Blog & News
Expert Perspective and Issue Brief: Tracking the Data on Medicaid’s Continuous Coverage Unwinding (State Health & Value Strategies Cross-Post)
January 21, 2022:The following content is cross-posted from State Health and Value Strategies published on January 21, 2022.
Authors: Emily Zylla, Elizabeth Lukanen, and Lindsey Theis, SHADAC
Medicaid and Children’s Health Insurance Plan (CHIP) programs have played a key role in the response to the COVID-19 pandemic, providing a vital source of health coverage for millions of people. However, when the Families First Coronavirus Response Act (FFCRA) Medicaid “continuous coverage” requirement is discontinued states will restart eligibility redeterminations, and millions of Medicaid enrollees will be at risk of losing their coveragei.
A lack of publicly available data on Medicaid enrollment, renewal, and disenrollment makes it difficult to understand exactly who is losing Medicaid coverage and for what reasons. Publishing timely data in an easy-to-digest, visually appealing way would help improve the transparency, accountability, and equity of the Medicaid program. It would inform key stakeholders, including state staff, policymakers, and advocates, allowing them to more fully understand the impacts of Medicaid policy changes on enrollees’ access, and give them an opportunity to modify or implement intervention strategies as needed. States already collect a significant amount of data that could inform their success in enrolling and retaining eligible individuals in Medicaid. Many advocates and researchers have been calling for increased transparency around this data in order to better understand the barriers and challenges individuals face when trying to enroll in or maintain coverage.
One effective way to monitor this dynamic issue is by creating and publishing a Medicaid enrollment and retention dashboard. A typical data dashboard is designed to organize complex data in an easy-to-digest visual format, thus allowing the audience to easily interpret key trends and patterns at a glance. A new issue brief examines the current status of Medicaid enrollment and retention data collection, summarizes potential forthcoming reporting requirements, and describes some of the best practices when developing a data dashboard to display this type of information.
The issue brief lays out a phased set of priority measures and provides a model enrollment and retention dashboard template that states can use to monitor both the short-term impacts of phasing out public health emergency (PHE) protections and continuous coverage requirements, as well as longer-term enrollment and retention trends.
State Medicaid Enrollment and Retention Dashboard – Measurement Priorities
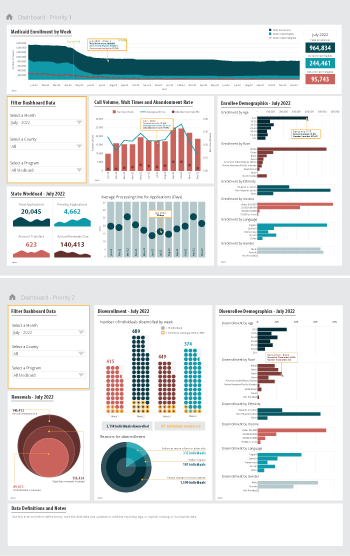 Priority 1 – Use currently reported data: Start with the data that are already collected and submitted to the Centers for Medicare & Medicaid Services (CMS) under the 11 Medicaid performance topics.
Priority 1 – Use currently reported data: Start with the data that are already collected and submitted to the Centers for Medicare & Medicaid Services (CMS) under the 11 Medicaid performance topics.
Priority 2 – Track reasons for disenrollment: Include measures in the proposed Build Back Better Act (BBB) legislative language that address the reasons why people are being disenrolled.
Priority 3 – Monitor coverage transitions: Add measures to address issues of transitions between programs and churn—the moving in and out of coverage—that frequently occurs in Medicaid and CHIP.
Priority 4 – Explore reasons for and consequences of disenrollment: Field disenrollment surveys that could provide quantitative and qualitative data that could be used to understand both the enrollee’s experience navigating Medicaid processes as well as the consequences of disenrollment.
Regardless of the measures highlighted, an overarching goal of any Medicaid enrollment and retention dashboard should be a focus on displaying disaggregated data. Providing data broken down by various population characteristics (e.g., age, race/ethnicity, income, gender, language, or program type) or geographic areas (urban, rural) will make it easier to understand the potentially disproportionate impact of administrative enrollment and renewal policies on communities of color, persons with lower incomes, and other populations that face disparities. Access to this type of granular data provides stakeholders an opportunity to take action in order to minimize needless loss of coverage.
Designing an easy-to-understand dashboard that is accessible to all interested stakeholders—state or county program staff, navigators or enrollment assisters, and advocates—will highlight the early warning signs of large numbers of people losing Medicaid coverage. States should start small, using data dashboard best practices and as they gain experience publicly reporting this data, consider adding additional measures over time.
i Buettgens, M. & Green, A. (September 2021). What Will Happen to Unprecedented High Medicaid Enrollment after the Public Health Emergency? [Research report]. Urban Institute. https://www.urban.org/sites/default/files/publication/104785/what-will-happen-to-unprecedented-high-medicaid-enrollment-after-the-public-health-emergency_0.pd









