Blog & News
State Health Compare Data Highlight: Potentially Preventable Hospitalizations
May 29, 2019:More expensive than outpatient or primary care, hospitalization contributes substantially to healthcare costs, with hospital care accounting for 33% of healthcare spending, or $1.1 trillion, in 2017.[1] Reducing potentially preventable hospitalizations—i.e., hospital admissions for certain acute illnesses or chronic conditions that might not have required hospitalization if they had been better managed through outpatient primary care—is therefore a key mechanism by which healthcare costs can be reduced. National and state-level data on potentially preventable hospitalizations allow policymakers and analysts to track and monitor trends in this area, assess progress or setbacks, and consider policy levers that could effect change.
State Health Compare: A Unique Source of State-Level Estimates on Potentially Preventable Hospitalizations
SHADAC’s State Health Compare is the only publicly accessible source of state-level measures on potentially preventable hospitalizations, with three measures available: 1) per person cost of potentially preventable hospitalizations; 2) rates of potentially preventable adult hospitalizations; and 3) rates of potentially preventable child hospitalizations. These measures are available for 2009 through 2015 (the most recent year available).
About the Data
State Health Compare uses data from the Health Care Cost and Utilization Project (HCUP) to produce the above measures.[2] HCUP is a collection of national and state inpatient and emergency department databases that constitutes the largest available all-payer longitudinal hospital care data source. HCUP data are derived from hospital administrative discharge records originally used for hospital billing procedures.[3] State Health Compare’s national estimates were calculated using HCUP’s Nationwide Inpatient Sample (NIS), and state-specific results were calculated using HCUP’s State Inpatient Databases (SID) along with state inpatient databases purchased directly from states.
State Health Compare Highlights from 2015
- In 2015, per person costs of potentially preventable hospitalizations averaged $129 nationwide. Among the states, costs ranged from $70 per person in Colorado to $215 per person in the District of Columbia.
- The national average for potentially preventable hospitalizations per 100,000 adults was 1,520 in 2015, compared to a low of 867 in New Mexico and a high of 2,061 in the District of Columbia.
- The rate of potentially preventable hospitalizations per 100,000 children averaged 131 nationwide in 2015. Among the states, this rate ranged from 46 in Vermont to 260 in the District of Columbia.
Policy Implications
Data on potentially preventable hospitalizations can be used as evidence in support of multiple policy interventions. For example, these data point to the need for policies that would increase preventive service utilization as well as policies that would increase utilization of effective primary care–both strategies that are shown to reduce potentially preventable hospitalizations. [4],[5]
Explore potentially preventable hospitalizations on State Health Compare.
Related Reading
In 2016, SHADAC published a report on using HCUP data for State Health Policy Analysis, available here.
Agency for Healthcare Research and Quality. (2019). HCUP Overview, Healthcare Cost and Utilization Project (HCUP). Available at: https://www.hcup-us.ahrq.gov/overview.jsp
[1] Centers for Medicaid & Medicaid Services (CMS). National Health Expenditures 2017 Highlights [PDF File]. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/downloads/highlights.pdf
[2] SHADAC used the first three quarters of 2015 data for the 2015 estimates because HCUP switched from ICD-9 to ICD-10 coding in the fourth quarter of 2015. The next year of data will continue to use ICD-10 codes. When SHADAC publishes the 2016 HCUP data, we will indicate a break in series.
[3] There are some states where the data are not available (or not supplied to the Health Care Cost and Utilization Project) or for which data are suppressed because of reliability issues.
[4] “Introduction” in The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Yong, P.L., Saunders, R.S., Olsen, L.A., eds. National Academies Press (US), 2010. Available at: https://www.ncbi.nlm.nih.gov/books/NBK53914/
[5] Agency for Healthcare Research and Quality (AHRQ). Chartbook on Care Coordination: Potentially Avoidable Hospitalizations. Content last reviewed June 2018. Available at: https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/carecoordination/measure3.html
Blog & News
Trends and Disparities in Children's Health Insurance: New Data and the Implications for State Policy (Webinar)
April 24, 2019:Date: May 2, 2019
Time: 11:00 a.m - 12:00 p.m. Central
View a recording of the webinar.
 The State Health Access Data Assistance Center (SHADAC) and State Health and Value Strategies (SHVS) are hosting an online discussion to share new data showing a recent uptick in the rate of uninsured children and highlight promising state-level policies that could help.
The State Health Access Data Assistance Center (SHADAC) and State Health and Value Strategies (SHVS) are hosting an online discussion to share new data showing a recent uptick in the rate of uninsured children and highlight promising state-level policies that could help.
The interactive webinar will feature experts Lynn Blewett, PhD, and Elizabeth Lukanen, MPH, from SHADAC and Heather Howard, JD, from SHVS, and will offer state-based policymakers a forum to learn from and share insight with each other.
With key findings from a new SHADAC report–including state-specific data broken down by race, income, and coverage type–the conversation will cover implications for policymakers, novel approaches states have put in place to ensure more children have access to care, and more.
SHADAC and SHVS will answer questions from attendees after the presentation.
Related Resources
Children's Health Insurance Coverage Nationwide and in the States, 2016-2017
Blog & News
SHADAC Releases 50-State Analysis of the Evolving Opioid Crisis (Infographics)
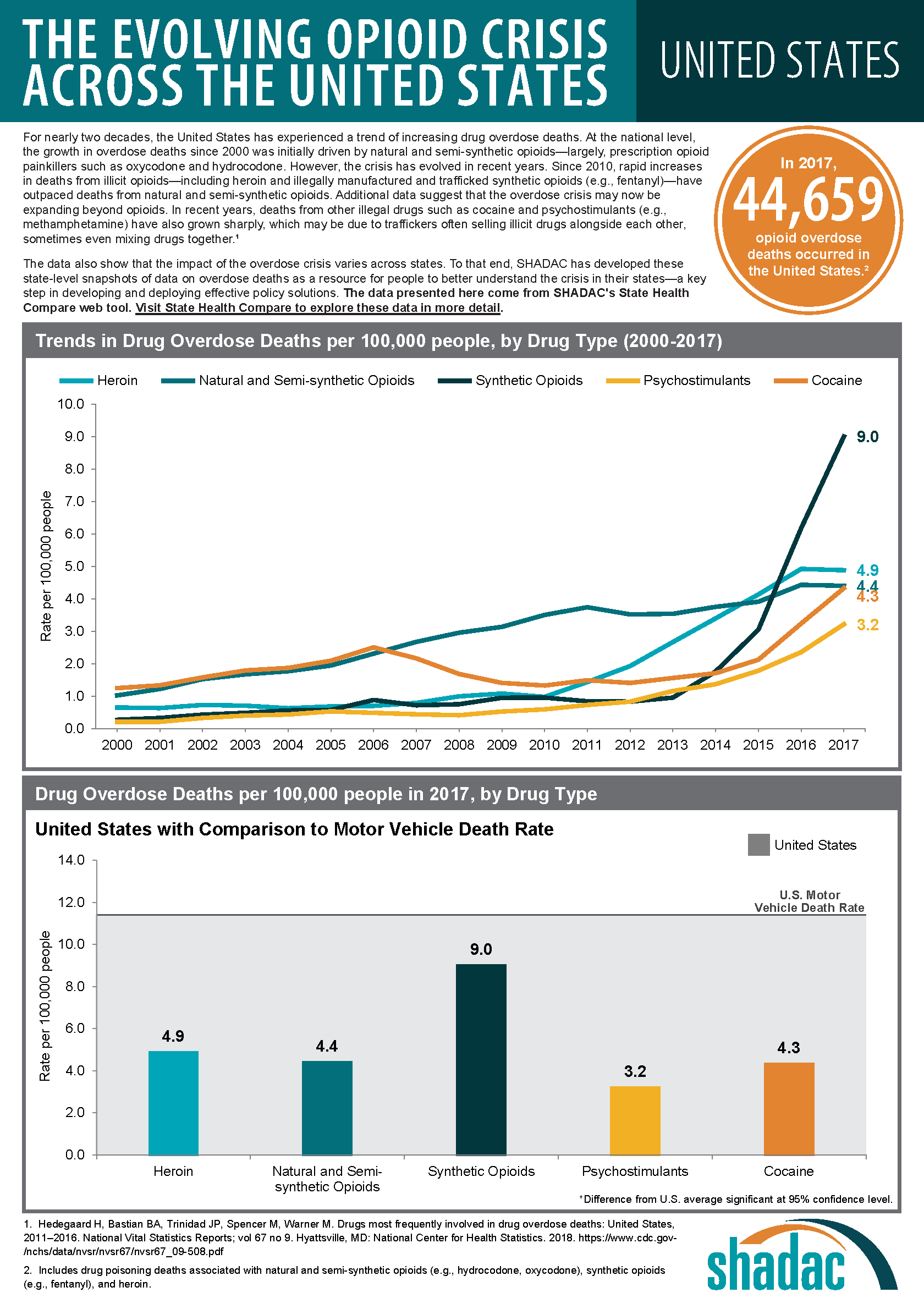
February 11, 2019:Much of the attention paid to the national opioid crisis in recent years has focused on the national toll of the crisis, such as the more than 44,000 opioid overdose deaths reported nationally in 2017.[1] However, the dynamics of the crisis vary widely across states, both in the prevalence of opioid overdose deaths and the types of opioids associated with those deaths.
To make state-specific information on opioid overdose deaths more easily accessible, SHADAC has used estimates from our State Health Compare online data tool to create a set of two-page infographics for all 50 states and the District of Columbia that include new data on drug overdose deaths for 2017.
Additionally, because of growing concern and evidence that the opioid crisis may be expanding to other non-opioid illicit drugs, we also have included data on drug overdose deaths from two types of drugs that are commonly involved in opioid overdoses: cocaine and psychostimulants (such as methamphetamine). [2],[3]
HIGHLIGHTS
Background: U.S. trends in drug overdose deaths
At the national level, data on opioid overdose deaths show multiple, evolving phases of the overdose epidemic. From 2000 to approximately 2011, the growth in opioid overdose deaths was driven primarily by natural and semi-synthetic opioids (i.e., prescription opioid painkillers); but that death rate has since largely plateaued. Beginning around 2011, deaths from heroin began to increase more rapidly and were responsible for the highest overdose death rates in 2015. Since around 2013, however, deaths from synthetic opioids, such as fentanyl, have grown precipitously, and in 2017 the overdose death rate from synthetic opioids was nearly double the rate for all other drug types.
Around the same time that death rates from heroin and synthetic opioids began to increase, deaths from cocaine and psychostimulants also began to increase. Evidence suggests that this relationship is driven, at least in part, by an increase in deaths that involve multiple drugs. Since 2011, when deaths from heroin began to rise, death rates from cocaine have nearly tripled, from 1.5 per 100,000 people to 4.3 per 100,000 people in 2017; and death rates from psychostimulants have more than quadrupled, from 0.7 per 100,000 people to 3.2 per 100,000 people in 2017.
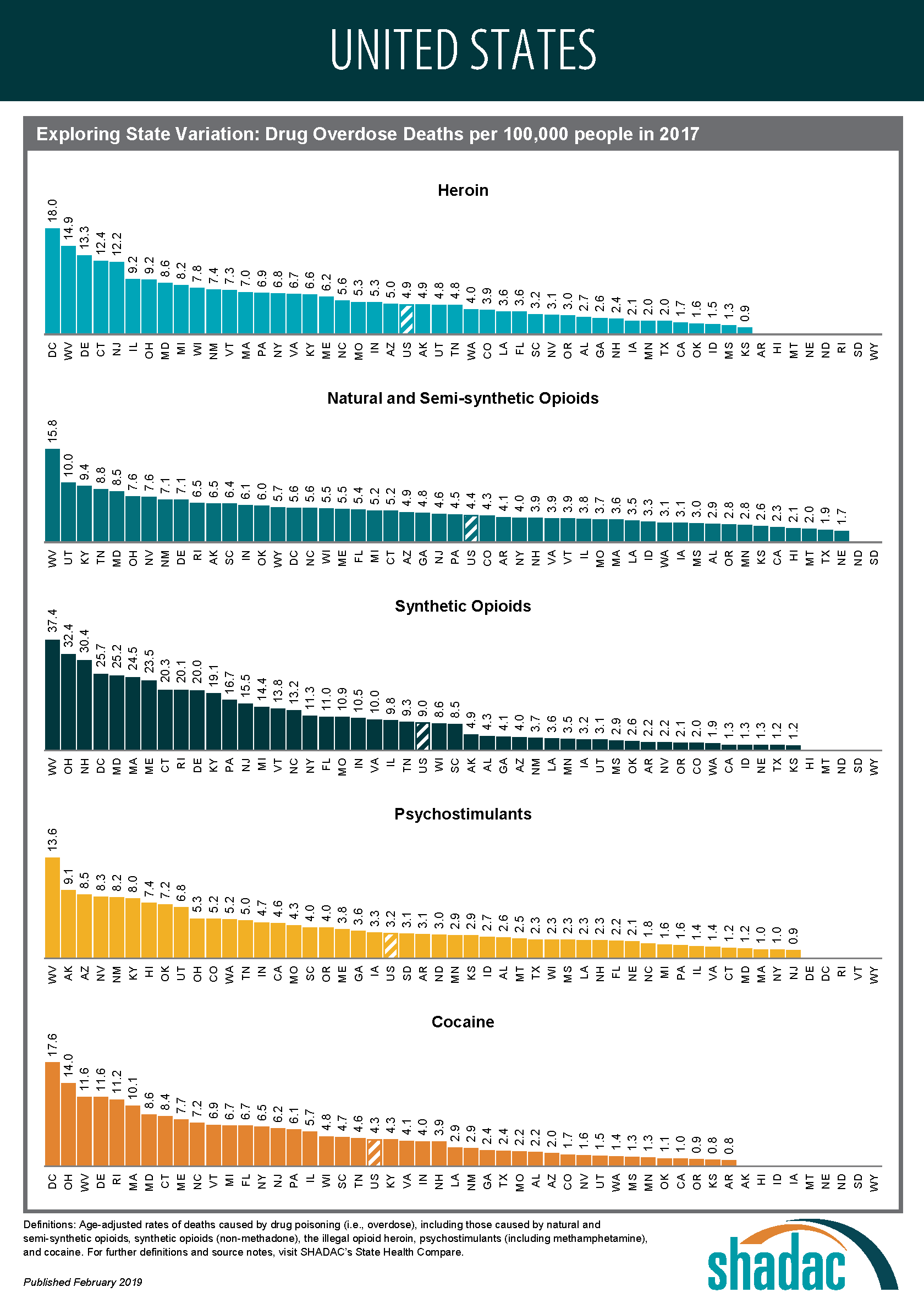
State variation in overdose deaths
Opioid Overdose Deaths
Although most states have experienced measurable increases in opioid overdose deaths since 2000, the scale of the crisis has varied widely across states. For example, West Virginia’s rate of deaths from synthetic opioids in 2017 was more than 30 times the rate of Nebraska and Texas (37.4 deaths versus 1.3 deaths per 100,000 people).
The types of opioids most commonly associated with overdoses also vary across states. For instance, Utah had the second-highest rate of deaths from natural and semi-synthetic opioids in 2017, at 10.0 deaths per 100,000 people; however, contrary to the U.S. trend, the state has experienced relatively little growth in deaths from synthetic opioids, and the state’s 2017 death rate from synthetic opioids (3.1 per 100,000 people), fell well below the U.S. rate of 9.0 per 100,000 people.
Overdose Deaths from Cocaine and Psychostimulants
The scale of overdose deaths from non-opioid illicit drugs also varies widely across states. For example, the 2017 overdose death rate from cocaine in the District of Columbia (17.6 deaths per 100,000 people) was 22 times the rate of Arkansas and Kansas (0.8 deaths per 100,000 people). Similarly, the 2017 overdose death rate from psychostimulants in West Virginia (13.6 deaths per 100,000 people) was more than 15 times the rate of 0.9 deaths per 100,000 people in New Jersey.
Regional Patterns in Drug Overdose Death Rates
Despite the evidence of state variation in drug overdose death rates, further analysis does illustrate some broader patterns:
Heroin and synthetic opioids
Death rates from heroin and synthetic opioids are generally higher east of the Mississippi River, particularly among states in the Northeast, the Appalachian region, and the industrial Midwest.
Natural and semi-synthetic opioids
Higher death rates from natural and semi-synthetic opioids are more geographically dispersed than those from heroin and synthetic opioids. While some states in the eastern U.S. have particularly high rates of deaths from natural and semi-synthetic opioids (e.g., Kentucky, Ohio, and West Virginia), there are other states in the western U.S. that also have similarly high death rates from these drugs (e.g., Utah, New Mexico, and Nevada).
Cocaine
An examination of cocaine death rates reveals a pattern similar to that of death rates from heroin and synthetic opioids, with states east of the Mississippi River exhibiting higher rates of cocaine overdose deaths.
Psychostimulants
Death rate patterns from psychostimulants appear to be almost the opposite of those for heroin and synthetic opioids, with relatively low death rates in the Northeast and particularly high rates of deaths in the western U.S. and the Southeast. Only a group of three state—Kentucky, Ohio, and West Virginia—shows strong overlaps between psychostimulant and heroin and synthetic opioid deaths.
Access the state-level infographics on drug overdose deaths.
Explore the data on drug overdose deaths on State Health Compare.
Further Reading and Resources
New Data on Drug Overdose Death Highlight the Need for State-Level Analysis
SHADAC Blog, December 2018
Exploring the New State-Level Opioid Data on SHADAC’s State Health Compare
SHADAC Webinar (Recording and Presentation Materials), September 2018
The Changing Opioid Epidemic: State Trends, 2000-2016
SHADAC Blog, August 2018
The Changing Opioid Epidemic: National Trends, 2000-2016
SHADAC Blog, July 2018
The Opioid Epidemic: National and State Trends in Opioid-Related Overdose Deaths, 2000-2016
SHADAC Issue Briefs, June 2018
[1] This number includes deaths from natural and semi-synthetic opioids (e.g., prescription opioid painkillers), heroin and synthetic opioids (e.g., fentanyl), but it excludes some opioids with relatively fewer deaths, such as methadone.
[2] Although reports of illicit drugs being tainted with synthetic opioids are relatively common, it is unclear whether deaths involving multiple drugs are typically the result of drugs being intentionally mixed by or unintentionally contaminated through traffickers’ sloppiness, or because individual drug users are concurrently abusing multiple different drugs of their own volition.
[3] U.S. Centers for Disease Control and Prevention. (2018, December 12). Drugs Most Frequently Involved in Drug Overdse Deaths: United States, 2011-2016. National Vital Stastics Report, 67(9), 1-14. Available at: https://www.cdc.gov/nchs/data/nvsr/nvsr67/nvsr67_09-508.pdf
Publication
Exploring Disparities Using New and Updated Measures on SHADAC’s State Health Compare - State-Level Highlights for Unaffordable Rents, Unhealthy Days, and More: Webinar
Date: February 6, 2019
Time: 1:00 p.m. – 2:00 p.m. Central
Click to view the webinar recording below. You can also download the slides as a PDF or download a copy of the event transcript.

On Wednesday, February 6th at 1:00 PM Central, SHADAC hosted a webinar introducing two new measures of health outcomes and social determinants of health on SHADAC’s State Health Compare—Unhealthy Days and Unaffordable Rents. This presentation by SHADAC researchers Brett Fried and Robert Hest examined these new measures and highlight how the estimates can be used to explore disparities between states and among sub-populations.
 The webinar also provided a virtual tour of some of the more than 40 state-level measures currently available on State Health Compare, highlighting recently updated data in particular. Mr. Fried and Mr. Hest demonstrated how users can employ State Health Compare to easily create compelling maps, charts, and graphs, as well as download the raw estimates to perform deeper analyses and statistical testing.
The webinar also provided a virtual tour of some of the more than 40 state-level measures currently available on State Health Compare, highlighting recently updated data in particular. Mr. Fried and Mr. Hest demonstrated how users can employ State Health Compare to easily create compelling maps, charts, and graphs, as well as download the raw estimates to perform deeper analyses and statistical testing.
SHADAC researchers also answered questions from attendees after the presentation.
2019 Measures and Estimates on State Health Compare
Table of Current Measures and Data Sources on State Health Compare
Adult Unhealthy Days: A New Measure on State Health Compare
SHADAC Blog
Housing Affordability Matters: Measuring and Addressing the Burden of Unaffordable Rents
SHADAC Blog
Examining Unaffordable Rents as a Social Determinant of Health
SHADAC Publication - Infographics
Fifty-State Analysis Finds Lower Access to Care among Adults with Less Education
SHADAC Blog
Education Matters: Educational Attainment and Access to Health Care, 50-State Analysis
SHADAC Publication - State Fact Sheets and Infographics
Significance Testing Using State Health Compare
SHADAC Brief
Blog & News
MACStats from MACPAC: 2018 Medicaid and CHIP Data Book Now Available
February 1, 2019:The Medicaid and CHIP Payment and Access Commission (MACPAC) recently released the 2018 version of its Medicaid and CHIP Data Book. This data book is a collection of federal and state statistics regarding the Medicaid and CHIP programs that are compiled by MACPAC from multiple data sources on key topic areas including Medicaid and CHIP eligibility, enrollment, and expenditures, as well as beneficiary health, service use, and access to care. An excellent resource, the data book draws on a wide variety of data sources including Medicaid administrative data (e.g., CMS-64 data, MSIS data, Medicaid Managed Care enrollment reports, etc.) as well as federal survey data in order to compile policy relevant, but difficult to access, information about the Medicaid and CHIP programs into one comprehensive tool.
SHADAC is excited to be among the contractors that contributed to this product, providing MACPAC with estimates from the National Health Insurance Survey (NHIS) and the Medical Expenditure Panel Survey (MEPS) that highlight individual enrollment, primary source of insurance coverage, and service use and access to care with breakdowns available by age, demographics, and health characteristics. SHADAC produced these estimates using data for years 2016 and 2017, which are the latest available respectively for each survey.
For additional information on data methods and sources used in the data book, see MACPAC’s Technical Guide to MACStats, which provides supplementary information to help readers interpret the exhibits in the MACStats tables and figures as well as to understand the data sources and methods used.