Blog & News
Updates to Minnesota's Community and Uninsured Profile Resource to Reflect 2016-2020 ACS Estimates
June 2, 2022: Following the release of the 2020 U.S. Census Bureau’s American Community Survey 5-year data file (2016-2020), SHADAC has made important updates to the Minnesota Community and Uninsured Profile resource to incorporate an analysis of the 2020 data.
Following the release of the 2020 U.S. Census Bureau’s American Community Survey 5-year data file (2016-2020), SHADAC has made important updates to the Minnesota Community and Uninsured Profile resource to incorporate an analysis of the 2020 data.
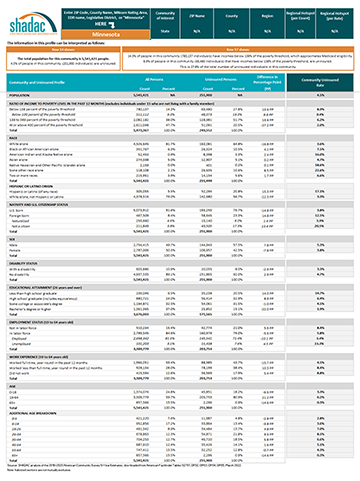 The Community and Uninsured Profile can be used in two ways: (1) to support other equity-focused work, advocacy work, strategic planning, community needs assessments, and grant-writing, and (2) to target health insurance coverage outreach and enrollment efforts.
The Community and Uninsured Profile can be used in two ways: (1) to support other equity-focused work, advocacy work, strategic planning, community needs assessments, and grant-writing, and (2) to target health insurance coverage outreach and enrollment efforts.
The Community and Uninsured Profile provides rates and counts of Minnesotans at a range of geographic levels. Users can explore characteristics of the total population and the uninsured population in a specific ZIP code while also overlaying in-depth community characteristics. In addition, users can look at rates and characteristics of the community and uninsured within the state as a whole, by region, county, and state legislative district. Users can also filter by MNsure rating areas -- the geographic regions health insurers use to set premiums on MNsure.
This resource was originally developed as part of “Minnesota’s Uninsured and the Communities in Which They Live,” a project funded by the Blue Cross Blue Shield Foundation of Minnesota that supports targeted outreach and enrollment activities of health insurance navigators and provides information about the uninsured to Minnesota policymakers as they develop strategies to reach the remaining uninsured in Minnesota.
To download the Profile, access additional information, or request the development of a similar tool for another state, visit the Minnesota Community and Uninsured Profile Resource page.
Blog & News
State and Federal Relief Prevented Deep Backslide in Health Care Affordability in California in 2020 (CHCF Cross Post)
May 18, 2022:The following content is cross-posted from California Health Care Foundation. It was first published on May 18, 2022.
Author: Colin Planalp, Research Fellow, SHADAC
In 2020, the start of the COVID-19 pandemic meant the imposition of incredible burdens on every corner of US society, particularly the health care system and the people it serves. There were well-founded fears that the pandemic, and the concurrent economic crisis, could make health insurance and health care unaffordable for even more people — already a long-standing problem in California.
In response to the pandemic, the US government enacted historic relief programs, including multiple instances of direct cash payments to a majority of US families. Those federal policies coincided with California health insurance reforms that, while developed before the pandemic, were implemented in 2020.
This analysis of the California Health Insurance Survey (CHIS) shows that Californians were largely protected from experiencing a major erosion in their ability to pay for health insurance and care. Despite this overall positive finding, the 2020 CHIS data on health care affordability continued to demonstrate clear inequities by income and race/ethnicity.
Key Findings
California’s uninsured rate declines, yet cost remains top reason for lacking health insurance. The rate of Californians under 65 without health insurance reached a historic low of 7.0% in 2020. However, 51.9% of uninsured people said they lacked coverage because it was too expensive.
Rate of going without needed care due to cost dropped in 2020. Among the 8.6% of Californians who reported forgoing needed medical care in 2020, 32.0% said it was concerns about the cost that caused them to go without care. That rate was significantly lower than the rate of 43.6% in 2019.
Fewer Californians reported difficulty paying medical bills. From 2019 to 2020, the rate of Californians reporting that they’ve had trouble paying medical bills in the past year declined significantly, from 13.3% to 11.1%. However, when breaking out the data by income, only those with higher incomes saw statistically significant improvement. Californians with lower incomes — 200% to 299% of federal poverty guidelines (FPG), 100% to 199% FPG, and below 100% FPG — reported no significant changes.
Less trouble affording necessities due to medical bills in 2020. In 2020, the rate of Californians who reported having trouble paying for basic necessities (such as food or clothing) because of medical bills declined significantly to 31.0% from 39.8% in 2019. Rates of trouble paying for necessities due to medical bills also declined across most income levels.
Practice of using credit card debt to finance medical bills declined. In 2020, the rate of Californians who reported taking on credit card debt to finance medical bills declined significantly, from 56.5% in 2019 to 44.3%. That finding held consistent for Californians across income levels — except for those with the lowest incomes.
Racial and ethnic disparities persisted in 2020. Although California experienced significant improvements in some measures of health care and insurance affordability in 2020, certain long-standing inequities persisted. For example, Black people reported the highest rate of trouble paying medical bills in 2020, at 14.0%, followed closely by Latinos/x, at 12.7%. Asians, Black people, and Latinos/x also reported similarly high rates of trouble paying for necessities due to medical bills (39.4%, 36.2%, and 33.1%, respectively).
Together, these findings provide some encouraging news. In a year of massive economic upheaval that would typically have caused serious financial problems for many Californians, they instead reported improvements in health care and insurance affordability. However, improvements were likely due, at least in part, to federal programs that were mostly designed to be temporary. Some have already expired. Additionally, the historically high inflation of 2021 and 2022 have since strained people’s finances.
But the fact that California experienced such measurable improvements in health insurance and health care affordability during a broad and deep recession shows that those problems don’t have to be intractable. In the future, it will be key to monitor these measures as policymakers in California and at the federal level consider initiatives to protect people against unaffordable health care and insurance costs, which remain a long-term challenge.
Blog & News
2021 NHIS Full-Year Health Insurance Estimates Early Release: Coverage Rates Remain Stable Overall, Changes Visible across Demographic Groups (Infographic)
May 10, 2022:The National Center for Health Statistics (NCHS) released health insurance coverage estimates for 2021 from the National Health Interview Survey (NHIS) as part of the NHIS Early Release Program. The estimates captured in this report are some of the first available coverage estimates for 2021 from a federal survey.
National-level estimates are available by breakdowns including age, sex, poverty status, race and ethnicity, and by state Medicaid expansion status. The NHIS full-year estimates for 2021 do not include either full or partial state-level data, as has been the case since the survey was redesigned in 2019. However, NCHS periodically releases state-level estimates of coverage, which SHADAC has previously covered on our blog and will continue to monitor and report on any future releases.
Changes between the 2020 and 2021 coverage estimates were minimal when examining rates of private coverage and those without health insurance coverage. However, the 2021 report indicates a slight uptick in public coverage which is consistent with trends in survey and administrative data since the start of the coronavirus (COVID-19) pandemic in the United States. The rates across all coverage types experienced several more notable shifts when examined by sex as well as race and ethnicity.
Changes in the NHIS
The COVID-19 pandemic significantly impacted 2020 NHIS field procedures (including interview format), response rates, and resulting data analytic files, though NCHS found minimal nonresponse bias in the 2020 NHIS. A recent SHADAC issue brief reported on these and other changes to federal surveys that were similarly impacted by the pandemic.
It is also worth noting that 2021 NHIS coverage estimates are based on information collected from 29,696 sample adults and 8,293 sample children. In 2019, the NHIS underwent a substantial redesign of its content and structure and one of the largest changes, the elimination of the family questionnaire, has resulted in a substantial reduction of the available sample size for the survey (though the NCHS also estimates a positive effect on higher response rates). It is likely that a survey with a larger sample size would find more significant year-over-year changes in coverage rates.
Notes on Race and Ethnicity Estimates from NHIS
The NHIS Early Release report from which the figures for the race/ethnicity category are drawn does not further disaggregate statistics by more detailed race and ethnicity categories. Individuals not identifying as Hispanic; non-Hispanic White, Black, or Asian; or identifying with multiple, non-Hispanic race categories are classified as “multiple races or any other race.”
Additionally, there are many factors that historically widen disparities in coverage across race and ethnicity; race-based discrimination in employment and systemic racism are two possible contributors.
Other NHIS analyses from 2022
- 2022 NHIS Early Release: Estimates for First Half of the Year Show Continued Fall of Uninsured Rates (Blog) December 2022
- 2022 NHIS Early Release: Quarter 1 estimates show potential post-pandemic rebounds (Blog) August 2022
- NHIS: National Rates of Health Insurance Coverage for Third Quarter of 2021 Statistically Unchanged from 2020 (Blog) January 2022
Source
Cohen, R.A., Cha, A.E., Terlizzi, E.P., & Martinez, M.E. (2022, May 5). Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2021. National Center for Health Statistics (NCHS). https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur202205.pdf
Blog & News
Minnesota’s uninsured rate hit historic low in 2021 but racial disparities increased (Minnesota Department of Health Cross Post)
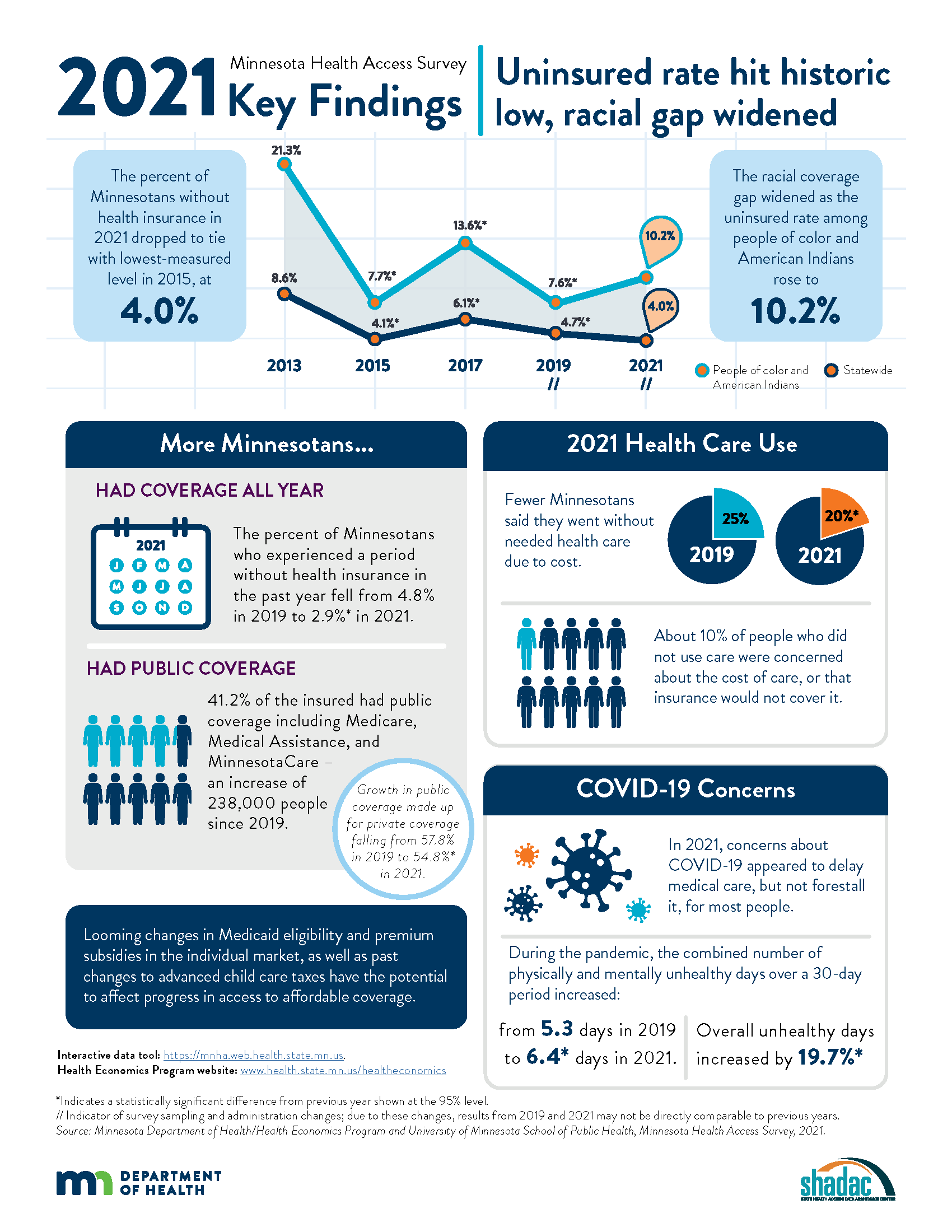
July 14, 2022:Today, the Health Economics Program (HEP) of the Minnesota Department of Health (MDH) and the University of Minnesota School of Public Health, State Health Access Data Assistance Center (SHADAC) released results from the 2021 Minnesota Health Access Survey (MNHA) - a biennial state-based population survey that collects information on how many people in Minnesota have health insurance and how easy it is for them to get health care. The survey is conducted as a partnership between MDH and SHADAC.
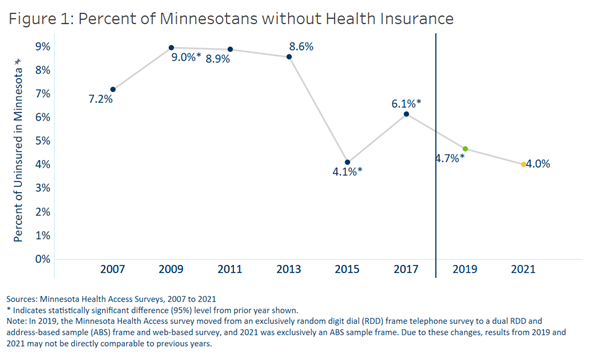
Key findings from the survey showed mixed results, with the statewide uninsured rate dropping to its lowest-ever rate (4.0%) and periodic uninsurance dropping significantly (2.9% from 4.8%). However, the survey also found that disparities in coverage increased when examined by race and ethnicity, with uninsured rates among American Indians and people of color rising to 10.2%.
The following content from the full press release is cross-posted from the Minnesota Department of Health published on April 21, 2022.
Authors: Alisha Simon, MDH; Stefan Gildemeister, MDH; Kathleen Call, SHADAC
The Minnesota Department of Health (MDH) released new data showing mixed news regarding health insurance coverage in Minnesota during 2021. While actions taken by state officials helped drop the state’s uninsured rate to the lowest level ever measured, racial disparities in coverage worsened.
Federal and state policies and funding during 2021 shielded Minnesota’s health insurance coverage against the pandemic’s economic shock. With the help of these efforts, the state’s uninsured rate fell to 4.0%, the lowest-ever measured level, essentially tying the 2015 rate.
Economic downturns often result in higher rates of uninsurance in the U.S. due to the link between employment and health insurance coverage. With the help of state and federal funding, Minnesota took steps to prevent insurance loss in 2020 and 2021, including government efforts to maintain coverage for low-income Minnesotans and premium subsidies in the individual market. Data from the Minnesota Health Access Survey found that 34,000 fewer Minnesotans went without health insurance in 2021 compared to 2019. Fewer Minnesotans also said they went without some type of needed health care due to cost in 2021 (20%) compared to 2019 (25%).
However, not all Minnesotans were equally able to access or retain coverage. Racial disparities worsened as the uninsured rate among Minnesotans of color and American Indians rose from 7.6% in 2019 to 10.2% in 2021. In contrast, the uninsured rate dropped among non-Hispanic Whites from 3.7% in 2019 to 2.4% in 2021.
“The investments we made before and during the pandemic to ensure Minnesotans had access to affordable health coverage helped more people stay insured, even in the midst of job losses and economic instability,” said Minnesota Commissioner of Health Jan Malcolm. “Sadly, we saw that people of color and American Indians did not benefit as much from these efforts. We must learn about what worked and what didn’t so we can adapt our approach to reach the goal of ongoing and equitable access to affordable health care for all Minnesotans.”
The number of Minnesotans with public insurance increased by 238,000 so that 41.2% of those insured had coverage through public sources in 2021, including Medicare, Medical Assistance and MinnesotaCare. This growth in public coverage made up for a decrease in private coverage – down from 57.8% in 2019 to 54.8% in 2021.
While most Minnesotans weathered the first two years of the pandemic with health insurance, there are concerns about maintaining coverage moving forward. Many government programs that added financial supports to families, increased subsidies for private health insurance plans sold through MNsure to make insurance more affordable or allowed people to stay on Medicaid longer ended or are set to expire this year.
“Historically, Minnesota has enjoyed a strong labor market and a strong employer-sponsored insurance market,” said Kathleen Call, a professor with the University of Minnesota School of Public Health and an investigator at the State Health Access Data Assistance Center. “However, alongside the crisis of the pandemic, the long-term erosion of private coverage over the past two decades, combined with the fact that not all employees are offered insurance and not all Minnesotans can afford it, reminds us that continued commitments are needed to support and promote Medical Assistance, MinnesotaCare and premium subsidies in the individual market available through MNsure.”
The survey suggests that COVID-19 had an impact in delaying care in 2021 but didn't keep most people from getting that care eventually. In the second year of the pandemic, COVID-19 concerns affected only 8% of people not receiving health care. The primary reasons for not using health care were cost or not needing it.
Both physical and mental health declined during the pandemic, according to the survey. The number of unhealthy days reported for a 30-day period climbed to an average 3.3 days for physical health and 4.3 days for mental health, compared to 2.8 for physical health and 3.7 for mental health in 2019.
“The reports of Minnesotans having fewer healthy days in 2021 are concerning, particularly in light of the continued strain on the state’s health care workforce and our structural weaknesses in mental health care,” said Stefan Gildemeister, MDH state health economist. “We will continue to monitor how effective our investments in community connections and resources during the pandemic are in reversing lingering harms to physical and mental health as the state moves into the next stage of the pandemic and as the economy recovers.”
The Minnesota Health Access Survey is a biennial state-based population survey that collects information on how many people in Minnesota have health insurance and how easy it is for them to get health care. The survey is conducted as a partnership between MDH and the University of Minnesota School of Public Health, State Health Access Data Assistance Center. The survey had responses from more the 18,000 Minnesotans across the state and was conducted between October 2021 and January 2022. More findings from the survey are available on the MDH Health Economics Program website.
Additional Resources
MDH Uninsurance Chartbook MNHA 2021 Survey Infographic MNHA Survey Tool
Publication
New SHADAC Brief Summarizes Study of Effects of Medicaid Expansion on Physician Participation
With the Affordable Care Act's (ACA) expansion of Medicaid, approximately 15 million people were able to enroll in the program - many of whom were previously uninsured. However, researchers have long worried that an expansion of insurance coverage would not translate to an equal expansion in access to care. A particular point of concern is the worry that these newly eligible and enrolled individuals would not be able to find enough physicians who participate in Medicaid to treat them.
Existing research has traditionally relied on physician survey data to study trends in physician acceptance of Medicaid and the factors associated with participation in the Medicaid program. For example, under contract with the Medicaid and CHIP Payment and Access Commission (MACPAC), SHADAC researchers used data from the National Electronic Health Records Survey (NEHRS) to create state-level estimates of physician participation in Medicaid before and after expansion and to study the physician- and practice-level characteristics associated with participation.
However, a new study led by Dr. Hannah Neprash is the first to provide direct answers about how clinicians responded to the Medicaid expansion. In their paper, "The effect of Medicaid expansion on Medicaid participation, payer mix, and labor supply in primary care” published in the December 2021 issue of the Journal of Health Economics, Dr. Neprash and her co-authors use all-payer claims and practice management data from 2012 through 2017 to examine how clinicians changed their labor supply and payer mix in response to Medicaid expansion.
This brief summarizes key findings from this study, including the effect of expansion on the number of Medicaid appointments and number of Medicaid patients seen by primary care clinicians (i.e., Medicaid participation), the total number of appointments provided (i.e., their labor supply) and the share of those appointments paid for by Medicaid versus private coverage or other payers (i.e., payer mix). The study also compares the relative change in participation in states subject to the Medicaid expansion compared to the change in states not subject to the expansion, estimating a causal effect of expansion on clinician participation in Medicaid.
Click on the image to the upper right to access and download a PDF of the full brief.
Related Resources
Physician Acceptance of New Medicaid Patients: Findings from the National Electronic Health Records Survey (MACPAC Fact Sheet)
Explore Physician Acceptance of New Medicaid Patients through Two New Measures on SHADAC’s State Health Compare and in a New MACPAC Factsheet (SHADAC Blog)
Physicians who accept new Medicaid patients (State Health Compare Data Measure)