Blog & News
Five-Year Review Shows Rising Trends in Adult E-Cigarette Use: 2017 to 2021
November 9, 2022:|
BRFSS OVERVIEW |
|
Though COVID-19 remains a focal point of concern as the official public health emergency (PHE) is extended, public health researchers and workers have slowly begun to resume attentions to other ongoing and emergent public health crises such as the long-running opioid epidemic, increases in alcohol-related behaviors such as binge drinking and heavy drinking, and e-cigarette use and smoking rates, especially among young adults.
The recent ban and removal of all JUUL e-cigarette products by the U.S. Food and Drug Administration (FDA) is one of the biggest moves to address this issue at the federal level. Additionally, as of June 2022, all 50 states, the District of Columbia, and nearly all U.S. territories have enacted legislation banning sales of e-cigarettes to underage individuals (under age 21). These actions at the federal and state level are aimed at curbing an alarming and persistent rise in e-cigarette usage, especially flavored e-cigarettes, among high-school and middle-school-aged children, as shown in a recent study conducted by the FDA and the Centers for Disease Control and Prevention (CDC). However, the issue of rising e-cigarette use is not limited to only teens and young adults.
Significant Increases Across the States
Nationally, the rate of adult e-cigarette use in 2021 was 6.6 percent. Across the states, e-cigarette use among adults in 2021 ranged from a high of 9.4 percent in Oklahoma to a low of 4.5 percent in Maryland.
Rates of E-Cigarette Use Among Adults, Top Five and Bottom Five States, 2021
While these rates may initially seem low, a comparison to a previous SHADAC analysis on e-cigarette use shows that in just five years the overall rate of adults reporting using e-cigarettes has increased significantly by over two percentage points (PP) from 4.4 percent in 2017.
The range of e-cigarette usage reported by adults across the states has experienced similar trends. From 2017 to 2021*, Oklahoma remained the state with the highest rate of adult e-cigarette use, rising significantly to 9.4 percent in 2021 from 7.1 percent in 2017. The state with the lowest rate of adult e-cigarette use shifted from the District of Columbia (D.C.) in 2017, with a rate of just 2.5 percent, to Maryland in 2021, with a rate of 4.5 percent. Again, the difference between the two lowest rates was statistically significant, indicating an overall increase in e-cigarette use by adults during this time period.
Overall, the states ranking in the top and bottom five for e-cigarette use among adults remained largely unchanged from 2017 to 2021. Kentucky, Oklahoma, and Tennessee remained among the states with the highest rates of reported adult e-cigarette use, with Alabama and Louisiana in 2021 replacing Indiana and Wyoming. Connecticut, Maryland, Vermont, and D.C. remained among the states with the lowest rates of reported e-cigarette use from 2017 to 2021, with New Hampshire in 2021 replacing California.
E-Cigarette Use by Age Group
Most efforts toward curbing rising e-cigarette use have been aimed at teen and young adult age groups, and as the figure below shows, it is easy to see why.
While rates of e-cigarette usage rose across all age groups over the past five years, the highest increases were seen among younger adults age 18-24 and 25-34.
Adult E-Cigarette Use by Age Group from 2017 to 2021
The rate of e-cigarette use among adults age 18-24 nearly doubled, rising by over 8 percentage points from 10.1 percent in 2017 to 18.5 percent in 2021, a statistically significant difference. Similarly, the rates for adults age 25-34 increased significantly from 6.6 percent in 2017 to 11.1 percent in 2021. In fact, all age groups except adults age 45-64 saw significant increases in the rate of e-cigarette use from 2017 to 2021.
Conclusion
In 2019, the CDC began tracking the number of lung injuries and related deaths associated with vaping and e-cigarette use. By early 2020, they revealed that all 50 states, D.C., and several territories were submitting pertinent data to CDC and that the number of lung injuries across the nation had been recorded at 2,807 with deaths recorded at 68. According to recent research from Johns Hopkins University, many of these deaths have not come from regulated market products, but from black market modifications to devices or to vaping liquids—mirroring concerns about current trends in the opioid crisis, which has shifted from prescription (i.e., regulated market) opioid painkillers to unregulated fentanyl that traffickers mix into drugs, leaving consumers unaware of the exact makeup or potency of the product they are purchasing.
While the true effectiveness of state legislations and the FDA ban on e-cigarette products will be revealed with time, they are solid steps towards curbing rising rates of e-cigarette use across a number of age groups in the U.S.
Source: SHADAC Analysis of 2017-2021 Behavioral Risk Factor Surveillance System (BRFSS) public use files.
Notes: * 2019 data is not available. Statistically significant changes at the 95% confidence level unless otherwise noted.
Blog & News
BRFSS Estimates Show Potential Break in Series for Usual Source of Care: New Data on State Health Compare
October 20, 2022:A change to the 2021 BRFSS’ “personal doctor” question has led to large changes in the share of respondents reporting having no personal doctor
The Center for Disease Control’s (CDC) Behavioral Risk Factor Surveillance System (BRFSS) is a long-running, telephone-based state survey designed to monitor trends in adults’ health-related risk behaviors, chronic health conditions, and use of preventive services. SHADAC uses the BRFSS to produce state-level estimates of a number of different measures of health care access and affordability, health behaviors, and outcomes. These measures are posted on State Health Compare and are available by subgroup and over time.
Among these measures is Adults with No Personal Doctor, which quantifies the share of adults who report having no personal doctor. SHADAC tracks this measure because adults with a personal doctor are thought to have better access to care than those with no personal doctor.
The 2021 estimates of those reporting no personal doctor shifted dramatically and across nearly every measured subgroup and state. Notably, these large shifts in estimates corresponded with a change in how the BRFSS asks respondents if they have a personal doctor.
|
Because of this change in methodology and the large, uniform shift in resulting data across various subgroups, we believe the 2021 BRFSS represents a break in series for estimates of “no personal doctor” (and related measures) and do not recommend comparing 2021 estimates to those from prior years. |
This blog post describes changes to the “personal doctor” question and presents evidence of the impact this change had on estimates across the states and relevant subpopulations.
Changes to the “personal doctor” question structure
The table below compares the text of the “personal doctor” question asked in the BRFSS between 2000 and 2020 and the text of the question asked in the 2021 BRFSS. The main difference is that in 2021, the question broadens the concept of “personal doctor” by suggesting respondents consider groups of doctors when identifying whether they have a personal doctor. Specifically, the 2021 question specifically prompts the respondent if there is “one person or a group of doctors” (emphasis added) providing care whereas the question asked through 2020 only asks if there is more than one person who they think of as a personal doctor if the respondent has already indicated they don’t have one person they think of as their personal doctor.
|
2000-2020 BRFSS |
2021 BRFSS |
| "Do you have one person you think of as your personal doctor or health care provider? [If No, read: Is there more than one, or is there no person who you think of as your personal doctor or health care provider?]" 1 Yes, only one 2 More than one 3 No 7 Don't know / not sure 9 Refused |
"Do you have one person or a group of doctors that you think of as your personal health care provider?" 1 Yes, only one 2 More than one 3 No 7 Don't know / not sure 9 Refused |
Fewer people say they have “no personal doctor” using the 2021 question than in previous years
The primary result of this questionnaire change is that fewer people report having “no personal doctor” or other health care provider under the 2021 question compared with the question asked through 2020. This effect is nearly universal among many groups and across nearly every state. This type of change is uncommon and typically results from an update to the survey or its methods rather than from a true change in the population.
As shown below, the 2021 rate of 16.7% was far outside the range of estimates observed since 2011,1 which have been as high as 23.8% in 2013 and as low as 21.5% in 2015.
Percent reporting "no personal doctor" in the 2021 BRFSS was the lowest it has been in 10 years
The figures below present estimates of the share of the adult population who report having no personal doctor, comparing estimates from the 2020 and 2021 BRFSS. As shown in the figure on the left, the total percent of adults reporting no personal doctor was 6.4 percentage points (PP) lower in the 2021 survey (16.7%) compared to the 2020 survey (23.1%). Similar differences were observed across all measured groups (except for uninsured adults), with PP differences ranging from 2.5 PP among adults age 65 or older to 10.0 PP among adults age 25 to 34. As shown in the figure on the right, this was also true across the states, with a smaller share of adults reporting “no personal doctor” in the 2021 BRFSS compared to the 2020 survey in all but Delaware and Oregon. The difference ranged from 2.9 PP in Massachusetts to 13.4 PP in North Dakota.
Percent reporting "no personal doctor" dropped among most groups and nearly all states in the 2021 BRFSS
Further, these results hold when controlling for multiple factors in a multivariate analysis. In a variety of models, all controlling for the factors shown in the previous figures, respondents to the 2021 BRFSS were significantly less likely to report having no personal doctor than respondents to the 2020 BRFSS, with effects ranging from 4.1 PP (Model B) to 4.9 PP (Model C).
Multivariate analysis of rates of “no personal doctor” in 2021 BRFSS vs. 2020 BRFSS
|
|
Model A | Model B | Model C | Model D |
| 2021 coefficient | -0.043 | -0.041 | -0.049 | -0.046 |
| SE | 0.0072 | 0.0074 | 0.0020 | 0.0019 |
| t-score | -55.88 | -55.83 | -25.00 | -23.57 |
| p | <0.000 | <0.000 | <0.000 | <0.000 |
| Model type | OLS, robust SEs | OLS, robust SEs | Survey-weighted OLS | Survey-weighted OLS |
| State fixed effects | No | Yes | No | Yes |
Visit State Health Compare to explore this measure further!
1 The BRFSS implemented cell phone sampling and an advanced weighting method in 2011. For this reason, estimates from before 2011 are not comparable to those from 2011 and later.
Publication
Prevalence and disparities in excessive alcohol use among U.S. adults
 17 million report heavy drinking,
17 million report heavy drinking,
40 million report binge drinking
In the past several years, researchers have shone new light on the public health threat of alcohol consumption in the United States. Nationally, life expectancy has declined, while deaths involving drugs and alcohol have increased.i Those findings are reinforced by studies finding increased high-risk alcohol consumption, such as binge drinking and heavy drinking.ii And early evidence indicates that the COVID-19 pandemic has only accelerated Americans’ alcohol consumption and risky drinking behaviors.iii
The health toll of excessive alcohol consumption affects nearly every segment of the U.S. adult population, as shown by statistically significant growth in alcohol-involved deaths in almost every state and demographic subgroup in a recent SHADAC analysis.iv However, alcohol-involved deaths have not affected the population evenly, with some states and some demographic subgroups experiencing much higher death rates than others.
The analysis in this new brief from SHADAC expert Colin Planalp focuses on high-risk alcohol consumption behaviors that can lead to death and other alcohol-involved diseases. Similar to alcohol-involved deaths, significant differences were found among demographic subgroups in the prevalence of binge drinking and heavy drinking.
Download a PDF of SHADAC's "Prevalence and disparities in excessive alcohol use among U.S. adults" brief.
Related Reading
Size of alcohol, drug overdose death increases in first pandemic year were unparalleled (Blog)
U.S. Health on the Rocks: The Quiet Threat of Growing Alcohol Deaths (Webinar)
Pandemic drinking may exacerbate upward-trending alcohol deaths (Blog)
Escalating Alcohol-Involved Death Rates: Trends and Variation across the Nation and in the States from 2006 to 2019 (Brief and Infographics)
i Case, A. & Deaton, A. (2015, December 8). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. PNAS, 112(49), 15078-15083. https://www.pnas.org/content/112/49/15078
ii Dafna, D., Naimi, T.S., Liu, Y., & Brewer, R. (2020, January 17). Trends in total binge drinks per adult who reported binge drinking—United States, 2011-2017. MMWR Weekly, 69(2), 30-34. https://www.cdc.gov/mmwr/volumes/69/wr/mm6902a2.htm?s_cid=mm6902a2_w#F1_down
iii Grossman, E.R., Benjamin-Neelon, S.E., & Sonnenschein, S. (2020). Alcohol consumption during the COVID-19 pandemic: A cross-sectional survey of US adults. Int J Environ Res, 17(24), 9189. https://www.mdpi.com/1660-4601/17/24/9189
iv Planalp, C., Au-Yeung, C.M., & Winkelman, T.N.A. (2021). Escalating alcohol-involved death rates: Trends and variation across the nation and in the states from 2006 to 2019. State Health Access Data Assistance Center (SHADAC). https://www.shadac.org/sites/default/files/publications/Alcohol-Involved-Deaths/AID-4.21-SHADAC-Brief.pdf
Blog & News
Affordability and Access to Care in 2018: Examining Racial and Educational Inequities across the United States (Infographic)
December 17, 2019: The Centers for Medicare and Medicaid Services (CMS) recently reported that the cost of health care spending in the United States increased by 4.6 percent last year to reach an all-time high of approximately $3.6 trillion.1 This report comes amidst a number of other concerning health care cost-related trends, such as the largest single-year increase for single-coverage premiums in 2018 from $6,368 to $6,715 (5.4 percent) for workers enrolled in employer-sponsored insurance (ESI) and an increase in average household spending on health care (out of pocket expenses, cost-sharing for ESI, and payroll taxes for Medicare, etc.) rising to a record $1.04 trillion.2
The Centers for Medicare and Medicaid Services (CMS) recently reported that the cost of health care spending in the United States increased by 4.6 percent last year to reach an all-time high of approximately $3.6 trillion.1 This report comes amidst a number of other concerning health care cost-related trends, such as the largest single-year increase for single-coverage premiums in 2018 from $6,368 to $6,715 (5.4 percent) for workers enrolled in employer-sponsored insurance (ESI) and an increase in average household spending on health care (out of pocket expenses, cost-sharing for ESI, and payroll taxes for Medicare, etc.) rising to a record $1.04 trillion.2
Rising expenses such as these have contributed to the record number of Americans (25 percent) who reported in 2019 that either themselves or a family member skipped or delayed needed medical care due to cost, according to the results from a new Gallup poll released earlier this month.3
This post examines Americans’ access and ability to afford medical care, focusing on inequities related to race/ethnicity and education, and using two recently updated measures from SHADAC’s State Health Compare: Adults Who Forgo Needed Medical Care and Adults with No Personal Doctor. These measures come from a SHADAC analysis of 2018 data from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS).
Racial and educational inequities persist in adults’ reported ability to afford needed medical care
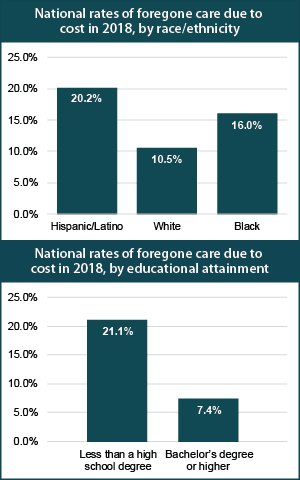 Significant inequities in adults’ ability to afford medical care by race/ethnicity emerged when we examined the updated data for 2018. At the national level, our analysis showed that Hispanic/Latino adults were nearly twice as likely as White adults to forgo needed medical care due to cost (20.2 percent versus 10.5 percent), and African Americans/Black adults were 1.5 times as likely to report forgoing care compared to White adults (16.0 percent versus 10.5 percent). Hispanic/Latino adults were also significantly more likely to report forgoing medical care than White adults in 35 states and D.C., and this gap was greater than 20 percentage points in Maryland (31.4 percent versus 7.4 percent) and Missouri (34.4 percent versus 11.1 percent). Black adults were significantly more likely to report going without care than White adults in 24 states and D.C., and this gap was greater than 10 percentage points in four states: Iowa (16.2 percentage points), North Dakota (15.5 percentage points), Utah (11.5 percentage points), and Minnesota (10.2 percentage points).
Significant inequities in adults’ ability to afford medical care by race/ethnicity emerged when we examined the updated data for 2018. At the national level, our analysis showed that Hispanic/Latino adults were nearly twice as likely as White adults to forgo needed medical care due to cost (20.2 percent versus 10.5 percent), and African Americans/Black adults were 1.5 times as likely to report forgoing care compared to White adults (16.0 percent versus 10.5 percent). Hispanic/Latino adults were also significantly more likely to report forgoing medical care than White adults in 35 states and D.C., and this gap was greater than 20 percentage points in Maryland (31.4 percent versus 7.4 percent) and Missouri (34.4 percent versus 11.1 percent). Black adults were significantly more likely to report going without care than White adults in 24 states and D.C., and this gap was greater than 10 percentage points in four states: Iowa (16.2 percentage points), North Dakota (15.5 percentage points), Utah (11.5 percentage points), and Minnesota (10.2 percentage points).
Nationwide, Americans with less than a high school degree were almost three times as likely to report going without needed medical care due to cost as compared to those with a bachelor’s degree (21.1 percent versus 7.4 percent) in 2018. Adults with less than a high school education were significantly more likely to report forgone care due to cost compared to adults with college degrees in 2018 in all but two states—Montana and Vermont—and in the District of Columbia (D.C.). For four states this gap was greater than 20 percentage points in 2018—Georgia (21.1 percentage points), Maryland (20.9 percentage points), Oklahoma (21.2 percentage points), and Virginia (21.2 percentage points).*
Racial/ethnic minorities and adults without a high school diploma less likely to have a personal doctor
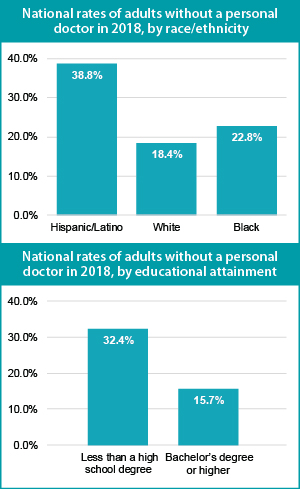 Nationally, Hispanic/Latino and Black adults were both significantly more likely to report not having a regular doctor as compared to their White counterparts. Our analysis revealed that Hispanic/Latino adults were more than twice as likely as White adults to report not having a personal doctor (38.8 percent versus 18.4 percent), and Black adults were nearly 25 percent more likely to report not having a personal doctor compared with White adults (22.8 percent versus 18.4 percent).*
Nationally, Hispanic/Latino and Black adults were both significantly more likely to report not having a regular doctor as compared to their White counterparts. Our analysis revealed that Hispanic/Latino adults were more than twice as likely as White adults to report not having a personal doctor (38.8 percent versus 18.4 percent), and Black adults were nearly 25 percent more likely to report not having a personal doctor compared with White adults (22.8 percent versus 18.4 percent).*
These inequities in access to care by race/ethnicity were present in a large majority of states. A significant gap between Hispanic/Latino and White adults with no personal doctor was present in 43 states, and Hispanic adults were more than three times as likely to report not having a personal doctor in five states (Connecticut, Maryland, Nebraska, New Jersey, and North Carolina). This significant gap also persisted between Black and White adults in 20 states, as we found that Black adults were more than twice as likely to not have a personal doctor in three states—Connecticut (22.8 percent versus 10.8 percent), Iowa (31.2 percent versus 15.1 percent), and Rhode Island (21.2 percent versus 9.9 percent).*
Nationally, adults with less than a high school degree were more than twice as likely to not have a regular doctor as those with an undergraduate degree or greater (32.4 percent versus 15.7 percent). This pattern was consistent across nearly the entire nation, as adults with less than a high school education were significantly more likely than college graduates to report not having a personal doctor in 46 states. The gap between less than high school graduates and college graduates was larger than 20 percentage points in eight states (California, Colorado, Georgia, Maryland, Nebraska, Nevada, New Jersey, and Utah).
Note
* Data were not available or were suppressed for some states because the number of sample cases was too small, so this number could be higher if data were available in all states. For education breakdowns, adults are defined as 25 years of age and above. For race/ethnicity breakdowns, adults are defined as 18 years of age and above. All differences are statistically significant at the 95% level.
Explore Additional BRFSS Data at State Health Compare
Visit State Health Compare to explore national and state-level estimates for the following measures that also come from the BRFSS:
Income Inequality
Sales of Opioid Painkillers
Adult Cancer Screenings
Chronic Disease Prevalence
Activities Limited due to Health Difficulty
Adult Obesity
Adult Binge Drinking
Adult Smoking
Adult E-Cigarette Use (New Measure)
State Health Compare also features a number of other indicator categories, including: health insurance coverage, cost of care, access to and utilization of care, care quality, health behaviors, health outcomes, and social determinants of health.
Related Reading
Now Available on State Health Compare: Eleven Updated Measures and One Brand New Measure
Educational Attainment and Access to Health Care: 50-State Analysis
Fifty-State Analysis Finds Lower Access to Care among Adults with Less Education
[1] Hartman, M., Martin, A.B., Benson, J., & Catlin, A. (2019, December 5). National Health Care Spending in 2018: Growth Driven by Accelerations in Medicare and Private Insurance Spending. HealthAffairs. [E-published ahead of print.] https://doi.org/10.1377/hlthaff.2019.01451
[2] State Health Access Data Assistance Center (SHADAC). (2019, August 14). State-level Trends in Employer-Sponsored Health Insurance, 2014-2018. Retrieved from https://www.shadac.org/ESIReport2019
Murad, Y. (2019, December 5). U.S Health Spending Rose to $3.6 Trillion in 2018, Propelled by Health Insurance Tax. Morning Consult. Retrieved from https://morningconsult.com/2019/12/05/u-s-health-spending-rose-to-3-6-trillion-in-2018-propelled-by-health-insurance-tax/
[3] Saad, L. (2019, December 9, 2019). More Americans Delaying Medical Treatment Due to Cost. Retrieved from https://news.gallup.com/poll/269138/americans-delaying-medical-treatment-due-cost.aspx












