Blog & News
Charting Two Decades of the Evolving Opioid Crisis
November 18, 2022:
In more than 20 years, the overdose crisis has shifted and grown from prescription opioids to a range of illicitly trafficked drugs |
Just over a decade after the U.S. Centers for Disease Control and Prevention (CDC) declared an “epidemic” of overdoses from prescription painkillers in 2011, the opioid crisis is worse than ever—yet it only vaguely resembles those earlier days. While people are still dying of overdoses tied to prescription opioids, the problem has largely shifted to illicitly trafficked opioids, such as fentanyl, and is now deeply intertwined with other non-opioid substances, such as methamphetamine and cocaine.
This blog examines the history and evolution of the opioid crisis through several charts based on data from SHADAC’s State Health Compare.
Changing attitudes in opioid prescribing
Today, it is broadly accepted that the over-prescribing of opioid painkillers—such as the blockbuster drug Oxycontin (a brand-name version of oxycodone produced by Purdue Pharma) and related semi-synthetic opioid hydrocodone—sparked what became an epidemic of overdoses and deaths. Over more than 10 years, deaths from overdoses involving those medications gradually crept upward until they finally capture widespread attention. When the toll of overdose deaths from prescription opioids was fully recognized and the U.S. healthcare system started to grapple with the problem, efforts to curb prescribing began.
In the first chart, data from the U.S. Drug Enforcement Agency show how legal sales of oxycodone and hydrocodone began the early days of the crisis at about 5 kilograms per 100,000 people in 2000. But within a decade, oxycodone sales roughly quadrupled and hydrocodone sales almost tripled (Figure 1). Following growing awareness of the problem, legal sales of both drugs—driven by prescriptions written by healthcare providers—have declined substantially. In 2021, hydrocodone sales had fallen to about 5 kilograms per 100,000 people, and oxycodone sales to less than 10 kilograms per 100,000 people.
Figure 1: Prescription opioid painkiller sales, 2000-2021
Source: SHADAC analysis of U.S. Drug Enforcement Agency's Automated Reports and Consolidated Ordering System (ARCOS) Retail Drug Summary Reports, obtained from statehealthcompare.shadac.org.
These data demonstrate that legal sales of prescription opioid painkillers are down dramatically from their heights when the CDC first rang alarm bells over the issue. However, some experts and advocates argue that the abrupt pivot in opioid prescribing practices was not done carefully enough, with many people who were already addicted to opioids suddenly cut off without sufficient screening for addiction or access to treatment. And data show that although deaths from prescription opioids have essentially plateaued since prescribing of opioid painkillers dropped, opioid overdose deaths have still continued to climb.
Persistently growing rates of opioid overdose deaths
Because overdose deaths were driven largely by prescription opioid painkillers in the early days of the epidemic, the hope and expectation was that death rates would drop as healthcare providers curtailed their prescribing of the risky medications. But this next set of charts shows that this hope was not fully realized.
In fact, the enhanced scrutiny on opioid prescribing and declining sales of prescription opioid painkillers appears to have marked a turning point in the epidemic. While deaths from prescription opioid painkillers have not declined dramatically, their growth trend leveled off and has remained relatively steady, around 4 deaths per 100,000 people, for almost a decade (Figure 2).
Figure 2: Prescription opioid painkiller death rates, 1999-2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
But to the shock and horror of many, overall overdose death rates—including prescription opioid painkillers as well as all other kinds of opioids—only continued to accelerate.
Figure 3: Death rates from all opioid types, 1999-2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
In less than a decade, the overdose death rate from all opioids roughly tripled, from 7.3 deaths per 100,000 people in 2011 to 21.4 deaths per 100,000 people in 2020 (Figure 3). But this time, the growth came from different types of opioids. First came heroin—an opioid that is without legal medical uses in the U.S. and is only available through the illicit drug trade. This was followed by fentanyl (and other closely related synthetic opioids), which does have legal medical uses but has been adopted by traffickers as a new drug of choice.
Figure 4: Death rates from fentanyl and other synthetic opioids, 1999-2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
In just a few years, the opioid crisis had transformed. What began as a problem rooted in widespread availability of prescription opioid painkillers shifted to illicitly trafficked opioids as legal opioid sales started to fall. By 2020, heroin overdose death rates had more than tripled since the CDC declared an opioid epidemic. And overdose death rates from fentanyl and similar synthetic opioids had grown more than 20 times (Figure 4).
In some ways, those developments may not be surprising. Economics tells us that when a good becomes scarce—such as prescription opioids after recognition of the crisis—people tend to cut back their consumption. But when people can’t simply stop their consumption, as in the case of addiction, they often turn to substitutes. With opioids, that unfortunately left many people to seek out substances such as heroin on the illicit market, where the purity and potency is unreliable, making them even riskier than prescription opioids. And once drug traffickers embraced the potent opioid fentanyl, it pervaded the illegal drug trade and became entangled with non-opioid substances, such as cocaine and methamphetamine.
A metastatic phase of the crisis
The opioid crisis is complex, and definitive evidence of how the epidemic evolved is hard to find. That is particularly the case in understanding the role of the illicit drug trade. However, it is widely accepted that some people shifted to heroin as prescription opioid painkillers became harder to obtain. Afterward, drug traffickers incorporated fentanyl into their supplies, sometimes to cheaply boost the potency of their heroin or simply to pass fentanyl off as heroin. Another approach was manufacturing counterfeit prescription medications, such as fake Oxycontin pills that actually contained fentanyl rather than the less-potent opioid oxycodone.
Over time, fentanyl became ubiquitous in the U.S. illicit drug market. Non-opioid illicitly trafficked substances, particularly cocaine and methamphetamine, are now often contaminated with fentanyl and related powerful opioids. And various kinds of illicitly trafficked counterfeit medications are found to contain fentanyl. In some cases, those counterfeit pills may mimic prescription opioid painkillers, but other counterfeit pills may contain fentanyl, even if the legitimate version does not. For instance, law enforcement agencies have reported interdicting fake stimulants (e.g., Ritalin and Adderall pills) that are mixtures of methamphetamine and fentanyl, even though the genuine medications do not contain opioids.
Ultimately, the pernicious impact of fentanyl and related synthetic opioids have transformed the opioid crisis. The prescription opioid painkillers that sparked this epidemic now only account for a fraction of drug overdose deaths in the U.S. (Figure 5), dwarfed by the toll of synthetic opioids such as fentanyl. And largely because of the pervasiveness of fentanyl in the market for illicit substances, deaths involving non-opioids also have grown to historic levels.
Figure 5: National Death rates for opioid and non-opioid substances, 2020
Source: SHADAC analysis of National Center for Health Statistics mortality files, obtained from statehealthcompare.shadac.org.
Lessons from opioids data
More than two decades into the opioid crisis, the main consistency is that the problem is continually evolving. When the role of prescription opioids in overdose deaths led the health care system to curtail dangerously generous prescribing of those medications, some people seemingly transitioned to illicitly trafficked opioids. When drug traffickers saw an opportunity to enhance their profits on heroin sales by using fentanyl and by manufacturing counterfeit pills, the epidemic became even deadlier. And as fentanyl became more pervasive, it also became intertwined with non-opioid substances, such as cocaine and methamphetamine—further extending the deadly reach of opioids.
To better understand and address the opioid crisis, it is important to use data to identify evolving patterns and trends and to anticipate new developments before they snowball into larger public health threats. Examining the history of the opioid crisis may prove useful to avoid recurrences of similar situations in the future, but it is also important to recognize the limitations of retrospective data for designing solutions to a dynamic situation. For instance, an overemphasis on prescribing of opioid painkillers now, when the vast majority of drug overdose deaths are caused by illicitly trafficked substances, could be considered akin to driving down a busy interstate highway while fixed on the rearview mirror.
Related Reading:
Blog: 2020 U.S. alcohol-involved deaths climbed by 26.6%, and drug overdose deaths by 30.6%
Resource Page: The Opioid Epidemic in the United States
Blog & News
Five-Year Review Shows Rising Trends in Adult E-Cigarette Use: 2017 to 2021
November 9, 2022:|
BRFSS OVERVIEW |
|
Though COVID-19 remains a focal point of concern as the official public health emergency (PHE) is extended, public health researchers and workers have slowly begun to resume attentions to other ongoing and emergent public health crises such as the long-running opioid epidemic, increases in alcohol-related behaviors such as binge drinking and heavy drinking, and e-cigarette use and smoking rates, especially among young adults.
The recent ban and removal of all JUUL e-cigarette products by the U.S. Food and Drug Administration (FDA) is one of the biggest moves to address this issue at the federal level. Additionally, as of June 2022, all 50 states, the District of Columbia, and nearly all U.S. territories have enacted legislation banning sales of e-cigarettes to underage individuals (under age 21). These actions at the federal and state level are aimed at curbing an alarming and persistent rise in e-cigarette usage, especially flavored e-cigarettes, among high-school and middle-school-aged children, as shown in a recent study conducted by the FDA and the Centers for Disease Control and Prevention (CDC). However, the issue of rising e-cigarette use is not limited to only teens and young adults.
Significant Increases Across the States
Nationally, the rate of adult e-cigarette use in 2021 was 6.6 percent. Across the states, e-cigarette use among adults in 2021 ranged from a high of 9.4 percent in Oklahoma to a low of 4.5 percent in Maryland.
Rates of E-Cigarette Use Among Adults, Top Five and Bottom Five States, 2021
While these rates may initially seem low, a comparison to a previous SHADAC analysis on e-cigarette use shows that in just five years the overall rate of adults reporting using e-cigarettes has increased significantly by over two percentage points (PP) from 4.4 percent in 2017.
The range of e-cigarette usage reported by adults across the states has experienced similar trends. From 2017 to 2021*, Oklahoma remained the state with the highest rate of adult e-cigarette use, rising significantly to 9.4 percent in 2021 from 7.1 percent in 2017. The state with the lowest rate of adult e-cigarette use shifted from the District of Columbia (D.C.) in 2017, with a rate of just 2.5 percent, to Maryland in 2021, with a rate of 4.5 percent. Again, the difference between the two lowest rates was statistically significant, indicating an overall increase in e-cigarette use by adults during this time period.
Overall, the states ranking in the top and bottom five for e-cigarette use among adults remained largely unchanged from 2017 to 2021. Kentucky, Oklahoma, and Tennessee remained among the states with the highest rates of reported adult e-cigarette use, with Alabama and Louisiana in 2021 replacing Indiana and Wyoming. Connecticut, Maryland, Vermont, and D.C. remained among the states with the lowest rates of reported e-cigarette use from 2017 to 2021, with New Hampshire in 2021 replacing California.
E-Cigarette Use by Age Group
Most efforts toward curbing rising e-cigarette use have been aimed at teen and young adult age groups, and as the figure below shows, it is easy to see why.
While rates of e-cigarette usage rose across all age groups over the past five years, the highest increases were seen among younger adults age 18-24 and 25-34.
Adult E-Cigarette Use by Age Group from 2017 to 2021
The rate of e-cigarette use among adults age 18-24 nearly doubled, rising by over 8 percentage points from 10.1 percent in 2017 to 18.5 percent in 2021, a statistically significant difference. Similarly, the rates for adults age 25-34 increased significantly from 6.6 percent in 2017 to 11.1 percent in 2021. In fact, all age groups except adults age 45-64 saw significant increases in the rate of e-cigarette use from 2017 to 2021.
Conclusion
In 2019, the CDC began tracking the number of lung injuries and related deaths associated with vaping and e-cigarette use. By early 2020, they revealed that all 50 states, D.C., and several territories were submitting pertinent data to CDC and that the number of lung injuries across the nation had been recorded at 2,807 with deaths recorded at 68. According to recent research from Johns Hopkins University, many of these deaths have not come from regulated market products, but from black market modifications to devices or to vaping liquids—mirroring concerns about current trends in the opioid crisis, which has shifted from prescription (i.e., regulated market) opioid painkillers to unregulated fentanyl that traffickers mix into drugs, leaving consumers unaware of the exact makeup or potency of the product they are purchasing.
While the true effectiveness of state legislations and the FDA ban on e-cigarette products will be revealed with time, they are solid steps towards curbing rising rates of e-cigarette use across a number of age groups in the U.S.
Source: SHADAC Analysis of 2017-2021 Behavioral Risk Factor Surveillance System (BRFSS) public use files.
Notes: * 2019 data is not available. Statistically significant changes at the 95% confidence level unless otherwise noted.
Publication
Prevalence and disparities in excessive alcohol use among U.S. adults
 17 million report heavy drinking,
17 million report heavy drinking,
40 million report binge drinking
In the past several years, researchers have shone new light on the public health threat of alcohol consumption in the United States. Nationally, life expectancy has declined, while deaths involving drugs and alcohol have increased.i Those findings are reinforced by studies finding increased high-risk alcohol consumption, such as binge drinking and heavy drinking.ii And early evidence indicates that the COVID-19 pandemic has only accelerated Americans’ alcohol consumption and risky drinking behaviors.iii
The health toll of excessive alcohol consumption affects nearly every segment of the U.S. adult population, as shown by statistically significant growth in alcohol-involved deaths in almost every state and demographic subgroup in a recent SHADAC analysis.iv However, alcohol-involved deaths have not affected the population evenly, with some states and some demographic subgroups experiencing much higher death rates than others.
The analysis in this new brief from SHADAC expert Colin Planalp focuses on high-risk alcohol consumption behaviors that can lead to death and other alcohol-involved diseases. Similar to alcohol-involved deaths, significant differences were found among demographic subgroups in the prevalence of binge drinking and heavy drinking.
Download a PDF of SHADAC's "Prevalence and disparities in excessive alcohol use among U.S. adults" brief.
Related Reading
Size of alcohol, drug overdose death increases in first pandemic year were unparalleled (Blog)
U.S. Health on the Rocks: The Quiet Threat of Growing Alcohol Deaths (Webinar)
Pandemic drinking may exacerbate upward-trending alcohol deaths (Blog)
Escalating Alcohol-Involved Death Rates: Trends and Variation across the Nation and in the States from 2006 to 2019 (Brief and Infographics)
i Case, A. & Deaton, A. (2015, December 8). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. PNAS, 112(49), 15078-15083. https://www.pnas.org/content/112/49/15078
ii Dafna, D., Naimi, T.S., Liu, Y., & Brewer, R. (2020, January 17). Trends in total binge drinks per adult who reported binge drinking—United States, 2011-2017. MMWR Weekly, 69(2), 30-34. https://www.cdc.gov/mmwr/volumes/69/wr/mm6902a2.htm?s_cid=mm6902a2_w#F1_down
iii Grossman, E.R., Benjamin-Neelon, S.E., & Sonnenschein, S. (2020). Alcohol consumption during the COVID-19 pandemic: A cross-sectional survey of US adults. Int J Environ Res, 17(24), 9189. https://www.mdpi.com/1660-4601/17/24/9189
iv Planalp, C., Au-Yeung, C.M., & Winkelman, T.N.A. (2021). Escalating alcohol-involved death rates: Trends and variation across the nation and in the states from 2006 to 2019. State Health Access Data Assistance Center (SHADAC). https://www.shadac.org/sites/default/files/publications/Alcohol-Involved-Deaths/AID-4.21-SHADAC-Brief.pdf
Blog & News
Pandemic drinking may exacerbate upward-trending alcohol deaths
June 14, 2021:Even before 2020, alcohol-involved deaths reached a modern record
Considering the well-deserved attention paid to the opioid crisis in recent years, few people might guess that rates of alcohol-involved deaths were as high as or higher than opioid overdose death rates in nearly half of states (Figure 1).1 Like the opioid crisis, the trend in alcohol-involved deaths is also worsening, having grown by roughly 50 percent in just over a decade. All this was before the coronavirus crisis had even begun.
Figure 1. State alcohol death rates vs. opioid death rates, 2019
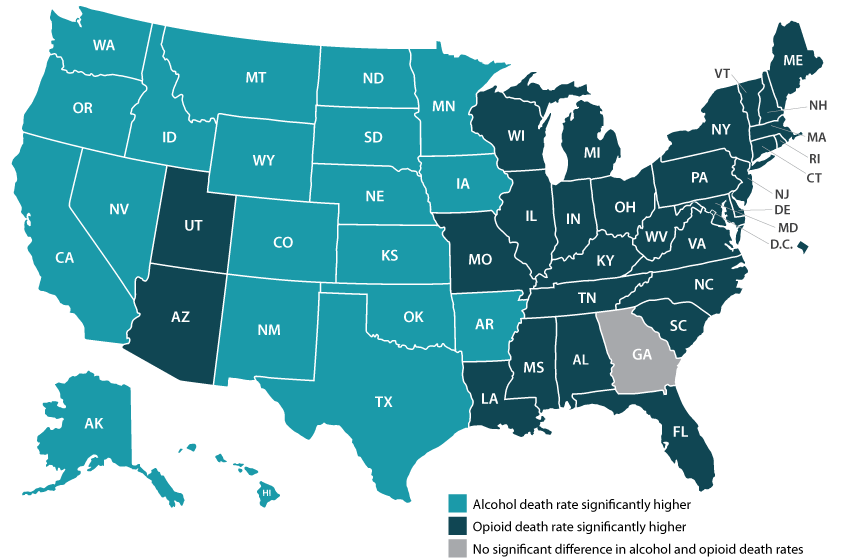
|
Data and analysis on alcohol-involved deaths Read more about growing alcohol-involved death |
Now, evidence is accumulating that the pandemic precipitated dangerous changes in the way people consume alcohol in the United States. For instance, research has found increased alcohol sales since the crisis began, a finding illustrated by data showing that liquor taxes represented a rare instance of increased revenues for some states, such as Minnesota, during the COVID pandemic.2,3 Other studies have found that U.S. adults report consuming more alcohol in order to deal with pandemic-related stress, and that they are drinking more frequently and engaging in more high-risk drinking behaviors, such as heavy drinking and binge drinking.4,5,6
As we climb our way out of the immediate crisis, the U.S. will need to shift attention back to long-running public health threats. Beyond the obvious toll of the virus itself, another legacy of the pandemic may be the exacerbation of existing problems, including alcohol-related deaths and the opioid crisis. The opioid crisis was commonly recognized before 2020, but the upward trend in alcohol deaths was still occurring largely under the radar (Figure 2). But recent attention to risky pandemic-related alcohol consumption can sharpen our focus on this emerging concern.
Figure 2. U.S. alcohol-involved death rates, 2000-2019
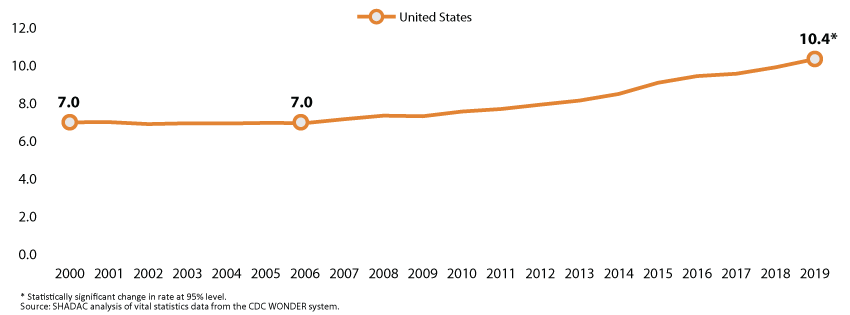
With alcohol especially, the U.S. has a window of opportunity to intervene before many people’s pandemic-era risky drinking habits result in deaths, since the bulk of alcohol-involved deaths result from years of excessive drinking. In the coming years, it will be vital for states to monitor and study these issues and to consider doubling down on policy initiatives to curb the tide through efforts such as enhancing access to treatment of substance use disorder and by persuading and assisting people in recalibrating their alcohol consumption to healthier levels.
Visit State Health Compare to explore state-level data on alcohol death and opioid death rates.
1 SHADAC Staff. U.S. alcohol-related deaths grew nearly 50% in two decades: SHADAC briefs examine the number among subgroups and states. https://www.shadac.org/news/us-alcohol-related-deaths-grew-nearly-50-two-decades. Published April 19, 2021. Accessed May 12, 2021.
2 Rebalancing the ‘COVID-19 effect’ on alcohol sales. Nielseniq.com. https://nielseniq.com/global/en/insights/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/. Published May 7, 2020. Accessed May 12, 2021.
3 Ewoldt J. Liquor stores neared sales records for 2020 as bars, restaurants closed. Startribune.com. https://www.startribune.com/liquor-stores-neared-sales-records-for-2020-as-bars-restaurants-closed/573469221/. Published December 26, 2020. Accessed May, 12, 2021.
4 American Psychological Association. Stress in America: One year later, a new wave of pandemic health concerns. https://www.apa.org/news/press/releases/stress/2021/sia-pandemic-report.pdf. Published March 2021. Accessed May 12, 2021.
5 Pollard MS, Tucker JS, Green HD. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020; 3(9): e2022942. doi: 10.1001/jamanetworkopen.2020.22942.
6 Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health. 2020;17(24): 9189. doi: 10.3390/ijerph17249189
SHADAC Expertise
Population Health
Population health research focuses on the health outcomes, health determinants, and policies and programs that affect a specific group of individuals, or “population.” SHADAC researchers often conduct population health research by geographic levels, most often for states, but also offer technical assistance to state researchers and policy analysts who might be interested in looking at population health by county or city. Other examples of SHADAC’s population health expertise focus around studies of health disparities for a particular measure based on race or ethnicity, income level, or education level and assessments of state health information exchange policies.
Related SHADAC work
Click on any title below to learn more about the project.
Prevalence and disparities in excessive alcohol use among U.S. adults
In the past several years, researchers have shone new light on the public health threat of alcohol consumption in the United States. Nationally, life expectancy has declined, while deaths involving drugs and alcohol have increased. Those findings are reinforced by studies finding increased high-risk alcohol consumption, such as binge drinking and heavy drinking. And early evidence indicates that the COVID-19 pandemic has only accelerated Americans’ alcohol consumption and risky drinking behaviors. This report focuses on high-risk alcohol consumption behaviors that can lead to death and other alcohol-involved diseases. Similar to alcohol-involved deaths, significant differences were found among demographic subgroups in the prevalence of binge drinking and heavy drinking.
Rates of Anxiety and Depression Symptoms Declined in 2021, Remained Higher than Pre-Pandemic
This brief examines both combined and individual rates of reported anxiety and depression symptoms for the total adult population as well as by specific breakdowns, including age, gender, race/ethnicity, income categories, and education levels. Findings discussed in this brief can help public health officials and policymakers identify the need for intervention and outreach targeted at populations that have been especially affected by the mental health burdens of the pandemic.
Exploring 2021 State Public Health Funding Estimates Using State Health Compare
Tracking data on state public health funding can help identify which states are well-positioned to absorb potential decreases in federal funding (assuming no recourse to additional state-level funding) and improve efforts to distribute scarce public health resources most effectively nationwide. This updated SHADAC brief on state-provided public health funding estimates highlights newly-available 2021 data as well as trends over the past decade (2012–2021). These estimates come from SHADAC’s State Health Compare measure, “Public Health Funding”, which provides annual estimates of per-capita state public health funding starting in 2005 (with the exception of data year 2006, for which no estimates are available).
The Opioid Crisis in the Pandemic Era
During 2020 and 2021, the first two years of the COVID-19 pandemic, data show that drug overdose deaths did not subside or plateau, but unfortunately surged alongside the rise of the coronavirus. Growing death rates were driven by a substantive change in the very foundation of the opioid crisis, transforming it from a public health threat caused by prescription painkillers to one in which overdose deaths are predominantly due to three different substances: methamphetamine, cocaine, and, most concerningly, fentanyl. In their newest opioid brief, SHADAC researchers examine this latest shift in the long-standing crisis of opioid use in the United States. Read the brief in full here for more detailed findings, and explore the data by topic on SHADAC's State Health Compare.
Past Work
Charting Two Decades of the Evolving Opioid Crisis
Just over a decade after the U.S. Centers for Disease Control and Prevention (CDC) declared an “epidemic” of overdoses from prescription painkillers in 2011, the opioid crisis is worse than ever—yet it only vaguely resembles those earlier days. While people are still dying of overdoses tied to prescription opioids, the problem has largely shifted to illicitly trafficked opioids, such as fentanyl, and is now deeply intertwined with other non-opioid substances, such as methamphetamine and cocaine. This blog examines the history and evolution of the opioid crisis through several charts based on data from SHADAC’s State Health Compare.
Internet Access Measures the Impact of the Digital Divide and COVID-19
 Lack of equitable access to broadband internet services across all households has been an issue of concern among health care experts even prior to the coronavirus pandemic. Initially, the problem of digital divide was studied in terms of barriers to health plan application and enrollment during the rollout of the newly developed online health insurance marketplace. In light of the coronavirus pandemic, lack of access to broadband internet services has also emerged as a potential challenge to efforts to respond to the coronavirus; not only in preventing individuals from accessing the real-time information they need surrounding COVID-19, but also in lost chances for utilization of telehealth services, ability to work remotely, keeping pace with an e-learning curriculum, or to help mitigate the dangers of social isolation while practicing social distancing. SHADAC researchers explore the variation in access to broadband internet across states, and reveal disparities by income, rurality, coverage, and disability status.
Lack of equitable access to broadband internet services across all households has been an issue of concern among health care experts even prior to the coronavirus pandemic. Initially, the problem of digital divide was studied in terms of barriers to health plan application and enrollment during the rollout of the newly developed online health insurance marketplace. In light of the coronavirus pandemic, lack of access to broadband internet services has also emerged as a potential challenge to efforts to respond to the coronavirus; not only in preventing individuals from accessing the real-time information they need surrounding COVID-19, but also in lost chances for utilization of telehealth services, ability to work remotely, keeping pace with an e-learning curriculum, or to help mitigate the dangers of social isolation while practicing social distancing. SHADAC researchers explore the variation in access to broadband internet across states, and reveal disparities by income, rurality, coverage, and disability status.
Pages
- « first
- ‹ previous
- 1
- 2
- 3












