Cost and affordability of health care are understandably at the forefront of consumer concerns as studies show rising health care spending across the nation. SHADAC’s work on these subjects ranges from studies involving primary data collection to assess costs of care, such as care coordination costs; to secondary data analyses of individuals who forgo needed medical care or make changes to prescription drugs due to cost; and of increasing premiums and deductibles in our annual employer-sponsored insurance report. SHADAC staff have also modeled the projected use and cost of Medicaid spending on long-term services and supports for Medicaid enrollees.
Blog & News
Now Available on State Health Compare: One Brand New Measure and Five Updated Measures
May 26, 2023:Estimates for five measures of health care access, affordability, and use have now been updated on SHADAC’s State Health Compare. One new measure, Had Telehealth Visit, has also been added to State Health Compare. The new and updated measures are all produced using data from the National Health Interview Survey (NHIS), conducted by the National Center for Health Statistics (NCHS). SHADAC produces these state-level measures using restricted-access data through the Minnesota Research Data Center (MnRDC). SHADAC’s State Health Compare is the only source of state-specific data for these measures which are essential for monitoring individuals’ access to and use of medical care, along with their ability to afford care.
These measures now contain data through 2021, using two-year pooled periods (i.e., 2019-2020, 2020-2021). The measures can be broken down by Total, Age, and Coverage Type (Public, Private, Uninsured).
Updated and new measures include:

 NEW: Had Telehealth Visit
NEW: Had Telehealth Visit
This measure describes the percent of individuals who had a medical appointment by video or phone during the past twelve months.

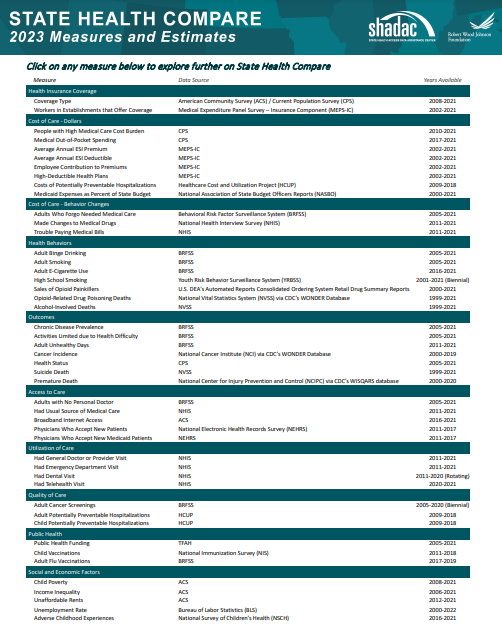 Had Usual Source of Medical Care
Had Usual Source of Medical Care
This measure captures rates of individuals who had a usual place of medical care other than an emergency department during the past twelve months.
 Had General Doctor or Provider Visit
Had General Doctor or Provider Visit
This measure provides rates of individuals who had any visit to a general doctor or provider within the last year.
 Had Emergency Department Visit
Had Emergency Department Visit
This measure looks at rates of individuals who had any type of visit to an emergency department in the past twelve months.
 Trouble Paying Medical Bills
Trouble Paying Medical Bills
This measure examines rates of individuals who had trouble paying off medical bills during past twelve months.
 Made Changes to Medical Drugs
Made Changes to Medical Drugs
This measure highlights rates of individuals who were prescribed medication in the past twelve months who made changes to their medical drugs due to cost during the past twelve months. This includes delaying filling a prescription, taking less medicine, or skipping doses to save money.
Click here to explore these measures on State Health Compare!
Notes: Data for State Health Compare’s Had Dental Visit measure is only asked in the NHIS rotating core and thus was not asked in the 2021 survey. We will be able to update that measure with new data after both the 2022 and 2023 data are out in mid-2024.
All measures are representative of the civilian noninstitutionalized population.
Data Source: The estimates were produced using restricted NHIS data in the MnRDC. Measures have been updated with data through 2021 using two-year pooled periods, including (a) 2011–2012 through 2017–2018 and (b) 2019-2020 through 2020-2021, except in the case of the telehealth measure for which data is only available from 2020-2021.
Blog & News
SHADAC in JHPPL: The Future of State All-Payer Claims Databases
January 24, 2023:This journal article was originally published in Volume 48, Issue 1 of the Journal of Health Politics, Policy and Law (JHPPL).
Authors: Lynn A. Blewett, PhD, MPA, Natalie Schwehr Mac Arthur, PhD, MAc, and James Campbell
SHADAC researchers recently published an article in the Journal of Health Politics, Policy and Law on states’ development and use of state-based all-payer claims databases (APCDs).
Abstract
State policymakers are under increasing pressure to address the prohibitive cost of health care given the lack of action at the federal level. In 2020, the United States spent more on health care than any other country in the world—$4.1 trillion, representing 19.7% of the nation's gross domestic product. States are trying to better understand their role in health care spending and to think creatively about strategies for addressing health care cost growth. One way they are doing this is through the development and use of state-based all-payer claims databases (APCDs). APCDs are health data organizations that hold transactional information from public (Medicare and Medicaid) and private health insurers (commercial plans and some self-insured employers). APCDs transform this data into useful information on health care costs and trends. This article describes states' use of APCDs and recent efforts that have provided benefits and challenges for states interested in this unique opportunity to inform health policy. Although challenges exist, there is new funding for state APCD improvements in the No Surprises Act, and potential new federal interest will help states enhance their APCD capacity so they can better understand their markets, educate consumers, and create actionable market information.
Read the full research article in Volume 48, Issue 1 of the Journal of Health Politics, Policy and Law.
Blog & News
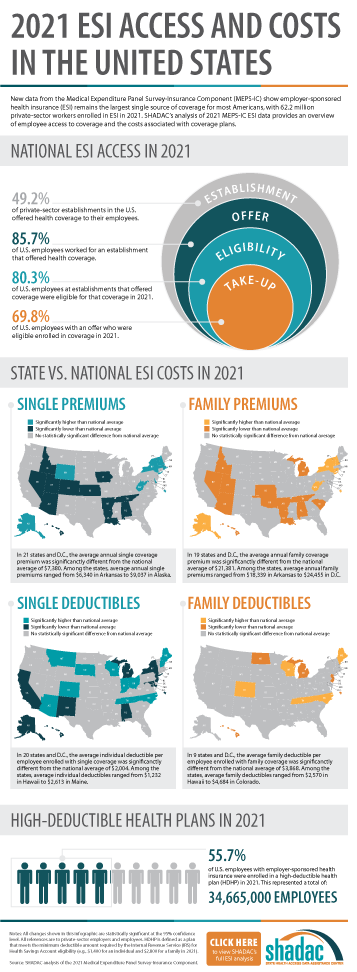
Employer-Sponsored Insurance (2019-2021): A National-Level Look at Cost and Coverage Rates (Infographic)
August 30, 2022:Throughout the United States, a majority of Americans and their families receive health insurance coverage through their employer. In 2021, the number of individuals enrolled in this type of coverage–known as employer-sponsored insurance or ESI–exceeded 62.2 million. In this blog, infographic, and companion documents, SHADAC researchers use data from the Medical Expenditure Panel Survey-Insurance Component (MEPS-IC) to analyze the private-sector ESI landscape in 2021 on a national level and within the states. As discussed in SHADAC’s 2020 ESI coverage blog, the COVID-19 pandemic complicated the collection and analysis of data throughout recent years, leading our researchers to compare 2021 ESI access data against pre-pandemic (2019) estimates and 2021 ESI cost data against 2020 estimates.
Key Findings
Employee Access to Coverage (2019 vs. 2021)
Establishment
Not all private sector establishments offer their employees health insurance coverage. In fact, slightly less than half of establishments in the U.S. offered coverage in 2021 (49.2%). This was a significant increase from 47.4% in 2019.
Offer
The offer of employer-sponsored insurance coverage was extended to the majority of private-sector employees. In 2021, 85.7% of employees in the U.S. worked in establishments that offered health insurance coverage, a rate that remained statistically unchanged from 2019 (85.3%).
Eligibility
Among employees working at establishments that offered coverage, the percent eligible for coverage was 80.3% in 2021; an increase from 77.7% in 2019.
Take-Up
The take-up rate of ESI-eligible employees has varied over the years, and in 2021, 69.8% of eligible employees enrolled in coverage. This represented a 2.1 percentage-point decrease from 2019 (71.9%).
Employee Coverage Costs (2020 vs. 2021)
Premiums and contributions
- The average annual premium for single coverage rose to $7,380 in 2021, a $231 or 3.2% increase from 2020.
- For those enrolled in family coverage, average annual premiums also rose. In this case, premiums climbed to $21,381 in 2021, a $623 or 3.0% increase from 2020.
Deductibles
- For single coverage, the 2021 average individual deductible was $2,004. This represented a significant increase of 3.0% from 2020 ($1,945).
- Among those enrolled in family coverage, the average deductible per employee enrolled was $3,868 in 2021. This was also a significant increase of 3.9% from 2020 ($3,722).
High-Deductible Health Plans
- In 2021, the share of employees enrolled in high-deductible health plans (HDHPs) increased substantially in 2021 to 55.7% – an increase of 5.3 percentage points from 2020.
Key Takeaways
With so many Americans relying on their employers for health insurance coverage, ESI findings remain an important indicator of the financial and health burdens many individuals and families face. In 2021, the U.S. experienced several continuing ESI trends, including rising costs across employee premiums, premium contributions, and deductibles. Additionally, the share of private sector employees enrolled in high-deductible plans increased substantially. In regards to coverage, more employers offered ESI to their employees in 2021 when compared to pre-pandemic levels. Meanwhile, the rate of ESI-eligible employees enrolling in offered coverage was down overall from pre-pandemic, though unchanged from 2020.
For more detailed information on ESI findings from SHADAC, see the following products:

 Report Narrative
Report Narrative
The report narrative provides an in-depth look at 2019-2021 ESI estimates including state-level changes and trends.
50-State Comparison Tables
The 50-state tables include 2017-2021 ESI estimates and allow for easy cross-state and state vs. national analysis.
Other related resources
• 2021 ESI Blog (2019-2020 data)
• 2020 ESI Report, Blog, and Infographic (2015-2019 data)
• 2019 ESI Report, Blog, and Infographic (2014-2018 data)
Blog & News
State and Federal Relief Prevented Deep Backslide in Health Care Affordability in California in 2020 (CHCF Cross Post)
May 18, 2022:The following content is cross-posted from California Health Care Foundation. It was first published on May 18, 2022.
Author: Colin Planalp, Research Fellow, SHADAC
In 2020, the start of the COVID-19 pandemic meant the imposition of incredible burdens on every corner of US society, particularly the health care system and the people it serves. There were well-founded fears that the pandemic, and the concurrent economic crisis, could make health insurance and health care unaffordable for even more people — already a long-standing problem in California.
In response to the pandemic, the US government enacted historic relief programs, including multiple instances of direct cash payments to a majority of US families. Those federal policies coincided with California health insurance reforms that, while developed before the pandemic, were implemented in 2020.
This analysis of the California Health Insurance Survey (CHIS) shows that Californians were largely protected from experiencing a major erosion in their ability to pay for health insurance and care. Despite this overall positive finding, the 2020 CHIS data on health care affordability continued to demonstrate clear inequities by income and race/ethnicity.
Key Findings
California’s uninsured rate declines, yet cost remains top reason for lacking health insurance. The rate of Californians under 65 without health insurance reached a historic low of 7.0% in 2020. However, 51.9% of uninsured people said they lacked coverage because it was too expensive.
Rate of going without needed care due to cost dropped in 2020. Among the 8.6% of Californians who reported forgoing needed medical care in 2020, 32.0% said it was concerns about the cost that caused them to go without care. That rate was significantly lower than the rate of 43.6% in 2019.
Fewer Californians reported difficulty paying medical bills. From 2019 to 2020, the rate of Californians reporting that they’ve had trouble paying medical bills in the past year declined significantly, from 13.3% to 11.1%. However, when breaking out the data by income, only those with higher incomes saw statistically significant improvement. Californians with lower incomes — 200% to 299% of federal poverty guidelines (FPG), 100% to 199% FPG, and below 100% FPG — reported no significant changes.
Less trouble affording necessities due to medical bills in 2020. In 2020, the rate of Californians who reported having trouble paying for basic necessities (such as food or clothing) because of medical bills declined significantly to 31.0% from 39.8% in 2019. Rates of trouble paying for necessities due to medical bills also declined across most income levels.
Practice of using credit card debt to finance medical bills declined. In 2020, the rate of Californians who reported taking on credit card debt to finance medical bills declined significantly, from 56.5% in 2019 to 44.3%. That finding held consistent for Californians across income levels — except for those with the lowest incomes.
Racial and ethnic disparities persisted in 2020. Although California experienced significant improvements in some measures of health care and insurance affordability in 2020, certain long-standing inequities persisted. For example, Black people reported the highest rate of trouble paying medical bills in 2020, at 14.0%, followed closely by Latinos/x, at 12.7%. Asians, Black people, and Latinos/x also reported similarly high rates of trouble paying for necessities due to medical bills (39.4%, 36.2%, and 33.1%, respectively).
Together, these findings provide some encouraging news. In a year of massive economic upheaval that would typically have caused serious financial problems for many Californians, they instead reported improvements in health care and insurance affordability. However, improvements were likely due, at least in part, to federal programs that were mostly designed to be temporary. Some have already expired. Additionally, the historically high inflation of 2021 and 2022 have since strained people’s finances.
But the fact that California experienced such measurable improvements in health insurance and health care affordability during a broad and deep recession shows that those problems don’t have to be intractable. In the future, it will be key to monitor these measures as policymakers in California and at the federal level consider initiatives to protect people against unaffordable health care and insurance costs, which remain a long-term challenge.
SHADAC Expertise
Health Care Cost and Affordability
Health care cost and affordable health care are understandably at the forefront of consumer concerns as studies show rising health care spending across the nation. For over a decade, SHADAC has monitored and produced reports on health care cost and affordability trends through primary data collection and secondary data analysis. SHADAC’s work on these subjects ranges from studies involving primary data collection to assess costs of care, such as care coordination costs; to secondary data analyses of individuals who forgo needed medical care or make changes to prescription drugs due to cost; and of increasing premiums and deductibles in our annual employer-sponsored insurance report. SHADAC staff have also modeled the projected use and cost of Medicaid spending on long-term services and supports for Medicaid enrollees.
Related SHADAC Work:
Click on any title below to learn more about the project.
 Affordability and Access to Care: Examining Inequities Across the United States
Affordability and Access to Care: Examining Inequities Across the United States
Various SHADAC analyses examine Americans’ health care costs, access to care, and ability to afford medical care. Many of our analyses explore inequities related to race/ethnicity and education, often using measures from SHADAC’s State Health Compare, including: Adults Who Forgo Needed Medical Care, Health Insurance Coverage by Type, and Adults with No Personal Doctor. The graphic to the right, featured in one of our analyses using 2018 BRFSS data, explored inequities in health care cost and access based on race/ethnicity and education. In one of our latest publications on the topic of health care cost and affordable health care, researchers analyze Forgone Care by Coverage Type, which revealed that 63% of adults without health coverage reported forgone care while no more than 14% of those with coverage reported forgone care. Find the full analysis here; explore this and other data on State Health Compare.
State and Federal Relief Prevented Deep Backslide in Health Care Affordability in California in 2020
There were well-founded fears that the pandemic, and the concurrent economic crisis, could make health insurance and health care unaffordable for even more people — already a long-standing problem in California. This analysis of the California Health Insurance Survey (CHIS) shows that Californians were largely protected from experiencing a major erosion in their ability to pay for health insurance and care. Despite this overall positive finding, the 2020 CHIS data on health care affordability continue to demonstrate clear inequities by income and race/ethnicity.
Employer-Sponsored Insurance: A National-Level Look at Cost and Coverage Rates

 Throughout the United States, a majority of Americans and their families receive health insurance coverage through their employer. In 2021, the number of individuals enrolled in this type of coverage – known as employer-sponsored insurance or ESI – exceeded 62.2 million. In this blog, infographic, and companion documents, SHADAC researchers use data from the Medical Expenditure Panel Survey-Insurance Component (MEPS-IC) to analyze the private-sector ESI landscape in 2021 on a national level and within the states. We used the following year's data from the same source and compared 2022 vs 2021 in terms of employee access to coverage, health care cost for employees, and more in this blog and accompanying infographic.
Throughout the United States, a majority of Americans and their families receive health insurance coverage through their employer. In 2021, the number of individuals enrolled in this type of coverage – known as employer-sponsored insurance or ESI – exceeded 62.2 million. In this blog, infographic, and companion documents, SHADAC researchers use data from the Medical Expenditure Panel Survey-Insurance Component (MEPS-IC) to analyze the private-sector ESI landscape in 2021 on a national level and within the states. We used the following year's data from the same source and compared 2022 vs 2021 in terms of employee access to coverage, health care cost for employees, and more in this blog and accompanying infographic.Past Work
2018 State-Level Estimates of Medical Out-of-Pocket Spending for Individuals with Employer-Sponsored Insurance Coverage
As part of SHADAC’s work monitoring trends in coverage, access, and affordability, this brief highlights the affordability of coverage for those with employer-sponsored health insurance (ESI). Using data from the Current Population Survey (CPS), SHADAC estimated family out-of-pocket costs for people with employer coverage across all 50 states and the District of Columbia (D.C.). Additional analysis looked at family median out-of-pocket costs by state and estimated the high medical cost burden where family out-of-pocket spending is greater than 10% of household income.
Minnesota Health Care Home Care Coordination Cost Study
The Minnesota Department of Human Services and Health contracted with SHADAC to conduct a study of the costs of Health Care Home care coordination for adults. In order to estimate the cost of care coordination, SHADAC used a case study approach and developed a list of activities (or “ingredients”) that define care coordination and collected information about the costs associated with each of these activities at six non-acute, primary care clinics.