patients by the following physician/practice characteristics:
- Setting (private solo/group versus total) available for pooled data years 2011-2012 and 2014-2017;
- The share of Medicaid existing patients (above versus below national average) available for pooled data years 2011 & 2013 and 2014-2017;
- And the ratio of mid-level providers (above versus below national average) available for pooled data years 2014-2017.
At the national level in the most recent time period: physicians in private solo/group practices were less likely to accept new Medicaid patients compared to all physicians (70.4% versus 74.0%); physicians with an above-average share of existing Medicaid patients were more likely to accept new Medicaid patients compared to all physicians (87.4% versus 63.8%); and physicians with an above-average ratio of mid-level providers were more likely to accept new Medicaid patients compared with all physicians (80.5% versus 73.7%).
New MACPAC Factsheet
 Physician Acceptance of New Medicaid Patients: Findings from the National Electronic Health Records Survey
Physician Acceptance of New Medicaid Patients: Findings from the National Electronic Health Records Survey
This new MACPAC factsheet analyzes physician acceptance of new Medicaid patients at the national and state levels. As Medicaid programs vary by each state and there is little information on physician participation in Medicaid at the state level, this analysis provides an important update of previous MACPAC work analyzing physician acceptance at the national level and prior literature analyzing state-level physician acceptance, last updated for data year 2013.
The analysis found significant differences in rates of physician acceptance of new patients by coverage type, with physicians being more likely to accept private and Medicare patients compared with Medicaid patients. Acceptance of Medicaid patients varied significantly by state and by various patient, physician, and practice characteristics. These include source of patient coverage (Medicaid, Medicare, and private), physician specialty, practice setting, existing Medicaid caseload, and presence of mid-level providers. The analysis found that nationally, rates of physician acceptance were stable over time and increased significantly in a handful of states, with no states experiencing significant decreases in rates of acceptance.
1 Data for 2016 was not released by National Center for Health Statistics (NCHS), which conducts the NEHRS. Data were unavailable by setting in data year 2013; data were unavailable by share of existing Medicaid patients for data year 2012; and data were unavailable by ratio of mid-level providers for data years 2011-2013.
Blog & News
Minnesota Medicaid Enrollment Grew More than the U.S. Average during COVID-19
July 21, 2021:The Minnesota Medicaid program has served as an important safety net program during the COVID-19 crisis. As a countercyclical program, Medicaid enrollment/spending increases when the economy is in decline (such as during a pandemic or a recession), as employer-sponsored insurance decreases and the low-income population increases.1
The additional enrollment of 166,364 individuals in Minnesota from February 2020 to January 2021 provided important and needed coverage during this unprecedented time.2 The COVID-19 public health emergency declaration has supported this growth with the moratorium on disenrollment and extended open enrollment sessions.
Medicaid in Minnesota
Minnesota was an early Medicaid expansion state through the options provided by the Affordable Care Act. Minnesota extended eligibility for Medicaid (called Medical Assistance in the state) to childless adults at or below 75% of the Federal Poverty Guideline (FPG) in 2011 and adopted the full expansion to 138% FPG in 2014.3,4 In 2019, Medical Assistance in Minnesota provided health insurance coverage to approximately 13.1% of the state’s population.5
Minnesota’s Medicaid expansion was a crucial resource during the COVID-19 pandemic for those who lost their jobs and/or their employer-sponsored health insurance coverage. It is estimated that approximately 29,500 Minnesotans lost their private health insurance coverage between April 2020-July 2020.6 Despite these changes, data from the 2019 Minnesota Health Access Survey and the state’s 2020 Health Insurance Enrollment Survey show that Minnesota’s uninsured population has stayed relatively stable during COVID-19, with increases in Medicaid enrollment making up for some of the losses experienced in the private insurance market.6
Minnesota in Context
SHADAC analyzed a recently released 50-state review of Medicaid growth during COVID-19 from Manatt Health to explore how Medicaid enrollment in Minnesota during COVID-19 compares to the rest of the United States.1 Manatt Health utilized state-specific sources to gather data from February 2020 through January 2021. These data show that Minnesota’s Medicaid program has not only stabilized the state’s coverage landscape but has also grown at a faster pace than many other state Medicaid programs. A total of 21 states have reported data from February 2020 to January 2021, and they are included in this analysis.
Key Findings1
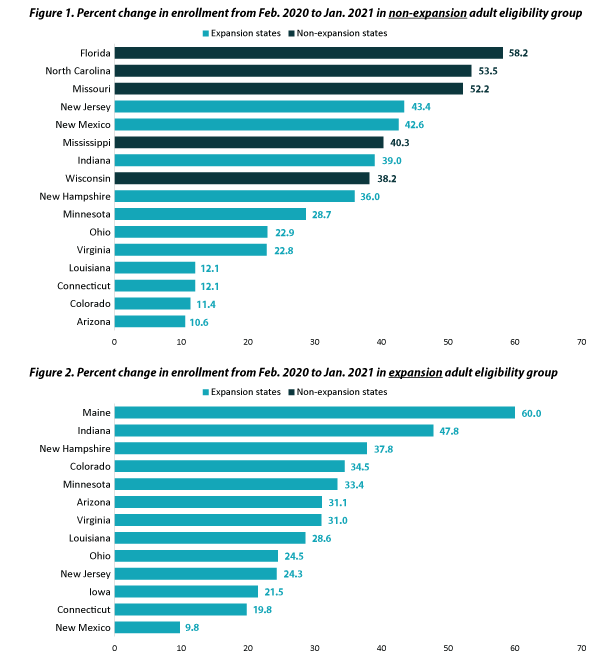
From February 2020 to January 2021, enrollment in Medical Assistance grew by 19.7 percent in Minnesota, from 844,467 to 1,010,831. This increase was higher than the national median growth rate of 14.5 percent in expansion states and 15.7 percent in non-expansion states.
Only 3 of the 21 states that provided Medicaid enrollment data for this time period experienced larger growth: Florida, Indiana, and Missouri. The highest percentage growth among states was 22.6% in Missouri, and the lowest growth was 8.2% in Tennessee.
When comparing Medicaid expansion adults with non-expansion adults, Minnesota saw a growth in enrollment of 33.4% vs 28.7%, respectively. Minnesota’s enrollment growth was above the median for reporting states for expansion adults (31.0%) but below the 37.1% median for non-expansion adults (Exhibits 1 and 2).1
Conclusion
While Minnesota’s Medicaid growth during COVID-19 has helped to offset private health insurance coverage losses and the state’s program has done well with respect to coverage relative to many other states, the eventual end of the federal public health emergency will bring with it an end to special emergency Medicaid rules such as the moratorium on disenrollment. The public health emergency’s mandate of continuous eligibility was vital in the growth of Medicaid as a safety net. As the economy continues to recover and the federal public health emergency concludes as soon as the end of the year, we should see an increase in employer-sponsored insurance and a decrease in Medicaid enrollment due to the countercyclical nature of the program. It will be important to track Medicaid enrollment as these emergency rules are phased out to evaluate the impact of returning to standard enrollment and retention practices.
Further Reading
Pandemic’s Impact on Health Insurance Coverage in Minnesota was Modest by Summer 2020. (Minnesota Department of Health, May 2021)
Tracking Medicaid Enrollment Growth during COVID-19. (State Health and Value Strategies, February 2021)
1 MACPAC. (June 2020) Considerations for countercyclical financing adjustments in Medicaid. https://www.macpac.gov/wp-content/uploads/2020/06/Considerations-for-Countercyclical-Financing-Adjustments-in-Medicaid.pdf.
2 State Health and Value Strategies. (2021, February 25). Tracking Medicaid enrollment growth during COVID-19 databook. https://www.shvs.org/wp-content/uploads/2020/10/Tracking-Medicaid-Enrollment-Growth-During-COVID-19-Databook_03.2021.xlsx
3 Minnesota Department of Human Services. (2018). Medicaid Matters: The impact of Minnesota’s Medicaid Program [DHS-7659-ENG 2-18]. https://www.leg.mn.gov/docs/2018/other/180391.pdf
4 Office of Rural Health and Primary Care. (April 2017). Public and individual health insurance trends in rural Minnesota: enrollment during implementation of the Affordable Care Act. Minnesota Department of Health. https://www.health.state.mn.us/facilities/ruralhealth/pubs/docs/2017enroll.pdf
5 State Health Compare. (2021). Health Insurance Coverage Type. State Health Access Data Assistance Center (SHADAC). http://statehealthcompare.shadac.org/map/11/health-insurance-coverage-type-by-total#8/27/21
6 Minnesota Department of Health. (May 2021). Pandemic’s impact on health insurance coverage in Minnesota was modest by summer 2020. https://www.health.state.mn.us/data/economics/docs/inscoverage2020.pdf