Blog & News
BRFSS Spotlight Series: Adult Binge Drinking Rates in the United States (Infographic)
February 27, 2020:|
BRFSS SPOTLIGHT SERIES OVERVIEW |
Click on the infographic image to enlarge
Adult Binge Drinking*
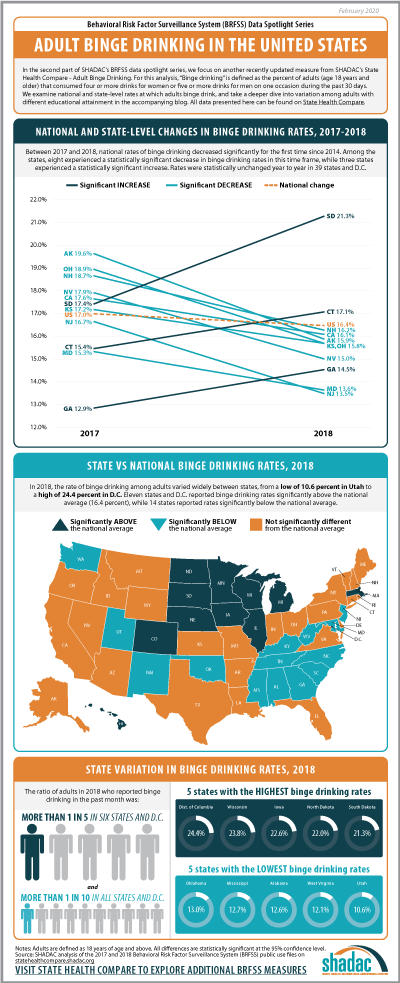
For this second post in our BRFSS Spotlight Series blog, we focus on an analysis of our Adult Binge Drinking measure (for which all differences described are statistically significant at a 95% confidence level unless otherwise specified). “Binge drinking” is defined by the Centers for Disease Control and Prevention (CDC) in the BRFSS as “drinking 5 or more drinks on an occasion for men or 4 or more drinks on an occasion for women" in the past 30 days.1
Over the past five years, adult binge drinking at the national level has increased a small but statistically significant amount from 16.0 percent in 2014 to 16.4 percent in 2018. For this analysis we also examined binge drinking by educational attainment, and found that adults (25 years and over) with a bachelor’s degree or higher in the U.S. reported a binge drinking rate of 15.7 percent in 2018, up from 15.3 percent in 2014 (percentage point difference was not statistically significant); and adults with less than a high school degree reported a rate of 13.5 percent in 2018, up from 12.8 percent in 2014.
Trends in Binge Drinking Rates from 2017 to 2018
Nationally, rates of binge drinking fell by 0.6 percentage points from 17.0 percent in 2017 to 16.4 percent in 2018—the first decrease since 2014. Statistically significant decreases in rates of binge drinking were seen in eight states: Alaska, California, Kansas, Maryland, New Hampshire, New Jersey, Nevada, and Ohio. Rates of binge drinking were statistically unchanged year to year in 39 states and D.C. Rates of binge drinking increased significantly in three states from 2017 to 2018: South Dakota, which experienced an increase of 3.9 percentage points (17.4 percent to 21.3 percent); Connecticut, which saw a 1.7 percentage-point increase (15.4 percent to 17.1 percent); and Georgia, with an increase of 1.6 percentage points (12.9 percent to 14.5 percent) between the two years.
State Variation (2018)
In 2018, rates of binge drinking varied widely between states, from a low of 10.6 percent in Utah to a high of 24.4 percent in D.C. Eleven states and D.C. reported rates of binge drinking above the national average (16.4 percent), and 14 states reported rates that fell below.
More than one in five adults reported binge drinking in the past month in six states—Iowa, Minnesota, Nebraska, North Dakota, South Dakota, and Wisconsin—and D.C., of which all but the latter were Midwest or Plains states.
Binge Drinking Rates across Education Levels+
Nationally, adults with less than a high school education were 14.1 percent less likely to report binge drinking compared to adults with a bachelor’s degree or higher level of education (13.5 percent vs. 15.7 percent).
Among the 48 states and D.C. where estimates of binge drinking among adults with a less than a high school education were statistically reliable^:
- Utah was both the only state where adults with less than a high school education were statistically more likely to report binge drinking than adults with a bachelor’s degree or higher, and also the state with the largest relative gap (89.2 percent) in binge drinking rates by education (14.7 percent vs. 7.8 percent).
- Adults with less than a high school education were statistically less likely to report binge drinking compared to adults with a bachelor’s degree or higher in 14 states, and the size of this gap varied from a low of 19.4 percent in Minnesota (15.1 percent vs. 18.8 percent) to a high of 56.6 percent in Missouri (7.8 percent vs. 17.9 percent).
- There was no statistically significant difference between these groups’ rates of binge drinking in 33 states and D.C.
This analysis follows recent trends reported by the Centers for Disease Control and Prevention, which indicates binge drinking is more common among people of higher educational levels and with household incomes of $75,000 or more. Individuals with lower incomes and educational levels in the U.S., however, consume more binge drinks (i.e., number of drinks in a binge drinking occasion) per year.2
Notes
All differences described in the post are statistically significant at the 95% confidence level unless otherwise specified.
* Rate of binge drinking among adults for the civilian noninstitutionalized population 18 years and over.
+ For the education analysis, adults are defined as those age 25 and older.
^ Estimates were considered statistically unreliable if the standard error was more than 30% as large as the estimate (i.e., RSE > 30%) - in this instance, estimates were statistically unreliable for Alaska and New Jersey.
References
1Centers for Disease Control and Prevention (CDC). (2020, January 2). Data on excessive drinking. Retrieved from https://www.cdc.gov/alcohol/data-stats.htm.
There is some differentiation between agencies (such as the CDC, National Institute of Alcohol Abuse and Alcoholism [NIAAA], and the National Institute of Health [NIH]) over whether binge drinking is defined as four drinks for women and five drinks for men on “one occasion” or “within a two-hour period,” but the question included in the BRFSS uses the “on one occasion” phrasing.
2 Kanny D, Naimi TS, Liu Y, Lu H, Brewer RD. (2018). Annual total binge drinks consumed by U.S. adults, 2015. Am J Prev Med, 54(4), 486-496.
Blog & News
BRFSS Spotlight Series: Adult Smoking and E-Cigarette Use in the United States (Infographic)
February 10, 2020:|
BRFSS SPOTLIGHT SERIES OVERVIEW |
Adult Smoking and E-Cigarette Use
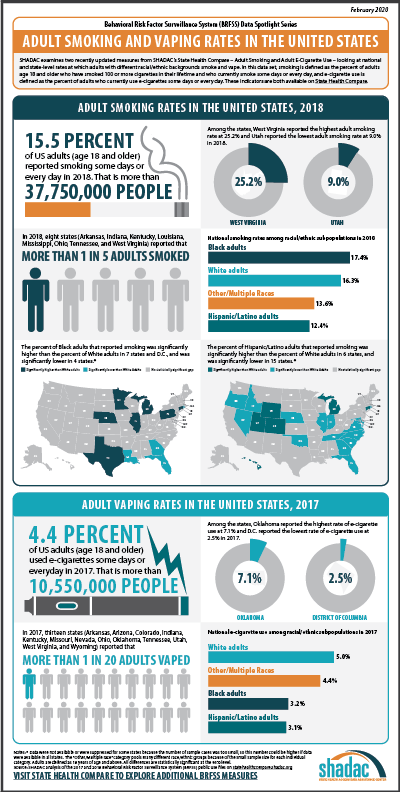 In the first part of our BRFSS spotlight series, we analyzed newly available 2018 data for an existing measure, Adult Smoking, and a more complete set of existing data from 2017 (as data for 2018 was not available in a majority of states) for a brand new measure, Adult E-Cigarette Use.
In the first part of our BRFSS spotlight series, we analyzed newly available 2018 data for an existing measure, Adult Smoking, and a more complete set of existing data from 2017 (as data for 2018 was not available in a majority of states) for a brand new measure, Adult E-Cigarette Use.
According to the Centers for Disease Control and Prevention and the World Health Organization, smoking was the leading cause of preventable death in 2017, with cigarette smoking being responsible for approximately 480,000 deaths per year in the United States.1
Lately, however, concerns around growth in tobacco use have shifted away from cigarette smoking—which has declined across the nation from a rate of 20.1 percent in 2011 to 15.5 percent in 2018—in response to the rise of vaping and e-cigarette use in recent years, especially among youth.2
Though vaping/e-cigarette use is thought to be less harmful compared to regular cigarettes,3 mounting concerns about the short- and long-term effects of such use have led researchers to conduct studies such as a recent analysis conducted by scholars at the University of California, San Francisco and published in the American Journal of Preventive Medicine, which finds growing evidence linking e-cigarette use and respiratory diseases.
As researchers continue to monitor individual and population-level trends in health behaviors, such as tobacco use, data from surveys such as the BRFSS will have an important impact in increasing our understanding of the consequences of smoking and e-cigarettes.
Adult Smoking (2018)
Smoking is defined as adults (age 18 and older) who have smoked 100 or more cigarettes in their lifetime and who currently report smoking “some days” or “every day.” Nationally, 15.5 percent of adults smoked some days or every day in 2018, which decreased significantly from a reported rate of 16.4 percent the previous year. Across the states (and the District of Columbia), smoking rates varied from a low of 9.0 percent in Utah to a high of 25.2 percent in West Virginia.
Eight states (Arkansas, Indiana, Kentucky, Louisiana, Mississippi, Ohio, Tennessee, and West Virginia) reported that more than one in every five adults smoked in 2018. In better news, data from eight states (Arizona, Florida, Louisiana, Maryland, New Mexico, New York, Vermont, and Washington) showed significant declines in adult smoking rates from 2017 to 2018, and no states experienced significant increases.
Smoking Patterns by Race/Ethnicity*
When looking at 2018 data across the nation by race/ethnicity, Black adults were 6.7 percent more likely to smoke than White adults (17.4 percent vs. 16.3 percent). Correspondingly, rates of smoking were higher among Black adults than among White adults in seven states (Connecticut, Illinois, Michigan, Minnesota, Nebraska, Pennsylvania, and Texas) as well as in D.C., and were only lower than the rate of White adults in four states (Florida, Georgia, Louisiana, and Rhode Island). The gap between smoking rates of Black and White adults was highest in D.C., where Black adults were more than two times more likely than White adults to smoke (21.8 percent vs. 6.9 percent).
Nationally, Hispanic/Latino adults were 23.6 percent less likely to report smoking compared to White adults (12.4 percent vs. 16.3 percent). Rates of smoking were higher among Hispanic/Latino adults than White adults in only six states (Colorado, Connecticut, Hawaii, Michigan, Utah, and Wyoming) and were lower than White adult smoking rates in 15 states. Hawaii was highest among states with a statistically significant gap, with Hispanic/Latino adults who were 83.7 percent more likely to smoke than White adults (21.4 percent vs. 11.6 percent).
For the adult smoking measure, we also analyzed national-level data for adults of Other/Multiple races, a category that includes those who identify as American Indian or Alaska Native, Asian, Native Hawaiian/Pacific Islander, Other race, or Multiracial.+ The national data showed that, overall, Other/Multiracial adults were 16.4 percent less likely to smoke than White adults (13.6 percent vs. 16.3 percent). Of this group, American Indian or Alaska Natives were most likely to report smoking at 29.1 percent, followed by Multiracial adults (23.5 percent), Native Hawaiian/Pacific Islanders (21.8 percent), adults reporting as “Other” (16.9 percent), and Asian adults having the lowest smoking rate at 7.7 percent. A high-level state analysis also revealed that Other/Multiracial adults had the highest rates of smoking in 26 states over White adults, Black adults, and Hispanic/Latino adults.
Adult E-Cigarette Use (2017)
E-Cigarette use is the newest measure that has been added to SHADAC’s State Health Compare web tool. The measure is defined as adults who currently report using e-cigarettes either “some days” or “every day.” Due to the fact that data are not available for all states in 2018, this analysis uses 2017 data in order to give a more complete picture of trends in e-cigarette use across the nation.
Nationally in 2017, 4.4 percent of adults used e-cigarettes—a rate that was statistically unchanged from 4.5 percent in 2016. Among the states, e-cigarette use ranged from a low of 2.5 percent in D.C. to a high of 7.1 percent in Oklahoma. Thirteen states (Arkansas, Arizona, Colorado, Indiana, Kentucky, Missouri, Nevada, Ohio, Oklahoma, Tennessee, Utah, West Virginia, and Wyoming) reported an e-cigarette use rate of more than one in every twenty adults in 2017. Just one state (Indiana) saw an increase in rates of e-cigarette use, while five states (Connecticut, Louisiana, Massachusetts, Nebraska, and Washington) saw decreases in rates of e-cigarette use.
Nationally, 3.2 percent of Black adults reported using e-cigarettes in 2017, a rate that was 36.5 percent less than White adults, who had an e-cigarette use rate of 5.0 percent. Hispanic/Latino adults reported e-cigarette use at 3.1 percent, a rate that was 38.2 percent less than White adults (5.0 percent), and Other/Multiracial adults’ reported e-cigarettes use that same year was 11.4 percent less than White adults (5.0 percent) at 4.4 percent.
As e-cigarette use becomes more of public health focus, and as more state and federal surveys field questions about this topic, SHADAC will continue to monitor available data for future analysis involving state-level trends in e-cigarette use.
A brief on Adult Smoking and E-cigarette Use at the national and state levels is currently planned for release some time later this year, and will include a deeper analysis of these data.
Notes
All data are from SHADAC analysis of the Behavioral Risk Factor Surveillance System (BRFSS). All differences described in the post are statistically significant at the 95% confidence level unless otherwise specified.
* Data breakdowns by race/ethnicity for smoking rates were not available in all states due to sample size limitations.
+ The “Other/Multiple race” category pools many different race/ethnic groups because of the small sample size for each individual category.
1 Centers for Disease Control and Prevention (CDC). (2019, November 15). Smoking and tobacco use: Fast facts. Retrieved from https://www.cdc.gov/tobacco/data_statistics/fact_sheets/fast_facts/index.htm
World Health Organization (WHO). (2017, July 19). WHO report on the global tobacco epidemic, 2017. Available from https://www.who.int/tobacco/global_report/2017/en/
Blog & News
Now Available on State Health Compare: Eleven Updated Measures and One Brand New Measure
December 3, 2019:Estimates for measures from a variety of categories (Health Outcomes, Health Behaviors, Access to Care, Cost of Care, and Social and Economic Factors, etc.) have now been updated on SHADAC’s State Health Compare web tool. All measures now contain data for 2018, the most recent year available. State Health Compare has also added a brand new measure, Adult E-Cigarette Use.
Updated Measures Include:
Income Inequality
Using the Gini coefficient (a summary of the dispersion of income across the entire income distribution), this measure gauges disparities in income in each state on a scale from 0 to 1, with higher values indicating greater inequality and lower values indicating the opposite. Estimates for all states are now available from 2006 through 2018.
Sales of Opioid Painkillers
This measure captures the rate of legal prescription opioid painkiller sales in kilograms per 100,000 people per year for both hydrocodone and oxycodone—the most common types of prescription opioids. Data is now available for all states from 2000 through 2018.
Adults Who Forgo Needed Medical Care*
The measure indicates the percent of adults (18+) in each state who could not get needed medical care due to cost. Breakdowns by education level and race/ethnicity are available for all states from 2005 through 2010 and 2011 through 2018.
Adults With No Personal Doctor*
This measure denotes the percent of adults without a personal doctor and is now available for all states from 2005 through 2010 and 2011 through 2018. Breakdowns by education level and race/ethnicity are also available.
Adult Cancer Screenings*
The measure is an indication of the percent of adults who have received recommended cancer screenings (e.g., colorectal screenings, mammograms, pap smears, etc.) in the past year, and is now available for all states from 2005 through 2010 and 2011 through 2018.
Chronic Disease Prevalence*
This measure captures the percent of adults who reported having one or more common chronic conditions such as diabetes, cardiovascular disease, heart attack, stroke, and asthma, in each state. Estimates are now available for all states from 2005 through 2010 and 2011 through 2018.
Activities Limited due to Health Difficulty*
This measure reports the average number of days (in the last 30 days) for which an adult indicates limited activity due to mental or physical health difficulties. It is now available for all states from 2005 through 2010 and 2011 through 2018.
Adult Obesity*
The measure is an indication of the prevalence of obesity, defined as a Body Mass Index (BMI) > 30, among the adult population 18 years of age and over. It is now available for all states from 2005 through 2010 and 2011 through 2018.
Adult Binge Drinking*
This measure indicates the percent of adults who, on one occasion, have consumed at least four drinks (women) or five (men) or more in the past 30 days. Now available for all states from 2005 through 2010 and 2011 through 2018, the measure includes breakdowns by education level and race/ethnicity.
Adult Smoking*
This measure indicates the percent of adults over 18 years of age who have smoked 100 or more cigarettes in their lifetime, and who currently smoke some days or every day. It is now available for all states from 2005 through 2010, and 2011 through 2018.
Adult E-Cigarette Use (Newly available measure on State Health Compare)
This measure indicates the percent of the adult population (18 years of age and over) who currently use e-cigarette some days or every day. It is now available for all states from 2016 through 2017 and for most states for 2018. Breakdowns are available by education level and race/ethnicity.
Data Sources
The State Health Compare estimates for income inequality come from the American Community Survey (ACS); the sales of opioid painkillers comes from the U.S. DEA’s Automated Reports Consolidated Ordering System Retail Drug Summary Reports; and the measures of chronic disease prevalence, activities limited due to health difficulty, and the adults who forgo needed medical care, adults with no personal doctor, and adult cancer screenings, obesity, binge drinking, smoking, and e-cigarette use measures all come from the Behavior Risk Factor Surveillance System (BRFSS).
Notes
All measures marked with an “*”: This indicates a break in series due to the BRFSS implementing cell phone sampling and an advanced weighting method in 2011.
Blog & News
Minnesota's Growing and Evolving Opioid Crisis
October 28, 2019: On Thursday, October 24, SHADAC Senior Research Fellow Colin Planalp presented a data-focused look at Minnesota’s opioid crisis during the University of Minnesota’s Medical Industry Leadership Institute “Combating Minnesota’s Opioid Epidemic” policy forum. Colin shared the stage with experts in a variety of arenas and policy levels including state and federal legislators and local stakeholders, as well as health insurers, health care providers, and payers, for this one-day event aimed at learning from and building on current efforts to successfully combat the opioid epidemic.
On Thursday, October 24, SHADAC Senior Research Fellow Colin Planalp presented a data-focused look at Minnesota’s opioid crisis during the University of Minnesota’s Medical Industry Leadership Institute “Combating Minnesota’s Opioid Epidemic” policy forum. Colin shared the stage with experts in a variety of arenas and policy levels including state and federal legislators and local stakeholders, as well as health insurers, health care providers, and payers, for this one-day event aimed at learning from and building on current efforts to successfully combat the opioid epidemic.
Across the states, the opioid crisis varies widely—both in the range of opioid death rates and in differences regarding the types of opioids that cause the most deaths (prescription opioid painkillers, heroin, synthetic opioids, etc.). For example, deaths from synthetic opioids, such as fentanyl, ranged from a low of 1.2 per 100,000 people in Kansas and Texas in 2017 to a high of 37.4 deaths per 100,000 people in West Virginia—a difference of more than 30 times (Figure 1).
Figure 1. State Synthetic Opioid Death Rates per 100,000 People, 2017
In 2017, Minnesota had one of the lowest overdose death rates among all 50 states for synthetic opioids, at 3.5 deaths per 100,000 people, which was also significantly lower than the U.S. rate of 9.0 deaths per 100,000 people (Figure 2). Minnesota’s death rates from heroin and prescription opioid painkillers also were significantly lower than the U.S. rate in 2017 (not shown).
Figure 2. State vs. National Synthetic Opioid Death Rates per 100,000 People, 2017
Although Minnesota has not been hit as severely as many other states, it would be wrong to assume the opioid crisis isn’t a problem in the state. Since 2000, the number of deaths attributed to opioid overdoses has increased nearly seven times, from 54 to 422 in 2017 (Figure 3).
Figure 3. Number of Opioid Overdose Deaths in Minnesota, 2000-2017
Despite common misconceptions about the kinds of communities affected by the opioid crisis—either that it’s only an urban problem or only a rural problem—data on opioid overdose deaths show that Minnesota’s opioid crisis isn’t limited geographically. Since 2000, opioid deaths have increased substantially in both the seven-county Twin Cities region and outside the Twin Cities in greater Minnesota. In the Twin Cities Metro, opioid deaths increased about 5.5 times, from 43 in 2000 to 280 in 2017; and they grew almost 12 times in greater Minnesota, from 11 to 142 deaths during the same time period (not shown).
A map of Minnesota counties paints a similar picture. During the three years from 2000-2002, only one of Minnesota’s 87 counties had an opioid death rate of more than 4.0 deaths per 100,000 people, but during the period from 2014-2016, most of the state’s counties (46 of 87) had an opioid death rate of more than 4.0 deaths per 100,000 people (Figure 4).
Figure 4. Opioid Overdose Death Rates per 100,000 People by Minnesota Counties, 2000-2002 and 2014-2016
Preliminary data on opioid overdose deaths published by the Minnesota Department of Health suggest that Minnesota may be turning a corner. If the preliminary data regarding overdose deaths hold accurate in the final count, Minnesota will experience a drop in total opioid overdose deaths in 2018 compared with 2017—only the second time that has happened since 2000. Despite that encouraging sign, however, the data show continued reasons for serious concern:
- First, even with a decline in 2018, the provisional data showing more than 300 opioid overdose deaths last year still represents a near-historic high.
- Second, while the total number of opioid overdose deaths may have declined, deaths from certain types of opioids continued to climb, with nearly 200 deaths resulting from synthetic opioids recorded in 2018.
- Third, drug overdose death data from Minnesota show signs that the opioid crisis may be spreading to non-opioid substances, such as methamphetamine and cocaine—a trend consistent with data for the U.S. and for other states. Minnesota’s 2017 and provisional 2018 data show cocaine and psychostimulant (e.g., methamphetamine) deaths at or near historic highs (Figure 5).
Figure 5. Number of Opioid Overdose Deaths in Minnesota, 2000-2018 (preliminary)