Blog & News
2020 U.S. alcohol-involved deaths climbed by 26.6%, and drug overdose deaths by 30.6%
February 16, 2022:Size of alcohol, drug overdose death increases in first pandemic year were unparalleled
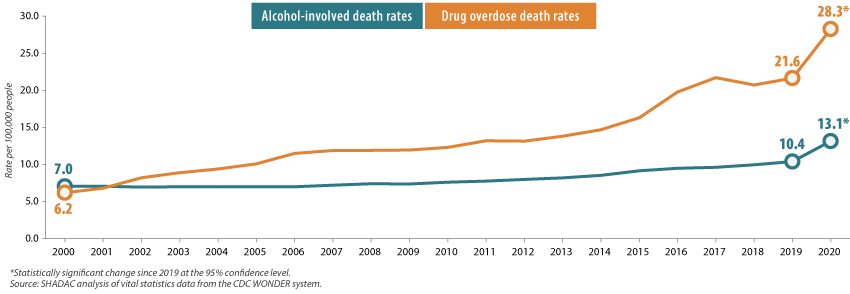
With the recent release of 2020 mortality data from the U.S. Centers for Disease Control and Prevention (CDC), we now know that fears that the pandemic could result in increased drug and alcohol deaths were well-founded. In just a single year, the U.S. alcohol-involved death rate increased 26.6%, and drug overdose deaths grew by 30.6% (Figure 1).
Figure 1. U.S. alcohol-involved and drug overdose death rates, 2000-2020
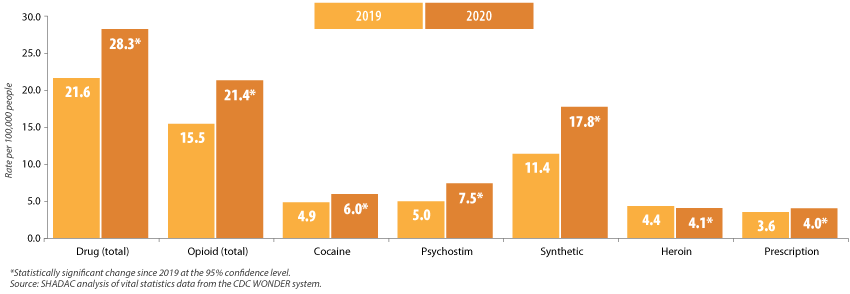
Overdose death rates increased significantly across most drug types (declining only for heroin), and they were led by a 55.6% increase in deaths from fentanyl and similar synthetic opioids, and a 48.2% increase in deaths from methamphetamine and other psychostimulant drugs (Figure 2).
Figure 2. Changes in U.S. drug overdose death rates by type, 2019-2020
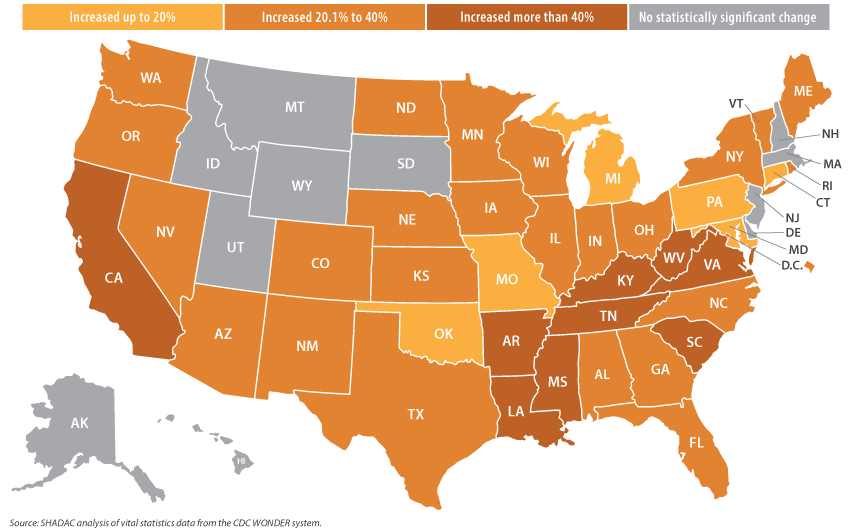
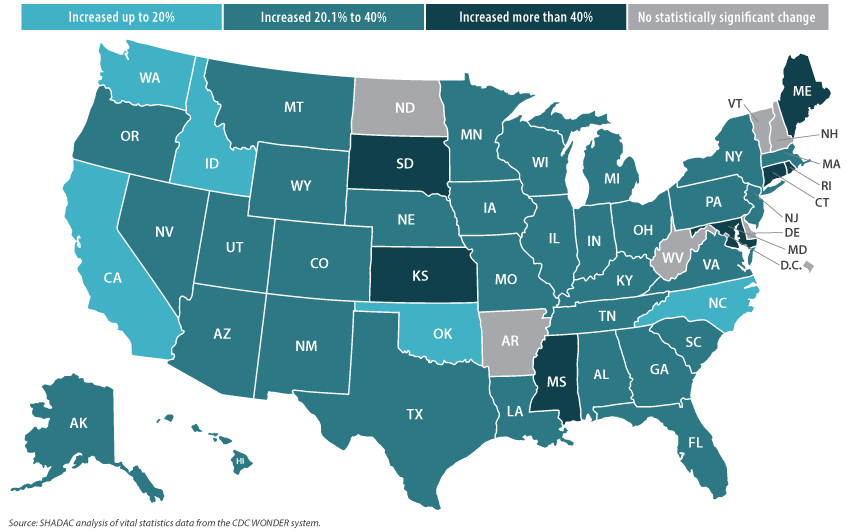
The story was similarly grim across the states. From 2019 to 2020, forty states experienced statistically significant increases in their drug overdose death rates. Those ranged from the smallest increase of 12.9 percent in Connecticut (from 34.7 deaths per 100,000 people in 2019 to 39.1 in 2020) to the largest increase of 54.8 percent in Mississippi (from 13.6 deaths per 100,000 people in 2019 to 21.2 in 2020) (Figure 3).
Figure 3. Statistically significant state-level increases in drug overdose death rates, 2019-2020
During the same period, 44 states recorded statistically significant increases in their rates of alcohol-involved deaths, ranging from the smallest increase of 15.2 percent in Oklahoma (15.1 deaths per 100,00 people in 2019 to 17.4 in 2020) to the largest increase of 67.2 percent in Mississippi (7.0 deaths per 100,00 people in 2019 to 11.8 in 2020) (Figure 4).
Figure 4. Statistically significant state-level increases in alcohol-involved death rates, 2019-2020
While these increases in alcohol-involved and drug overdose death rates follow patterns a decade or more in the making, the twin crises of high-risk substance use clearly reached a crescendo during the pandemic, as evidenced by the unparalleled heights of substance-related death rates reported in recent decades.1,2 And though data for 2021 are not yet fully available, provisional reports indicate that drug overdose deaths continued at historically elevated levels.3 Mortality data clearly show that the fallout of the pandemic has included the exacerbation of dangerous drug and alcohol use patterns in the U.S., and it is an issue that deserves redoubled focus as the COVID-19 emergency eventually begins to ebb.
The U.S. and state-level data analyzed in this blog post are all available on SHADAC’s State Health Compare data website: http://statehealthcompare.shadac.org/.
1 Planalp, C., Au-Yueng, C.M., & Winkelman, T.N.A. (April 2021). Escalating Alcohol-Involved Death Rates: Trends and Variation Across the Nation and in the States from 2006 to 2019. State Health Access Data Assistance Center (SHADAC). https://www.shadac.org/sites/default/files/publications/Alcohol-Involved-Deaths/AID-4.21-SHADAC-Brief.pdf
2 Planalp, C. & Hest, R. (August 2020). Overdose Crisis in Transition: Changing National Trends in a Widening Drug Death Epidemic. State Health Access Data Assistance Center (SHADAC). https://www.shadac.org/sites/default/files/publications/2020%20NATIONAL_SHADAC_Opioidbrief.pdf
3 Ahmad, F.B., Rossen, L.M., & Sutton, P. (2022, January 12). Provisional drug overdose death counts. National Center for Health Statistics (NCHS). https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
Blog & News
Brief: Strategies to Increase Access to Medications for Opioid Use Disorder during the COVID-19 Pandemic and Beyond
October 25, 2021: Impacts of the COVID-19 pandemic have been demonstrably far-ranging, including changes to substance use-related behaviors.1 Evidence indicates that opioid use disorders (OUDs), overdoses, and overdose deaths grew as a result of COVID-19-related isolation and economic anxiety, and mortality data indicate that opioid overdose deaths, in particular, reached record levels in 2020.
Impacts of the COVID-19 pandemic have been demonstrably far-ranging, including changes to substance use-related behaviors.1 Evidence indicates that opioid use disorders (OUDs), overdoses, and overdose deaths grew as a result of COVID-19-related isolation and economic anxiety, and mortality data indicate that opioid overdose deaths, in particular, reached record levels in 2020.
SHADAC researchers Carrie Au-Yeung and Lynn Blewett, along with Hennepin Healthcare researcher Tyler Winkelman, authored a new Milbank Foundation policy brief that examines the federal and state policies changes put in place to improve access to medications for opioid use disorder (MOUD) during the COVID-19 pandemic, during which time MOUD became especially challenging to access because MOUD patients are typically required to have as many as six in-person clinic visits a week. The authors conclude with federal and state policy recommendations based on their analysis.
What is MOUD?
MOUD – sometimes referred to as medication-assisted treatment, or MAT – is the use of medications (methadone, buprenorphine, and naltrexone) to treat OUD, reduce opioid use, and lower the risk of overdose mortality. MOUD is frequently coupled with counseling and behavioral therapies and is the standard of care for OUD.
What policy solutions were put into place to make MOUD more accessible during COVID-19?
A number of policy solutions were put into place at the federal and state level in order to reduce the number of in-person clinic visits required for MOUD and to make MOUD more accessible in general. These solutions involved service delivery rules, prescribing rules, dispensing and refill rules, drug-testing requirements, counseling requirements, Medicaid prior authorization rules, and Medicaid coverage of telehealth.
For example, at the state level:
- Telehealth visits were allowed to replace in-person MOUD visits around prescriptions, assessments, and counseling.
- Some states loosened restrictions on dispensing and refill rules for MOUD and also allowed opioid treatment programs (OTPs) to deliver medications to quarantined or otherwise homebound patients.
- Some states gave more latitude to practitioners to use their own clinical judgment regarding toxicology screening and drug testing, and relaxed state-level counseling requirements or suspending them altogether.
- Individual states temporarily suspended certain Medicaid prior authorization requirements for MOUD, extended prior authorizations through the end of the COVID-19 emergency period, and/or expedited prior authorizations through documentation flexibility.
- All 50 states and the District of Columbia (D.C.) modified Medicaid policies regarding telehealth to allow for more virtual visits: some upped payment rates for telehealth visits to match in-person visits, others extended policies to cover a wider array of providers, and others expanded “telehealth” to cover audio-only (telephonic) visits.
At the federal level, policy solutions included:
- In-person examination requirements for buprenorphine initiation were removed while for methadone, initiation must be in person, but subsequent visits can occur via telemedicine.
- In April 2021, the US Department of Health and Human Services altered prescribing rules to exempt eligible physicians and practitioners from federal training requirements to obtain a waiver to prescribe buprenorphine small numbers of patients (i.e., fewer than 30).
- Dispensing and refill rules, such as the standard take-home schedule for methadone, was relaxed by the Substance Abuse and Mental Health Services Administration (SAMHSA).
- The American Society for Addiction Medicine suggested pausing, limiting, or using alternative protocols for drug-testing requirements in certain areas to combat community spread of COVID-19.
Recommendation
The need to expand access to MOUD will not end with the COVID-19 emergency, as the number of individuals who need treatment far exceeds the capacity of MOUD providers and facilities. Some of the policy changes that have made MOUD more accessible during the pandemic have already been made permanent at the state level (e.g., expanding the definition of “telehealth” in Medicaid). The continuation of other changes, however, will require ongoing support from state and national policymakers.
The authors recommend continued efforts around three regulatory strategies in particular:
- National and state policymakers should encourage the continuation of federal policies allowing buprenorphine initiation via telemedicine and the removal of state-level restrictions that go beyond federal requirements.
- National and state policymakers should also promote the continuation of federal policies allowing OTPs to dispense more doses of methadone and the removal of any additional state-level methadone dispensing restrictions that exist.
- Policymakers should work to prohibit Medicaid prior authorization requirements for MOUD and to make permanent any temporary suspensions of prior authorization requirements for these medications that were implemented during the COVID-19 emergency.
The authors note that, though there are other policy avenues for expanding access to MOUD, these three areas are particularly relevant for reducing logistical barriers to treatment. Moreover, evidence and testimony from providers and patients indicates that these mechanisms have been safe and effective during the COVID-19 pandemic and that continuing them beyond the pandemic period is warranted.
1 Planalp, C. (2021, July 15). Drug overdose deaths grew by almost 30 percent in 2020. SHADAC blog. https://www.shadac.org/news/drug-overdose-deaths-grew-almost-30-percent-2020
Planalp, C. (2021, June 14). Pandemic drinking may exacerbate upward-trending alcohol deaths. SHADAC blog. https://www.shadac.org/news/pandemic-drinking
Blog & News
(Webinar) U.S. Health On the Rocks: The Quiet Threat of Growing Alcohol Deaths
August 01, 2024:Date: Tuesday, September 21st
Time: 3:00 PM Central / 4:00 PM Eastern
While much public attention has been given to the opioid epidemic, the United States has been quietly experiencing another growing public health crisis that surpasses opioid overdoses as a cause of substance abuse-related deaths in nearly half of all states: alcohol-involved deaths.
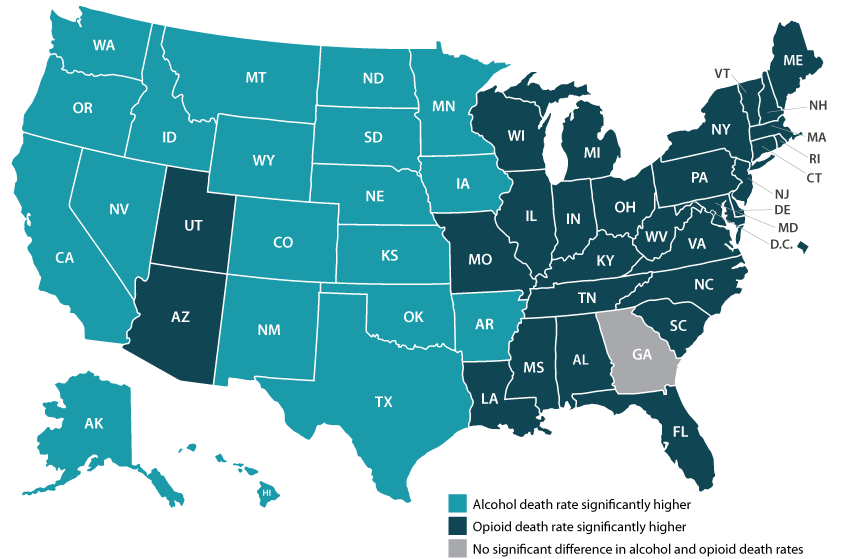
Using data from a recent analysis of alcohol-involved deaths from 2006 to 2019, SHADAC will host a webinar on Tuesday, September 21st detailing the trends in rising alcohol-involved deaths across the U.S., among the states, and for certain demographic groups.
Speakers
Carrie Au-Yeung, MPH, SHADAC – Ms. Au-Yeung will speak about variation in alcohol-related death rates across the states, as well as provide comparisons to opioid-related death rates in order to better understand the scale and context of substance use issues among the states.
Colin Planalp, MPA, SHADAC – Mr. Planalp will talk about national-level increases in alcohol death rates as well as rising rates for demographic groups by race and ethnicity, age, gender and urbanization.
Tyler Winkelman, MD, MSc, Hennepin Healthcare – Dr. Winkelman will discuss how the data serve can help us understand the impacts of the pandemic on alcohol-involved disease and deaths as well as the case for expanding our response to substance use issues beyond opioids.
A question and answer session will be open for all attendees following the webinar presentation. Attendees are encouraged to submit questions for any or all of the speakers prior to the webinar, and can do so here.
Slides from the webinar are available for download.
Resources
Escalating Alcohol-Involved Death Rates: Trends and Variation across the Nation and in the States from 2006 to 2019 (Infographics)
U.S. Alcohol-Related Deaths Grew Nearly 50% in Two Decades: SHADAC Briefs Examine the Numbers among Subgroups and States (Blog)
Pandemic drinking may exacerbate upward-trending alcohol deaths (Blog)
BRFSS Spotlight Series: Adult Binge Drinking Rates in the United States (Infographic)
Blog & News
New SHADAC Brief Looks at Changes in Federal Surveys During COVID Pandemic
August 27, 2021: The impacts of the coronavirus pandemic have been far ranging—on education, work, healthcare, and almost every other aspect of daily life. However, another effect of COVID that is just now coming to light is the interruption of data collection processes and falling response rates for yearly federal surveys that, among other measures, provide estimates of health insurance coverage for the United States population. Such surveys would, under normal circumstances, be ideally suited to measure changes to insurance coverage during such a tumultuous time.
The impacts of the coronavirus pandemic have been far ranging—on education, work, healthcare, and almost every other aspect of daily life. However, another effect of COVID that is just now coming to light is the interruption of data collection processes and falling response rates for yearly federal surveys that, among other measures, provide estimates of health insurance coverage for the United States population. Such surveys would, under normal circumstances, be ideally suited to measure changes to insurance coverage during such a tumultuous time.
In a new brief, SHADAC summarizes COVID-era changes and challenges for four major federal surveys—the American Community Survey (ACS), the Current Population Survey (CPS), the Medical Expenditure Panel Survey (MEPS), and the National Health Interview Survey (NHIS)—such as shifting in-person collection methods to phone and email, adding COVID-related questions to questionnaires, extending survey fielding in order to address falling response rates, and delayed data release dates, among others.
All four surveys made significant changes to their Survey Operations:
In-person: The ACS, CPS, and NHIS all suspended in-person operations from March to June 2020, with limited in-person interviews resuming in either July or September 2020. The MEPS Insurance Component (MEPS-IC) suspended in-person interviews entirely.
Mailing: Mailing centers for the ACS and the CPS were shut down in March 2020, but re-opened with limited staffing in July 2020, allowing previously completed surveys to be collected and counted. The MEPS Household Component (MEPS-HC) shifted to dual web-and-mailing collection methods in the fall of 2020 while the MEPS-IC shifted to dual web-and-phone data collection at that time.
Telephone: All surveys (ACS, CPS, MEPS-HC and MEPS-IC, and NHIS) shifted to phone-only surveys while in-person fielding was shut down, or while mailing operations were suspended, in the case of the MEPS-IC.
Web: While both the MEPS-HC and MEPS-IC took a different direction and shifted to telephone-only survey collection in March 2020, the former proposed a shift to dual web-and-mailing data collection modes while the latter opted to shift to dual web-and-phone methods in the fall of 2020.
Three surveys made changes to their Questionnaires:
The ACS and the MEPS-IC opted not make any changes to their questionnaires in response to COVID-19.
The CPS added five new questions regarding COVID’s impact on employment to the questionnaire. The NHIS similarly added new questions to its survey form, but instead asked respondents about COVID testing, contraction and symptoms, and prevention measures.
The MEPS-HC was the only survey to create an entirely new questionnaire: the “Social and Health Experiences” survey, which asked respondents about changes or delays in care due to COVID.
Each survey experienced falling Response Rates:
Where they were able to be measured, survey response rates dropped significantly. Neither the MEPS-HC nor the NHIS has yet released response rates for 2020, but previous years show a drop in response rates for the latter survey of 20 percentage points (80 percent in 2018 to 60 percent in 2019). Both the ACS and CPS saw falling response rates between 2019 and 2020. The ACS dropped 15 percentage points (86 percent in 2019 to 71 percent in 2020), while the CPS fell by roughly 6 percentage points (67.6 percent in 2019 to 61.1 percent in 2020). The MEPS-IC saw a smaller decrease between the years, from 59.6 percent in 2019 to 56.1 percent in 2020.
SHADAC plans to continue monitoring reported changes to these and other federal surveys in 2020, and continuing into 2021 where applicable. As data from 2020 becomes available, our researchers will continue to produce resources to explain what effects these adaptations may have for understanding the data, and if alternative sources may provide ways to fill in gaps where 2020 data may be incomplete or unable to be reliably used.
Blog & News
Drug overdose deaths grew by almost 30 percent in 2020
July 15, 2021:Fentanyl- and methamphetamine-type drugs surged roughly 50 percent in 2020
Drug overdose deaths surged in the United States during the first year of the COVID-19 pandemic, increasing nearly 30 percent in just 12 months. Provisional data recently published by the U.S. Centers for Disease Control and Prevention (CDC) show that more than 92,000 people died of drug overdoses in 2020—surpassing records yet again.1
The growth was widespread throughout the country, with only two states (New Hampshire and South Dakota) spared from the jump in drug overdose deaths. Conversely, some states saw their death rates increase more than 50 percent, including Kentucky, South Carolina, Vermont, and West Virginia.
Much of the growth in drug overdose deaths was driven by synthetic opioids such as fentanyl, which increased more than 50 percent from 2019 to 2020 (see Figure 1). Fentanyl has become a key product for international drug traffickers, often finding its way as an adulterant in other drugs like heroin and cocaine, and even as an ingredient in counterfeits of common opioid prescription pills such as Oxycontin. The emergence of fentanyl in the U.S. illicit drug trade is a newer phenomenon beginning in the past decade, and it has recently spread from eastern states to increasingly affect states in the western half of the country as well.
Figure 1. Changes in drug overdose deaths in the U.S., 2019 to 2020
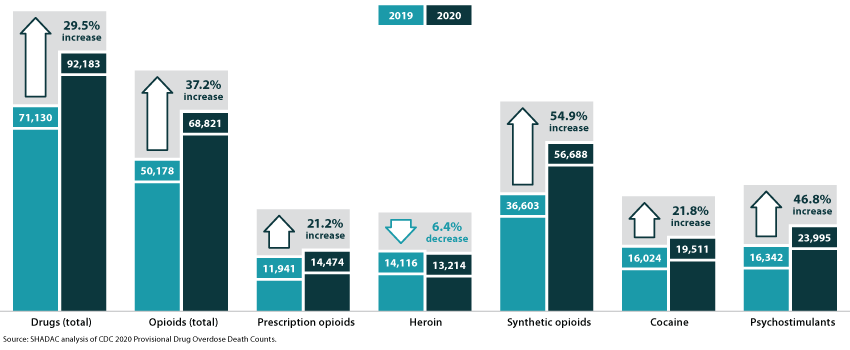
A family of drugs called “psychostimulants”—mostly methamphetamine—also drove a large increase in deaths in 2020, up nearly 50 percent since 2019. Deaths involving methamphetamine and other psychostimulants have grown dramatically in the past few years. The increased death toll involving psychostimulants is likely caused by two factors: First, the methamphetamine trafficked in the U.S. today is generally much more potent than methamphetamine sold in the past, raising the potential risk of overdoses caused by methamphetamine. Second, methamphetamine today is often contaminated with, or used alongside, synthetic opioids, raising the risk of an overdose involving the use of multiple drugs simultaneously.
Of the main drugs involved in overdoses2, only heroin was associated with a decline in deaths during 2020—falling by less than 10 percent since 2019. Meanwhile, overdose deaths involving prescription opioids increased more than 20 percent, reversing a trend of relatively stable or even declining death rates over several years. Cocaine overdose deaths similarly increased by more than 20 percent in 2020.
1 National Center for Health Statistics (NCHS). (2021, July 14). Vital Statistics Rapid Release: Provisional Drug Overdose Death Counts [Data set]. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
2 The drug overdose death categories presented in the CDC data include: heroin, natural opioid analgesics (e.g., morphine and codeine) and semisynthetic opioids (e.g., oxycodone and hydrocodone), synthetic opioids such as methadone and synthetic opioids other than methadone (e.g., fentanyl and tramadol), cocaine, and psychostimulants.
Pages
- « first
- ‹ previous
- 1
- 2
- 3