Blog & News
Examining Gender-Based Discrimination in Health Care Access by Gender Identity in Minnesota
December 9, 2022:Authors: Jeremy Duval, Natalie Mac Arthur, Kathleen Call
DefinitionsCisgender/cis: A person whose gender identity corresponds with their sex assigned at birth. Transgender/trans: A person whose gender identity differs from their sex assigned at birth. Non-binary: An umbrella term for a person whose gender identity is not binary (male or female). |
Introduction
Many barriers exist to creating an equitable health care experience for LGBTQ+ individuals. One critical barrier is gender-based discrimination from providers within health care systems. The biennial 2021 Minnesota Health Access Survey (MNHA) asked respondents how often their gender, sexual orientation, gender identity, or gender expression causes health care providers to treat them unfairly. We compared rates of gender-based discrimination and health care access in the Minnesota adult population and examined differences in access to care among cisgender (cis) and gender minorities who report gender-based discrimination (see Definition Box). We explored the impact of gender-based discrimination on health care access by comparing access rates among people who did and did not experience discrimination for cis men, cis women, transgender and non-binary populations in Minnesota.
Results
The majority (58.9%) of transgender (trans) and non-binary respondents reported experiencing gender-based discrimination from health care providers in 2021—a stark contrast from the statewide average of 6.0% (Figure 1). Cis women also reported gender-based discrimination (7.7%) above the population average, while cis men were less likely to experience this form of discrimination (2.9%). Gender-based discrimination was especially high for both non-binary (63.9%) and trans (48.8%) respondents. Due to sample size limitations, these populations were combined in the remainder of our analyses.
Figure 1. Unfair treatment from health care providers based on gender in Minnesota
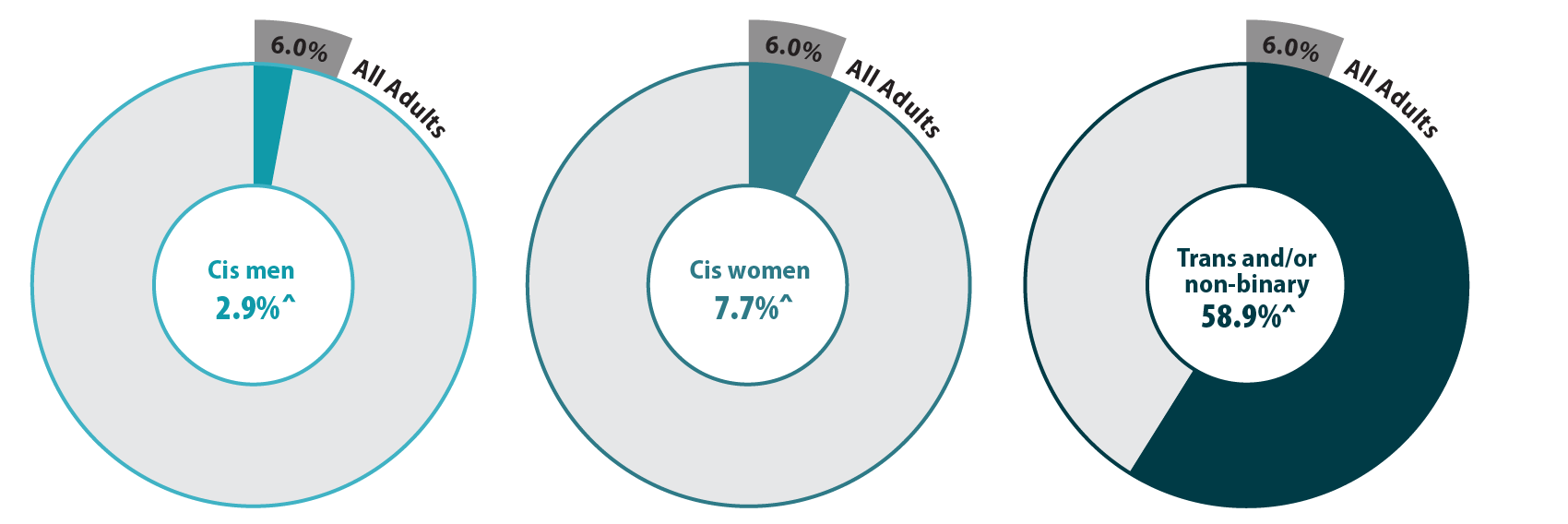
^ Rate significantly different from All Adults at the 95% confidence level.
Source: SHADAC analysis of the 2021 Minnesota Health Access Survey.
We also found differences in health care access among trans and non-binary people compared with the adult Minnesota population, particularly for confidence in getting care and forgoing needed care due to cost (Figure 2). We found that trans and non-binary respondents were similar to cis men in rates of having a usual source of care and having a medical visit (non-emergency) in the past year. Compared with the adult population in Minnesota, cis men were more likely to lack these forms of care, while cis women had better access to regular medical visits and a usual source of care. However, differences from the state average did not reach significance for trans and non-binary respondents, likely due to small sample size. Nearly a third (30.1%) of trans and non-binary adults had low confidence in getting necessary care compared to an average of 11.8% for adults in Minnesota. Over half (57.1%) of trans and non-binary people reported forgone care—more than double the average (26.2%).
Figure 2. Health care use and barriers to care
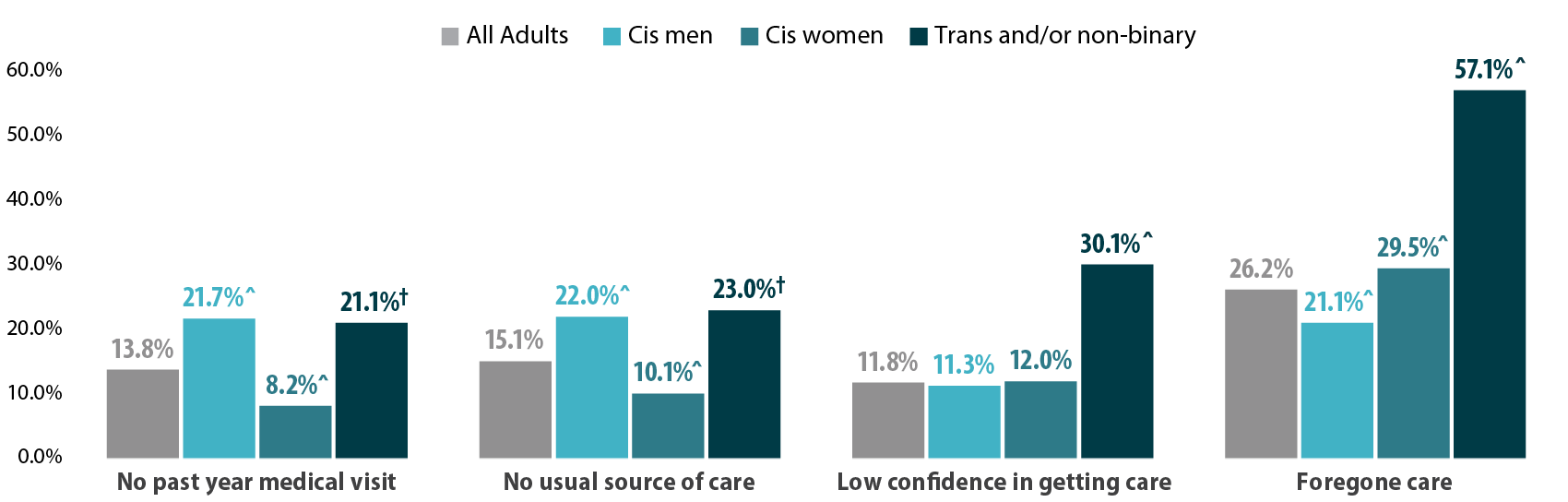
^ Rate significantly different from All Adults at the 95% confidence level.
† Estimate may be unreliable due to limited data (relative standard error greater than or equal to 30%).
Source: SHADAC analysis of the 2021 Minnesota Health Access Survey.
Figure 3. Experiences of gender-based discrimination associated with barriers to health care access
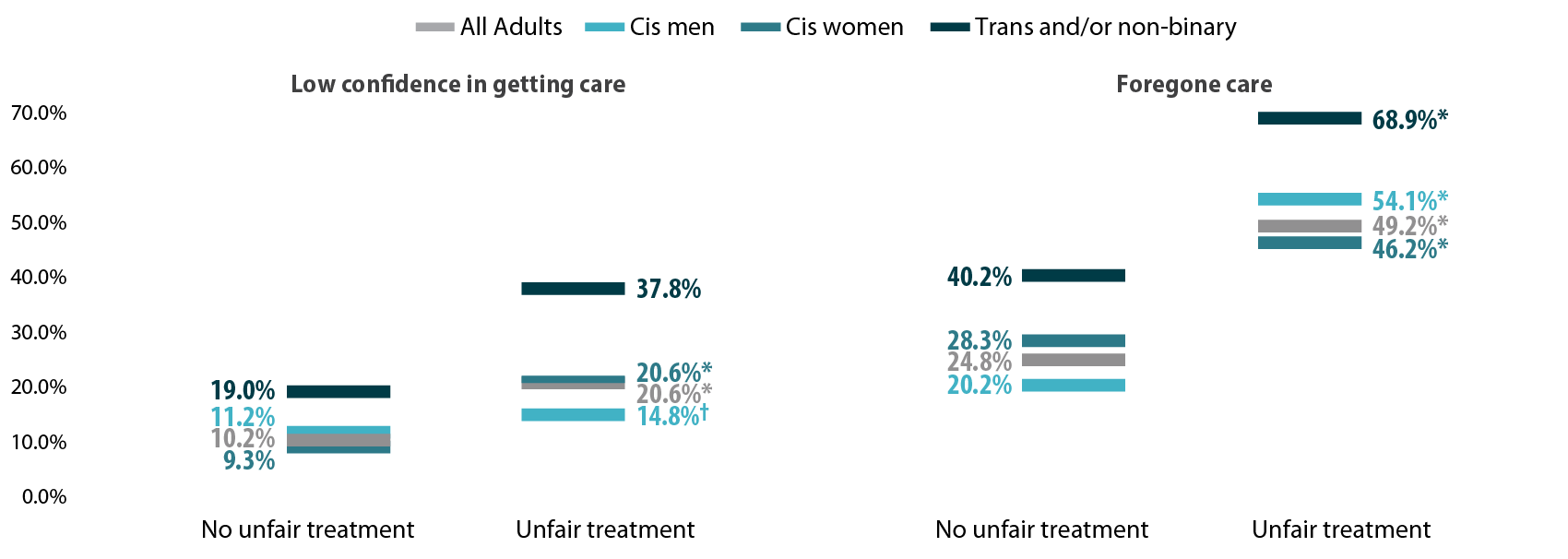
* Significant difference within a given subpopulation between rates of people who experienced unfair treatment and those who did not.
† Estimate may be unreliable due to limited data (relative standard error greater than or equal to 30%).
Source: SHADAC analysis of the 2021 Minnesota Health Access Survey.
Discussion
A worryingly high proportion of trans and non-binary adults reported gender-based discrimination and had forgone care or did not have confidence in getting needed care. This lack of confidence could be in part due to experienced or anticipated discrimination within a health care setting. Barriers to care were especially high among those who had experienced gender-based discrimination, which suggests that discrimination has a serious negative impact on health care access for trans and non-binary people.
We found higher rates of gender-based discrimination (58.9%) among trans and non-binary adults in Minnesota in 2021 compared to previously published literature on gender-based discrimination. National data indicate that between 20% and 40% of LGBTQ+ Americans experience discrimination while accessing health services (Kattari & Hasche, 2016), (Kachen & Pharr, 2020), (Penrose et al, 2020), (Rodriguez, Agardh & Asamoah, 2018), (Shires & Jaffee, 2015). Additionally, over 20% of the LGBTQ+ population avoided seeking health care due to anticipated discrimination (Kcomt et al, 2020). Notably, the majority of previously published estimates of trans peoples’ experiences of health care discrimination come from the National Transgender Discrimination Survey, which was conducted in 2016 and provides rich data, but for a specialized and non-probability sample. Such data are not considered generalizable. A strength of the MNHA survey is that it measures discrimination using a probability sample of adults reporting their gender identity.
Gender-based discrimination is just one factor affecting health care access. Gender minorities may additionally face disproportionate rates of other key barriers to access, such as lack of insurance coverage (Gonzales & Henning-Smith, 2017). Regardless, we found large gaps in health care access for trans people, non-binary people, and all people who experienced gender-based discrimination.
Conclusion
When the majority of a population is experiencing discrimination within health care systems, it is clear that change is necessary. Our data, based on a probability sample of Minnesotans, helps address gaps in knowledge about barriers transgender and non-binary adults face in accessing health care. The high rates of gender-based discrimination among gender minorities illustrate that gender-inclusive data collection is important for health equity.
However, quantifying rates of discrimination only scratches the surface of the true problem. Because of the limited sample size of gender minority adults, we were unable to explore the role of other social factors in gender-based discrimination and health care barriers by gender identity. Race, ethnicity, and class likely intersect to exacerbate experiences of discrimination and barriers to care for gender minorities. For example, Black and American Indian/Alaskan Native transgender women face disproportionate rates of victimization, and these experiences may impact their health care needs and intensify barriers to accessing care (Reisner, 2018). In this analysis, we only looked at gender identity; our future studies will look at sexual orientation with a similar lens and examine these two together.
One of the largest barriers to understanding discrimination and its effects on health access is data collection. Not all surveys collect and report inclusive data on gender identity, which makes it very hard to track access for trans and non-binary people. Even when gender-inclusive data are available, gender-based discrimination is rarely measured. Direct measurement of discrimination is essential for monitoring rates of discrimination in health care settings and associated barriers to care (Lett et al., 2022).
In Minnesota, state-level policies make this type of measurement possible. Historically, Minnesota has strong anti-discrimination laws in place to protect gender-diverse individuals. For example, Minnesota was one of the first states to allow an “X” option for gender on licenses (Walsh, 2018). Yet, we found alarmingly high reports of gender-based discrimination in health care among gender minorities in this state. The level of gender-based discrimination may be even higher in other states with less inclusive policies. Consequently, our results suggest that on a national level, gender-based discrimination in health care may affect a substantial number of Americans.
Understanding the full scope of gender-based discrimination in Minnesota and across the U.S. should be a priority in future research to support health equity. Our data contributes to the base of knowledge regarding gender-based discrimination in health care and its correlation with issues of health care access. Our findings highlight the need for more expansive research and policy changes in these areas.
Methods
Data are from the 2021 Minnesota Health Access (MNHA) survey, which is a biennial population-based survey on health insurance coverage and access conducted in collaboration with the Minnesota Department of Health. We limited the analysis to adults responding for themselves about experiences of discrimination and access (n=10,003); we excluded proxy reports (e.g., a household member answering for a spouse or roommate). Tests for statistical significance were conducted at the 95% confidence level.
Check out our companion blog "Examining Discrimination and Health Care Access by Sexual Orientation in Minnesota".
References
Gonzales, G., & Henning-Smith, C. (2017). Barriers to Care Among Transgender and Gender Nonconforming Adults. The Milbank quarterly, 95(4), 726–748. https://doi.org/10.1111/1468-0009.12297
Kachen, A., & Pharr, J. R. (2020). Health Care Access and Utilization by Transgender Populations: A United States Transgender Survey Study. Transgender health, 5(3), 141–148. https://doi.org/10.1089/trgh.2020.0017
Kattari, S. K., & Hasche, L. (2016). Differences Across Age Groups in Transgender and Gender Non-Conforming People's Experiences of Health Care Discrimination, Harassment, and Victimization. Journal of aging and health, 28(2), 285–306. https://doi.org/10.1177/0898264315590228
Lett E., Asabor E., Beltrán S., Cannon A.M., Arah O.A. (2022). Conceptualizing, Contextualizing, and Operationalizing Race in Quantitative Health Sciences Research. Ann Fam Med 20(2):157-163. https://doi.org/10.1370/afm.2792
Movement Advancement Project. "Equality Maps: Housing Nondiscrimination Laws." https://www.lgbtmap.org/equality-maps/non_discrimination_laws/housing. Accessed 11/07/2022.
Reisner, S. L., Bailey, Z., & Sevelius, J. (2014). Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the US. Women & health, 54(8), 750-767.
Shires, D. A., & Jaffee, K. (2015). Factors associated with health care discrimination experiences among a national sample of female-to-male transgender individuals. Health & social work, 40(2), 134–141. https://doi.org/10.1093/hsw/hlv025
Walsh, P. (2018, October 3). Minnesota Now Offers 'X' for Gender Option on Driver's Licenses. Star Tribune. Retrieved November 9, 2022, from https://www.startribune.com/minnesota-now-offers-x-for-gender-option-on-driver-s-licenses/494909961/.
Blog & News
SHADAC in AJPH: Insurance-Based Discrimination Reports and Access to Care Among Non-Elderly U.S. Adults, 2011-2019
December 8, 2022:This journal article was originally published in the American Journal of Public Health (AJPH).
Authors: Kathleen Thiede Call, PhD, Giovann Alarcon-Espinoza, PhD, MPP, Natalie Schwer Mac Arthur, PhD, MAc, and Rhonda Jones-Webb, DrPH
SHADAC researchers and external co-authors recently published an article in the American Journal of Public Health (AJPH) that examines rates of insurance-based discrimination for nonelderly adults with private, public, or no insurance between 2011 and 2019, a period marked by passage and implementation of the Affordable Care Act (ACA) and threats to it.
Using 2011–2019 data from the biennial Minnesota Health Access Survey, the study found that about 4,000 adults aged 18 to 64 report insurance-based discrimination experiences. Using logistic regressions, the authors examined associations between insurance-based discrimination and (1) sociodemographic factors and (2) indicators of access.
Key Findings
- On average, approximately 10% of nonelderly adults reported insurance-based discrimination, although there was a statistically significant increase from 7.7% in 2015 to 11.0% in 2017.
- Reports of insurance-based discrimination remained remarkably stable within each coverage type between 2011 and 2019:
- Uninsured adults ranged between 24.7% to 28.1%
- Adults with public coverage ranged between 18.4% to 24.0%
- Adults with private coverage ranged between 3.0% to 5.4%
- Compared with adults with private insurance (4% on average), insurance-based discrimination was 5 or 6 times higher for adults with public insurance (21% on average) and about 7 times higher for adults with no insurance (27% on average).
- There was little association between insurance-based discrimination and having a usual source of care. However, insurance-based discrimination persistently interfered with confidence in getting needed care and reports of forgone care.
These findings indicate that policy changes from 2011 to 2019 affected access to health insurance, but high rates of insurance-based discrimination among adults with public insurance or no insurance were impervious to such changes. Stable rates of insurance-based discrimination during a time of increased access to health insurance via the ACA suggest deeper structural roots of healthcare inequities.
Read the full American Journal of Public Health article to learn more about the study methods and findings. A copy of this AJPH article is also available upon request.
Publication
Collection of Race, Ethnicity, Language Data on Medicaid Applications: New and Updated Information on Medicaid Data Collection Practices in the States, Territories, and D.C.
 Collecting and monitoring data on Medicaid enrollees that is broken down by race, ethnicity, and language (REL) is an essential first step in assessing health disparities as well as identifying strategies for improvement in state Medicaid programs. Although all state Medicaid agencies and most U.S. territories collect self-reported data on REL from applicants during the eligibility and enrollment process, many states continue to face longstanding and persistent challenges in collecting complete, accurate, and granular data on REL.
Collecting and monitoring data on Medicaid enrollees that is broken down by race, ethnicity, and language (REL) is an essential first step in assessing health disparities as well as identifying strategies for improvement in state Medicaid programs. Although all state Medicaid agencies and most U.S. territories collect self-reported data on REL from applicants during the eligibility and enrollment process, many states continue to face longstanding and persistent challenges in collecting complete, accurate, and granular data on REL.
In this issue brief prepared for State Health and Value Strategies with funding from the Robert Wood Johnson Foundation, SHADAC researchers Emily Zylla, Elizabeth Lukanen, and Hannah Geressu provide an overview of federal REL data collection standards, and examine Medicaid application questions, answer options, and instructional language used by Medicaid programs in all 50 states, the District of Columbia, and five U.S. territories. This serves as an update to SHADAC’s previous brief, providing up-to-date information on Medicaid REL data collection among the states and extending the analysis to include the District of Columbia and the five territories.
Access the full brief for more information on state-level Medicaid REL data collection.
Related Reading
Previous version: Collection of Race, Ethnicity, Language (REL) Data in Medicaid Applications: A 50-state Review of the Current Landscape
SHVS Brief: Collection of Sexual Orientation and Gender Identity (SOGI) Data: Considerations for Medicaid and Spotlight on Oregon (Update forthcoming)
SHVS Expert Perspective: Exploring Strategies to Fill Gaps in Medicaid Race, Ethnicity, and Language Data
Publication
Better Health through Data: Improved Collection of Demographic Data in Medicaid
SHADAC Deputy Director Elizabeth Lukanen served as an expert panelist for an Alliance for Health Policy briefing hosted by Arnold Ventures titled "Better Health through Data: Opportunities and Limitations of Health Data" which was held virtually on October 6, 2022. This event reviewed the importance and use of health data in addressing health disparities, the main barriers that persist in limitations to health data, and policy levers that can improve health data collection and utilization at the federal level including changes to data standards and systems, incentives and requirements, education and technical assistance, and regulation.
Elizabeth's presentation specifically focused on Medicaid Administrative Data and how SHADAC has been working to evaluate activities aimed at improving response rates and enhancing the quality of these data at the state level. She also highlights efforts by a few states – Oregon, New York, and Maryland – that have done a lot of work to fill gaps in their demographic data collection of Medicaid enrollees.
Visit the Alliance for Health Policy event page for further details, resources provided by the panelists, and a recording of this event.
Related resources supported by State Health and Value Strategies (SHVS):
- Issue Brief - Collection of Race, Ethnicity, Language (REL) Data in Medicaid Applications: A 50-state Review of the Current Landscape
- Issue Brief - Collection of Sexual Orientation and Gender Identity (SOGI) Data: Considerations for Medicaid and Spotlight on Oregon
- Expert Perspective - Exploring Strategies to Fill Gaps in Medicaid Race, Ethnicity, and Language Data
- Expert Perspective - New York State of Health Pilot Yields Increased Race and Ethnicity Question Response Rates
Publication
Overview of SHADAC's Minnesota Community and Uninsured Profile for MDH's Health Equity Data Community of Practice
On September 19, 2022, SHADAC investigator Kathleen Thiede Call presented at the Minnesota Department of Health's Health Equity Data Community of Practice Meeting. This presentation included a guided tour of SHADAC's Minnesota Community and Uninsured Profile, along with a brief history of how this resource was created. Click the image below to download the slide deck from this presentation.