Cost and affordability of health care are understandably at the forefront of consumer concerns as studies show rising health care spending across the nation. SHADAC’s work on these subjects ranges from studies involving primary data collection to assess costs of care, such as care coordination costs; to secondary data analyses of individuals who forgo needed medical care or make changes to prescription drugs due to cost; and of increasing premiums and deductibles in our annual employer-sponsored insurance report. SHADAC staff have also modeled the projected use and cost of Medicaid spending on long-term services and supports for Medicaid enrollees.
Blog & News
Exploring Racial Disparities in Forgone Health Care Using State Health Compare
January 03, 2025:“Forgone care” describes when someone does not use or access health care despite a need for it. While there are a number of reasons why someone might choose to forgo care (e.g., fear of medical procedures or diagnosis, lack of health literacy and/or understanding, limited access to care, cultural beliefs), a very common reason for many is the cost of health care.
Whatever the reason, forgoing or delaying care is correlated with poorer health outcomes, delayed diagnoses, and disruption in care for chronic conditions.1,2 And, unfortunately, disrupted and/or forgone care can actually increase costs for some through further complications, missed preventative treatments, and later diagnoses.
Health care costs are rising in the United States3, and the prices of many other essentials have also gone up since the pandemic.4 As costs and overall pressures on family budgets continue to rise5, it is possible that people will also be more likely to forgo health care.
SHADAC’s State Health Compare tool tracks the percentage of adults who report forgoing care due to cost using data from the Behavioral Risk Factor Surveillance System (BRFSS). In 2023, it’s estimated that 11.6% of adults could not get medical care when they needed it due to cost.
While 11.6% represents how many of all adults reported forgoing care due to cost in 2023, we can look deeper at the phenomenon of forgone care by disaggregating the data and looking at how different factors, like insurance coverage type, sexual orientation, and race / ethnicity, impact rates of forgone care.
Looking at how forgone care due to cost appears for different groups and communities can help us identify disparities that may not be clear from the aggregated data, understand how structural and/or systemic racism might impact health care decisions and outcomes, and help policymakers and others target efforts to make care more accessible.
In this blog post, we are going to explore racial disparities in forgone health care due to cost. Using SHADAC’s State Health Compare tool, we will examine forgone care data broken down by race and ethnicity. Then, we will explore racial disparities in forgone care at the state level.
National Levels of Forgone Care Higher Among Hispanic/Latino, Black, and Other/Multiple Race Adults Compared to White Adults
Using State Health Compare, we examined national levels of forgone care over time for all available race/ethnicity breakdowns: Hispanic/Latino, Black, White, and Other/Multiple Races between 2011 and 2023.
Figure 1. Percent of Adults Who Could Not Get Medical Care When Needed Due to Cost by Race/Ethnicity
Figure 1 shows that each racial / ethnic group’s forgone care follows a similar trendline. Despite similar trends, White adults consistently report the lowest rates of forgone care due to cost. While rates of forgone care due to cost have decreased for all groups compared to 2011, the racial disparities are clear and persistent.
In 2023, rates of foregone care for Black adults (12.7%) and Hispanic/Latino adults (20.1%) were statistically significantly higher than the overall rate (11.6%) and the rate for Whites (8.6%). Since 2021, the percentage of Hispanic / Latino adults who forgo care due to cost has been at least 10 percentage points (PP) higher than White adults.
Forgone Care Due to Cost Differs by State, Ranges Widen for Hispanic/Latino and Black Adults
There is considerable variation across states in the rates of forgone care by race and ethnicity. As Figure 2 shows, state by state rates of forgone care due to cost range from 4.8% of White adults in Hawaii to 30.4% of Hispanic/Latino adults in Georgia .
Figure 2 also highlights the extent to which the range of forgone care across states differs by race and ethnicity, with Hispanic/Latino adults having higher rates consistently across states. For example, the highest rate among Hispanic/Latino adults (Georgia, 30.4%), is more than double the highest rate for White adults (Tennessee, 13.6%). Similarly, the lowest rate among Hispanic/Latinos (Hawaii, 9.2%) is close to double the lowest rate for White adults (Hawaii, 4.8%).
Figure 2. Forgone Care Due to Cost for Black, Hispanic, and White Adults by State

Low Rates of Forgone Care Overall Mask Racial Disparities
Figure 3 ranks the fifty states and D.C. by overall rates of forgone care. As shown, Hawaii, Vermont, Massachusetts, Iowa, and New Hampshire have some of the lowest rates of foregone care in the country.
Figure 3. Forgone Care Due to Cost for All Adults by State
What happens when we breakdown by race / ethnicity?
Figure 4. Forgone Care Due to Cost By State and By Race / Ethnicity

*Significant difference from White
When we disaggregate the data in states with low overall rates of forgone care, racial disparities are revealed.
Let’s take Massachusetts as an example since that is a state where we have data for each group. In Massachusetts, the only group that has a rate equal to or less than the overall rate is White adults at 5.0%. All of the other racial / ethnic groups with available data have rates that are significantly higher than White adults, with Black adults having more than double (10.7%) and Hispanic/Latino adults having almost triple (14.8%) the rate of forgone care compared to White adults.
Health Equity Considerations & Conclusion
Racial disparities in health care can come in a number of forms; as seen in this blog, there are important disparities in forgone care among adults by race and ethnicity. These disparities appear in most states, even states with low overall rates of forgone care, and the disparities are even more stark in certain states. Low overall rates of forgone care can mask these racial disparities – disaggregating data and looking at differences between groups is crucial for identifying and closing gaps & health disparities.
In some circumstances in this blog , we used White as the comparison group to test for statistically significant differences across racial and ethnic groups. This was because White adults had the lowest rates of forgone care, and are, generally, the most structurally advantaged compared to the other groups.
However, we want to acknowledge that this method is not always appropriate; as Whitfield et al remarks in a study on comparing racial groups: “There is an assumption of differences, but different from what?” Continuously using White groups as the basis of comparison can perpetuate the false narrative that White is a “standard” that racial/ethnic minorities differ from, which serves to ‘other’ those minority groups instead of treating each as distinct, and varied, groups with different social, cultural, and systemic/structural influences.6
There are also equity issues related to data availability — states are much more likely to have insufficient data for Black, Hispanic/Latino, and people who identify as other/multiple races. Excluding PA and KY (both states did not have sufficient data to be included in the 2023 BRFSS public data file and are not included in the national data), data is not available for:
- Other/Multiple Race adults in two states (NC and RI)
- Hispanic/Latino adults in three states (MS, WV, and VT)
- Black adults in 11 states (HI, ID, MT, ND, NH, NM, OR, SD, WY, UT, and VT)
Improving data collection for those of minority groups on surveys like the BRFSS could help to highlight important differences between states and groups that are not visible with the current data.
Finally, we acknowledge that grouping responses in to “Other/Multiple Races” may obscure important disparities within this diverse group. Efforts are being made to improve demographic data collection, like the newly revised standards from the OMB on federal race/ethnicity data collection; improving sample size and data collection methodology are important steps towards centering health equity, making critical disparities visible to researchers, policymakers, and community members.
Continue to explore this and more data on our interactive online data tool, State Health Compare.
Notes
All statistically significant differences were based on two-sided t-tests at the 95% level of confidence, indicating that these changes were likely to reflect true changes in the population given the available data. Lack of statistically significant changes does not indicate certainty that there was no true population change, but rather that any true population change was not detectable with the available data.
These results represent rates of adults that forgo needed medical care due to cost for the civilian non-institutionalized population who are 18 years and over.
Citations
1. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2775366
2. https://pmc.ncbi.nlm.nih.gov/articles/PMC8683898/
5. https://www.census.gov/newsroom/press-releases/2024/renter-households-cost-burdened-race.html
Publication
WEBINAR: U.S. Census Bureau Data Explained: Breaking Down 2023 Health Insurance Coverage Estimates from the ACS & CPS - featuring a Q&A with a Census Bureau Expert

This presentation is a part of our Survey Data Season series where we examine data from various surveys that are released annually from the summer through early fall. Find all of the Survey Data Season series posts on our Survey Data Season 2024 page here.
On Thursday, September 26th at 1:00 PM CST, SHADAC hosted a webinar covering the release of new Census data on health insurance coverage estimates for 2023. The estimates come from two key federal surveys conducted by the U.S. Census Bureau: The American Community Survey (ACS) and the Current Population Survey (CPS).
SHADAC researchers and presenters Robert Hest and Andrea Stewart discussed the 2023 health insurance data at national and state levels, as well as by coverage type, and a range of other demographic categories (age, geography, poverty level, and more). In addition, SHADAC walked through how to access the data and examples of how to use it to answer research questions. We were also pleased to once again welcome a special guest from the Census Bureau, Sharon Stern, who joined the end of the webinar to participate in a Q&A, answering questions from attendees.
Webinar attendees came away knowing more about:
- The new 2023 health insurance coverage estimates
- How to access the estimates via Census reports and the data.census.gov website
- How to access state-level estimates from the ACS using SHADAC’s State Health Compare web tool
- When and how to use 2023 Census data to understand health insurance coverage trends
Find a recording of this webinar, along with presentation slides and a transcript of webinar audio, below.
Find the slides from this presentation here. Find a transcript of this webinar here.
Speakers
 Elizabeth Lukanen, Moderator
Elizabeth Lukanen, Moderator
Deputy Director, SHADAC
Ms. Lukanen serves as the Deputy Director for SHADAC, overseeing center research and providing strategic direction and oversight. With 20 years of experience in the health policy arena, Ms. Lukanen specializes in managing complex projects and translating quantitative findings into actionable, policy-relevant information. Ms. Lukanen currently oversees SHADAC’s technical assistance to states in the areas of data use, analysis, and evaluation. Ms. Lukanen is vocal about the importance of collecting and reporting disaggregated data to explore issues related to health equity, while actively working with policymakers to improve data on race, ethnicity, sexual orientation, and gender identity.
 Robert Hest, Speaker
Robert Hest, Speaker
Senior Research Fellow, SHADAC
Robert Hest joined SHADAC in 2017, providing expertise in survey data, quantitative data analysis, data visualization, and health coverage policy. Mr. Hest leads SHADAC’s work monitoring and investigating developments in the measurement of health insurance coverage and health care access, affordability and utilization in federal survey data. He also manages SHADAC’s State Health Compare website, coordinating data processing, quality assurance, dissemination, and documentation of data used on the site and leads SHADAC’s work in the Minnesota Research Data Center applying restricted-use data to analyze health care affordability, access, and utilization at the state level.
 Andrea Stewart, Speaker
Andrea Stewart, Speaker
Research Fellow, SHADAC
Andrea Stewart joined SHADAC in 2018 as a Marketing and Communications Specialist, transitioning to a Research Fellow in 2022. Currently, Ms. Stewart leads SHADAC’s efforts to track and report health insurance coverage data from major federal surveys, and is involved in several other ongoing projects, including an effort to explore the potential for the creation of a Medicaid Equity Monitoring Tool. Portions of her other research work range in topic from health equity measurement to understanding the impacts of COVID-19 on federal survey data.
 Sharon Stern, Speaker
Sharon Stern, Speaker
Assistant Division Chief, U.S. Census Bureau
Sharon Stern is the Assistant Division Chief for employment characteristics in the U.S. Census Bureau’s Social, Economic and Housing Statistics Division. In her position, Ms. Stern oversees statistics on the labor force, health insurance and disability from several Census Bureau surveys. She has authored a wide variety of Census Bureau reports and papers on topics related to poverty, disability, and health insurance.
Stay up to date with our latest posts by joining our mailing list and following us on LinkedIn.
Blog & News
Integrated Health Partnerships—Minnesota’s Medicaid Accountable Care Organization Model
August 16, 2024:Minnesota's Integrated Health Partnerships (IHPs) have pioneered a new approach to implementing accountable care organizations (ACOs) for the Medicaid population. Initially launched in 2013 by the Minnesota Department of Human Services (DHS), these partnerships are voluntary agreements between health provider groups and DHS. Health provider groups partner directly with DHS in multi-year contracts to both improve the quality of and reduce the total cost of care for specified patient populations using a shared savings/shared risk financing model.
When IHPs were first established in Minnesota, there were six provider groups participating. A little more than 10 years later, the number of IHPs in Minnesota has more than tripled, with 25 total partnerships covering more than 505,000 beneficiaries, as of July 2024.
DHS released the 2025 Request for Proposals (RFPs) (which recently closed) hoping to expand the program to more interested organizations and to allow current organizations to continue their partnership with the agency.
In order to better understand potential expansions and changes that may be implemented through Minnesota’s IHPs, we must first understand the foundation, function, and purpose of these partnerships.
In this blog, SHADAC staff will explore:
- What is the purpose of an Accountable Care Organization (ACO)?
- How do IHPs relate to ACOs?
- How have IHPs been established in Minnesota and how have they evolved?
- How can IHPs advance health equity for included populations?
- What are some future considerations that could help in better understanding the effect of IHPs?
Keep reading to start learning about the IHP program and how it impacts communities in Minnesota.
ACOs in Medicaid
Accountable Care Organizations (ACOs) are groups of health care providers that agree to take financial responsibility for the quality and cost of care they deliver to a defined patient population. There are national, state, and regional ACO models, and they may support multiple insured populations, i.e., Medicare, Medicaid, commercial, and self-insured.
ACOs often operate alongside Managed Care Organizations (MCOs), offering additional avenues for health care reform and focusing increasingly on advancing health equity. ACOs are a pivotal tool in promoting access to care, investing in population health, and addressing social determinants of health that affect health equity.
Since the enactment of the Affordable Care Act (ACA) in 2010, the Center for Medicare and Medicaid Innovation (CMMI) has supported state initiatives like Minnesota's State Innovation Model (SIM) to test and expand ACO models within Medicaid, and Medicaid-specific ACOs have now been established in nearly a dozen states.*
These programs vary by state in terms of delivery system reform, payment expectations, and in the authorities needed to administer them, but all such Medicaid ACO alternative payment models (APMs) are standardized through classification under Categories 2, 3, and 4 of the Health Care Payment – Learning Access Network (HCP-LAN) APM framework.
IHPs are Minnesota’s Medicaid ACO model. In 2008, the Health Reform Law of Minnesota included recommendations for statewide quality reporting, payments for coordinated care services provided in health care homes (HCHs), and encouragement to participate in bundled payment demonstrations. The law was then amended in 2011 to require DHS to develop a program to “test alternative and innovative health care delivery systems, including ACOs that provide services to a specified patient population for an agreed-upon total cost of care or risk/gain sharing payment arrangement”, leading to the creation of IHPs.
In 2017, SHADAC had the opportunity to conduct an evaluation of early Minnesota IHP implementation as part of Minnesota’s SIM cooperative agreement with CMMI, which documented IHP expansion and evolution, helpful data analytics, and importance of ongoing monitoring of the effects of the IHP program on health care utilization, cost, and quality.
Minnesota's Integrated Health Partnerships Today
As noted earlier, Minnesota’s IHP program began over 10 years ago in 2013. In 2018, the program was updated with various enhancements and changes in order to place a stronger focus and effort on health equity, enhance the risk arrangement incentives, and provide a population-based payment. This led to the implementation of a new overall IHP model (Integrated Health Partnerships 2.0) with two possible tracks for Minnesota IHPs to operate under (see figure below). These two distinct organizational design tracks are tailored to both provider capabilities and population needs.
For full details and requirement on IHP design tracks, please reference the Minnesota Department of Human Services 2025 Request for Proposals for IHP Program
On top of improving care quality and reducing the total cost of care, IHPs on both tracks are also required to design interventions that address specific health disparities across their target population. IHPs in both tracks receive a quarterly risk-adjusted population-based payment (PBP) which is intended to contribute to care coordination and other investments for the population served. IHPs are also assessed based on quality, utilization, and health equity measures. This population-based payment is flexible, adjusting to reflect changing numbers of the included population specified by the IHP’s intervention plan, as well as changing risk factors due to medical and social complexities in the population makeup.**
IHPs are measured through quality and data metrics (e.g., comparing percent change between performance years), as well as a calculation of standards across five domains for those in the shared-risk model - Quality Core Set, Care for Children and Adolescents, Quality Improvement, Closing Gaps, and Equitable Care - a process which is described in further detail in the following section.
Ultimately, IHPs have proven quite successful in Minnesota, with significant savings and quality improvements. Since their inception, IHPs have yielded nearly $546 million in total savings through 2022.
Emphasis on Advancing Health Equity
In response to evolving health care needs and feedback suggesting that the timing was right to build on prior successes of the original IHP program, DHS introduced an improved program, IHP 2.0, enhancing its focus on health equity. The IHP 2.0 program, included modifications to allow the program to more directly address social determinants of health (SDOH) and incentivize partners to reduce racial, geographical, and/or other disparities.
The Minnesota Department of Health describes health equity as “addressing health disparities as part of a broad spectrum of public investments in housing, transportation, education, economic opportunity and criminal justice.” By implementing changes and integrating health equity goals into core operational frameworks, the hope with the IHP 2.0 program is to overcome the limitations of traditional health care approaches in addressing SDOH and health disparities that arise as a result.
In fact, recent case studies on Medicaid payment reforms conducted by the Urban Institute directly referenced and cited Minnesota’s IHPs, describing their influence on health equity along with the overall changes made to the program in 2018 in order to continue to advance equity in Medicaid.
The table below from the Urban Institute identifies and describes the core features of the IHP 2.0 program designed to both focus on and advance equity for beneficiaries.
Source: Allen & Willis, “Can Medicaid Payment and Purchasing Strategies Advance Health Equity?” The Urban Institute, December 2023, https://www.urban.org/sites/default/files/2023-12/Can%20Medicaid%20Payment%20and%20Purchasing%20Strategies%20Advance%20Health%20Equity_0.pdf
As described above, the success of IHPs is evaluated based on performance in health care quality, utilization, health equity, and total cost of care (TCOC). When monitoring quality for those in risk arrangements where quality has an impact on shared savings and losses, the quality-related assessments are organized into five domains.
As a reminder, those domains are as follows:
- Quality Core Set
- Care for Children and Adolescents
- Quality Improvement
- Closing Gaps
- Equitable Care
Two of these domains, “Closing Gaps” and “Equitable Care,” specifically target health equity through tailored clinical and utilization measures aimed at reducing and eliminating disparities among specific Medicaid populations. IHPs can also receive ‘bonus points’ on their overall quality score for creating additional initiatives under the Quality Improvement, Closing Gaps, and Equitable Care domains.
Recent Health Equity Interventions
As a part of the enhanced focus on health equity, IHPs are encouraged to design interventions to address targeted populations’ health equity challenges.
Target populations may differ among the IHPs, with some initiatives aimed at supporting the entire IHP patient population and some designed to serve a more specific sub-population. A summary list of common target populations of Minnesota’s 25 IHPs include:
- Children, adolescents, families, and new mothers
- Justice-involved individuals
- Patients with a mental illness or individuals living with a family member with a mental illness
- Patients that are food insecure
- Adults with substance use disorder
- Individuals experiencing challenges accessing care, including Black, Indigenous, and people of color
A summary list of common social risk factors across Minnesota’s 25 IHPs include:
- Housing instability
- Food insecurity
- Social isolation
- Transportation
- Difficulty paying bills
- Education
- Employment
- Mental health needs
- Access to care
- Language barriers
- Income
- Childcare
IHPs must first identify the population or populations that they are serving, and then they must design, develop, and implement targeted intervention efforts based on those populations, risk factors, and SDOH to advance equity for those groups. IHPs are encouraged to identify an intervention that will meet the needs of their specific population given their knowledge of their community. Examples of these efforts include community partnerships, screening initiatives, referrals to community resources or other needed programs, and care coordination for social needs. The following is a summary list of common interventions currently being used to address health equity across Minnesota’s 25 IHPs:
For a full list, the Health Equity Interventions Summary at this link provides the specific target population, social risk factors, interventions, and milestone components for each IHP in Minnesota.
Closing Thoughts
As DHS’ IHP Program continues to evolve, its focus on data analytics and population health management remains pivotal for achieving comprehensive care delivery and advancing health equity statewide. The IHP 2.0 Program exhibits the importance of translating equity-focused policy goals into actionable requirements and programs. DHS’ work to monitor and disseminate the outcomes of the health equity initiatives and interventions implemented by IHPs will continue to provide valuable insights into their effectiveness and impact on Minnesota's health care landscape.
One potential dissemination method would be to make the Population Health Reports from IHPs publicly available. This would not only increase transparency around the data collected by IHPs and the lessons learned from putting interventions into practice, but also aid in our understanding of the effectiveness of IHPs in addressing SDOH, improving access to care, and eliminating health disparities.
Continue learning about health equity in Medicaid and beyond with the following SHADAC products:
Notes
Blog & News
Disability Health Care Data and Information: Resources from SHADAC
January 09, 2025:- Unfair treatment in health care settings, at work, or when applying for public benefits
- Adults with disabilities are more likely to live in poverty compared to adults with no disability
- People with a disability often have increased medical expenses, with a study from the National Disability Institute estimating that a U.S. household containing an adult with a disability must spend an estimated 28% more income to obtain the same standard of living as a household with no disability
- Those with disabilities have twice the risk of developing chronic health conditions like depression, diabetes, asthma, and poor oral health
Federal Survey Sample Size Analysis: Disability, Language, and Sexual Orientation and Gender Identity
- People who indicated sexual orientation or gender identity (SOGI)
- People with language access needs, and
- People with disabilities
Collection of Self-Reported Disability Data in Medicaid Applications: A Fifty-State Review of the Current Landscape (SHVS Brief)
State Health Compare Disability Breakdowns
Housing Affordability Matters: Unaffordable Rents Infographics Updated with 2022 Data
Minnesota Community and Uninsured Profile
Stay Informed on Disability Health Data Resources and Information
Blog & News
Exploring Cost and Coverage Rates in Employer-Sponsored Insurance (Infographic)
September 5, 2023:Throughout the United States, a majority of Americans and their families receive health insurance coverage through their employer. In 2021, the number of people covered by this type of coverage—known as employer-sponsored insurance or ESI—exceeded 169 million. While a fuller picture of the coverage landscape will be available later this fall as agencies such the U.S. Census Bureau release more health insurance data, in this blog and infographic, SHADAC researchers use recently released data from the Medical Expenditure Panel Survey-Insurance Component (MEPS-IC) to analyze private-sector ESI and provide an initial snapshot of estimates for 2022 on a national level and within the states.
Key Findings (2022 vs. 2021)
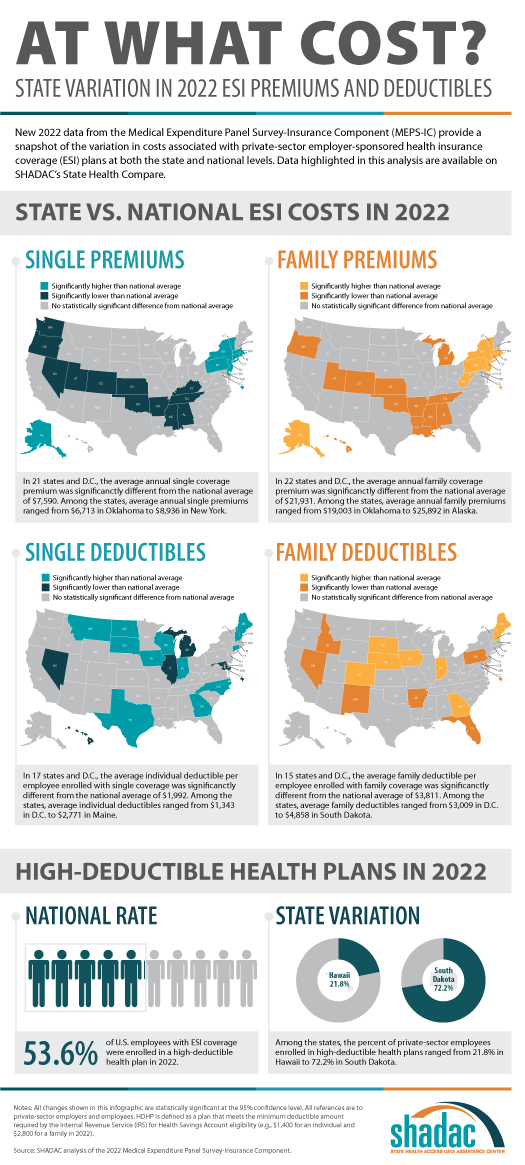 Employee Access to Coverage
Employee Access to Coverage
- The offer of employer-sponsored insurance coverage was extended to a large majority of private-sector workers. In 2022, 85.6% of employees in the U.S. worked in establishments that offered health insurance coverage, a rate that was statistically unchanged from 2021 (85.7%).
Employee Coverage Costs
Premiums
- The average annual premium for single coverage significantly increased to $7,590 in 2022, a $210 or 2.8% increase from 2021.
- Among the states, average annual single premiums ranged from $6,713 in Oklahoma to $8,936 in New York.
- For those enrolled in family coverage, average annual premiums also significantly increased. In this case, premiums increased to $21,931 in 2022, a $550 or 2.6% increase from 2021.
- Among the states, average annual family premiums ranged from $19,003 in Oklahoma to $25,892 in Alaska.
Deductibles
- For single coverage, the 2022 average individual deductible was $1,992, unchanged from 2021 ($2,004).
- Among the states, average individual deductibles ranged from $1,343 in D.C. to $2,771 in Maine.
- Among those enrolled in family coverage, the average deductible per employee enrolled was $3,811 in 2022. This was also unchanged from 2021 ($3,868).
- Among the states, average family deductibles ranged from $3,009 in D.C. to $4,858 in South Dakota.
High-Deductible Health Plans*
- In 2022, the share of employees enrolled in high-deductible health plans (HDHPs) decreased significantly in 2022 to 53.6% – a decrease of 2.1 percentage points from 2021.
- Among the states, the percent of private-sector employees enrolled in high-deductible health plans ranged from 21.8% in Hawaii to to 72.2% in South Dakota.
Key Takeaways
With so many Americans relying on an employer for health insurance coverage, measures of ESI coverage and cost remain important indicators of the financial and health burdens many individuals and families face. These measures will be of greater importance going forward as some current Medicaid enrollees may transition to employer coverage during the 2023-2024 unwinding of the Medicaid continuous coverage requirement. SHADAC is monitoring the unwinding process through a variety of avenues, including: federal surveys, state dashboards, and state-based marketplace data.
In 2022, as in previous years, premiums continued to rise, though premium increases were small compared to the relatively high rate of inflation in 2022. Average deductibles were unchanged from 2021, which represents a break from the long-running trend of increasing deductibles. Additionally, the share of private sector employees enrolled in high-deductible plans decreased by a small but statistically significant margin, which represented the first decrease since 2013. With regard to coverage, a large majority of workers were employed in establishments that offered health insurance coverage, and this was unchanged from 2021.
Notes and Sources
* High-deductible health plans (HDHP) are defined as plans that meet the minimum deductible amount required for Health Savings Account (HSA) eligibility ($1,400 for an individual and $2,800 for a family in 2022).
Data are from the 2022 Medical Expenditure Panel Survey–Insurance Component (MEPS-IC), produced by the Agency for Healthcare Research and Quality (AHRQ).
Health insurance coverage estimates through 2021 are available on SHADAC’s State Health Compare web tool at statehealthcompare.shadac.org, and estimates for 2022 will be added soon.