Blog & News
Examining Gender-Based Discrimination in Health Care Access by Gender Identity in Minnesota
December 9, 2022:Authors: Jeremy Duval, Natalie Mac Arthur, Kathleen Call
DefinitionsCisgender/cis: A person whose gender identity corresponds with their sex assigned at birth. Transgender/trans: A person whose gender identity differs from their sex assigned at birth. Non-binary: An umbrella term for a person whose gender identity is not binary (male or female). |
Introduction
Many barriers exist to creating an equitable health care experience for LGBTQ+ individuals. One critical barrier is gender-based discrimination from providers within health care systems. The biennial 2021 Minnesota Health Access Survey (MNHA) asked respondents how often their gender, sexual orientation, gender identity, or gender expression causes health care providers to treat them unfairly. We compared rates of gender-based discrimination and health care access in the Minnesota adult population and examined differences in access to care among cisgender (cis) and gender minorities who report gender-based discrimination (see Definition Box). We explored the impact of gender-based discrimination on health care access by comparing access rates among people who did and did not experience discrimination for cis men, cis women, transgender and non-binary populations in Minnesota.
Results
The majority (58.9%) of transgender (trans) and non-binary respondents reported experiencing gender-based discrimination from health care providers in 2021—a stark contrast from the statewide average of 6.0% (Figure 1). Cis women also reported gender-based discrimination (7.7%) above the population average, while cis men were less likely to experience this form of discrimination (2.9%). Gender-based discrimination was especially high for both non-binary (63.9%) and trans (48.8%) respondents. Due to sample size limitations, these populations were combined in the remainder of our analyses.
Figure 1. Unfair treatment from health care providers based on gender in Minnesota
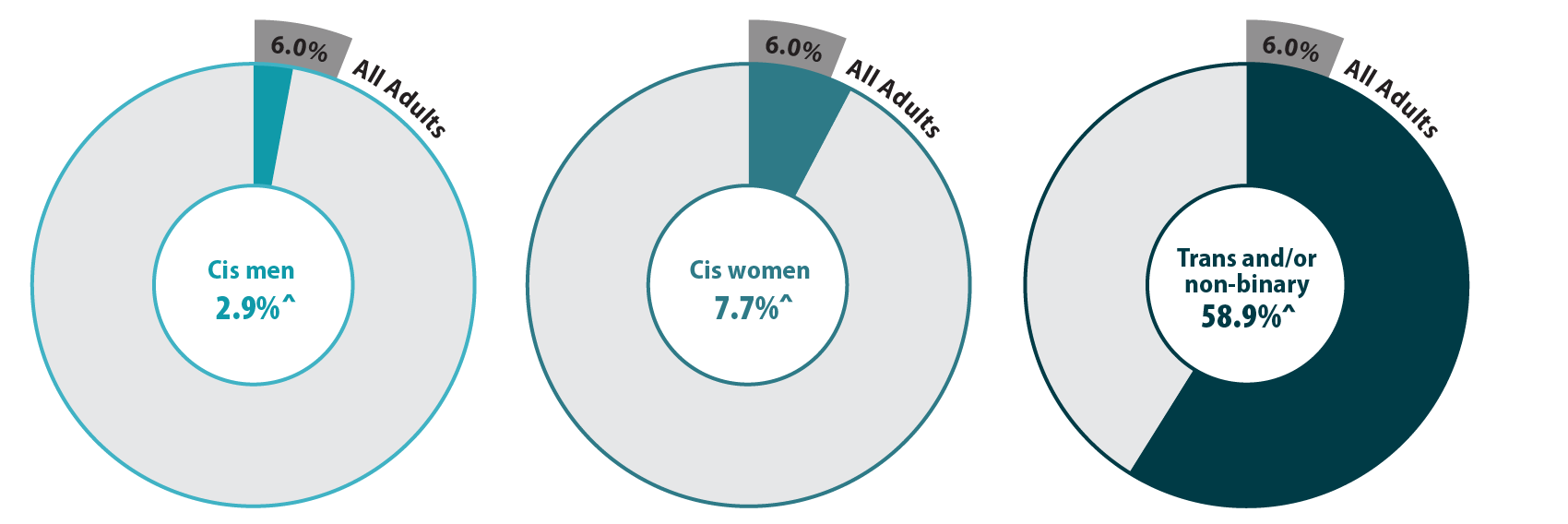
^ Rate significantly different from All Adults at the 95% confidence level.
Source: SHADAC analysis of the 2021 Minnesota Health Access Survey.
We also found differences in health care access among trans and non-binary people compared with the adult Minnesota population, particularly for confidence in getting care and forgoing needed care due to cost (Figure 2). We found that trans and non-binary respondents were similar to cis men in rates of having a usual source of care and having a medical visit (non-emergency) in the past year. Compared with the adult population in Minnesota, cis men were more likely to lack these forms of care, while cis women had better access to regular medical visits and a usual source of care. However, differences from the state average did not reach significance for trans and non-binary respondents, likely due to small sample size. Nearly a third (30.1%) of trans and non-binary adults had low confidence in getting necessary care compared to an average of 11.8% for adults in Minnesota. Over half (57.1%) of trans and non-binary people reported forgone care—more than double the average (26.2%).
Figure 2. Health care use and barriers to care
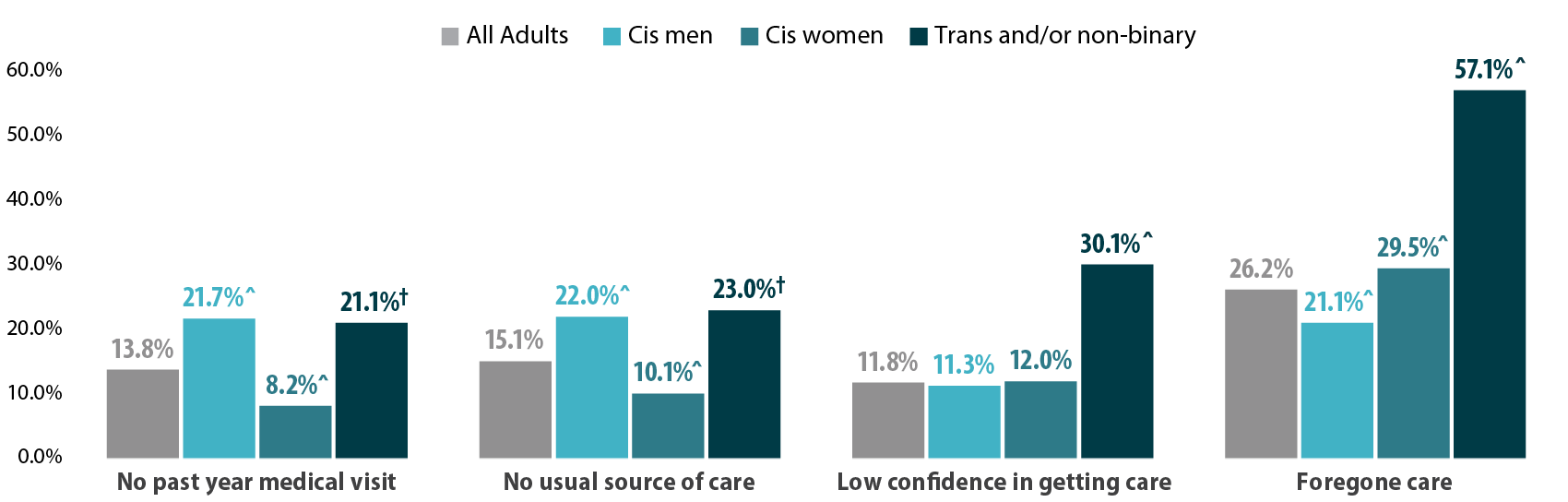
^ Rate significantly different from All Adults at the 95% confidence level.
† Estimate may be unreliable due to limited data (relative standard error greater than or equal to 30%).
Source: SHADAC analysis of the 2021 Minnesota Health Access Survey.
Figure 3. Experiences of gender-based discrimination associated with barriers to health care access
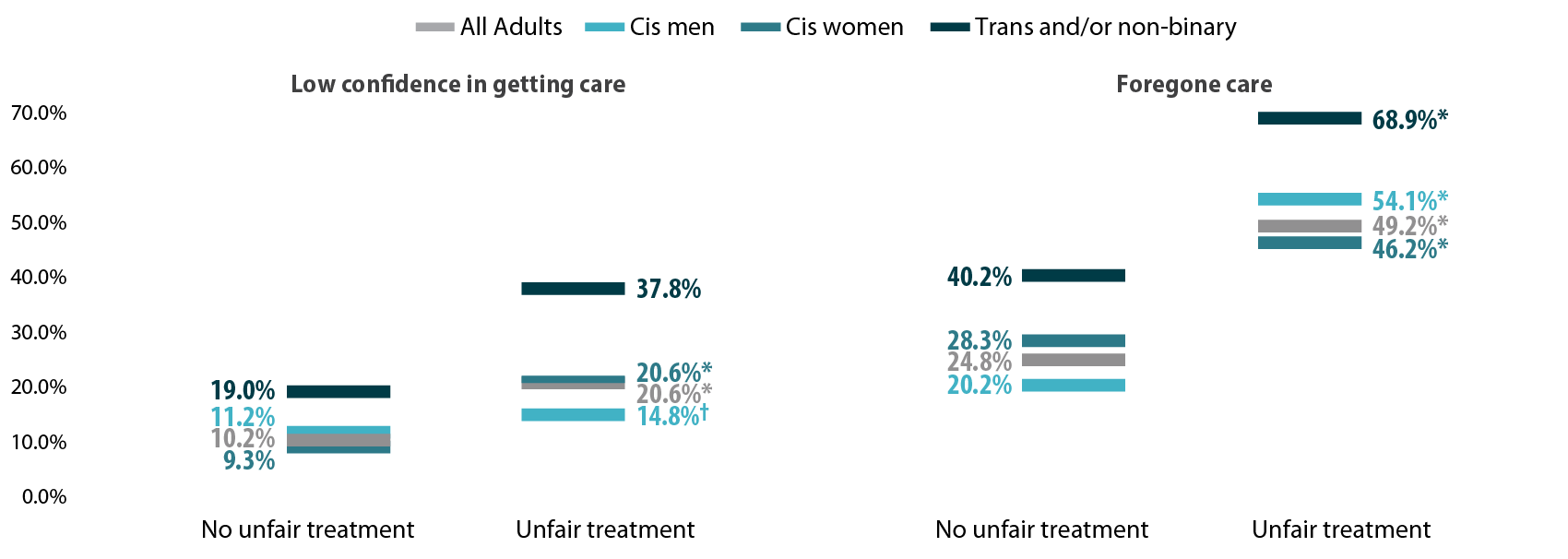
* Significant difference within a given subpopulation between rates of people who experienced unfair treatment and those who did not.
† Estimate may be unreliable due to limited data (relative standard error greater than or equal to 30%).
Source: SHADAC analysis of the 2021 Minnesota Health Access Survey.
Discussion
A worryingly high proportion of trans and non-binary adults reported gender-based discrimination and had forgone care or did not have confidence in getting needed care. This lack of confidence could be in part due to experienced or anticipated discrimination within a health care setting. Barriers to care were especially high among those who had experienced gender-based discrimination, which suggests that discrimination has a serious negative impact on health care access for trans and non-binary people.
We found higher rates of gender-based discrimination (58.9%) among trans and non-binary adults in Minnesota in 2021 compared to previously published literature on gender-based discrimination. National data indicate that between 20% and 40% of LGBTQ+ Americans experience discrimination while accessing health services (Kattari & Hasche, 2016), (Kachen & Pharr, 2020), (Penrose et al, 2020), (Rodriguez, Agardh & Asamoah, 2018), (Shires & Jaffee, 2015). Additionally, over 20% of the LGBTQ+ population avoided seeking health care due to anticipated discrimination (Kcomt et al, 2020). Notably, the majority of previously published estimates of trans peoples’ experiences of health care discrimination come from the National Transgender Discrimination Survey, which was conducted in 2016 and provides rich data, but for a specialized and non-probability sample. Such data are not considered generalizable. A strength of the MNHA survey is that it measures discrimination using a probability sample of adults reporting their gender identity.
Gender-based discrimination is just one factor affecting health care access. Gender minorities may additionally face disproportionate rates of other key barriers to access, such as lack of insurance coverage (Gonzales & Henning-Smith, 2017). Regardless, we found large gaps in health care access for trans people, non-binary people, and all people who experienced gender-based discrimination.
Conclusion
When the majority of a population is experiencing discrimination within health care systems, it is clear that change is necessary. Our data, based on a probability sample of Minnesotans, helps address gaps in knowledge about barriers transgender and non-binary adults face in accessing health care. The high rates of gender-based discrimination among gender minorities illustrate that gender-inclusive data collection is important for health equity.
However, quantifying rates of discrimination only scratches the surface of the true problem. Because of the limited sample size of gender minority adults, we were unable to explore the role of other social factors in gender-based discrimination and health care barriers by gender identity. Race, ethnicity, and class likely intersect to exacerbate experiences of discrimination and barriers to care for gender minorities. For example, Black and American Indian/Alaskan Native transgender women face disproportionate rates of victimization, and these experiences may impact their health care needs and intensify barriers to accessing care (Reisner, 2018). In this analysis, we only looked at gender identity; our future studies will look at sexual orientation with a similar lens and examine these two together.
One of the largest barriers to understanding discrimination and its effects on health access is data collection. Not all surveys collect and report inclusive data on gender identity, which makes it very hard to track access for trans and non-binary people. Even when gender-inclusive data are available, gender-based discrimination is rarely measured. Direct measurement of discrimination is essential for monitoring rates of discrimination in health care settings and associated barriers to care (Lett et al., 2022).
In Minnesota, state-level policies make this type of measurement possible. Historically, Minnesota has strong anti-discrimination laws in place to protect gender-diverse individuals. For example, Minnesota was one of the first states to allow an “X” option for gender on licenses (Walsh, 2018). Yet, we found alarmingly high reports of gender-based discrimination in health care among gender minorities in this state. The level of gender-based discrimination may be even higher in other states with less inclusive policies. Consequently, our results suggest that on a national level, gender-based discrimination in health care may affect a substantial number of Americans.
Understanding the full scope of gender-based discrimination in Minnesota and across the U.S. should be a priority in future research to support health equity. Our data contributes to the base of knowledge regarding gender-based discrimination in health care and its correlation with issues of health care access. Our findings highlight the need for more expansive research and policy changes in these areas.
Methods
Data are from the 2021 Minnesota Health Access (MNHA) survey, which is a biennial population-based survey on health insurance coverage and access conducted in collaboration with the Minnesota Department of Health. We limited the analysis to adults responding for themselves about experiences of discrimination and access (n=10,003); we excluded proxy reports (e.g., a household member answering for a spouse or roommate). Tests for statistical significance were conducted at the 95% confidence level.
Check out our companion blog "Examining Discrimination and Health Care Access by Sexual Orientation in Minnesota".
References
Gonzales, G., & Henning-Smith, C. (2017). Barriers to Care Among Transgender and Gender Nonconforming Adults. The Milbank quarterly, 95(4), 726–748. https://doi.org/10.1111/1468-0009.12297
Kachen, A., & Pharr, J. R. (2020). Health Care Access and Utilization by Transgender Populations: A United States Transgender Survey Study. Transgender health, 5(3), 141–148. https://doi.org/10.1089/trgh.2020.0017
Kattari, S. K., & Hasche, L. (2016). Differences Across Age Groups in Transgender and Gender Non-Conforming People's Experiences of Health Care Discrimination, Harassment, and Victimization. Journal of aging and health, 28(2), 285–306. https://doi.org/10.1177/0898264315590228
Lett E., Asabor E., Beltrán S., Cannon A.M., Arah O.A. (2022). Conceptualizing, Contextualizing, and Operationalizing Race in Quantitative Health Sciences Research. Ann Fam Med 20(2):157-163. https://doi.org/10.1370/afm.2792
Movement Advancement Project. "Equality Maps: Housing Nondiscrimination Laws." https://www.lgbtmap.org/equality-maps/non_discrimination_laws/housing. Accessed 11/07/2022.
Reisner, S. L., Bailey, Z., & Sevelius, J. (2014). Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the US. Women & health, 54(8), 750-767.
Shires, D. A., & Jaffee, K. (2015). Factors associated with health care discrimination experiences among a national sample of female-to-male transgender individuals. Health & social work, 40(2), 134–141. https://doi.org/10.1093/hsw/hlv025
Walsh, P. (2018, October 3). Minnesota Now Offers 'X' for Gender Option on Driver's Licenses. Star Tribune. Retrieved November 9, 2022, from https://www.startribune.com/minnesota-now-offers-x-for-gender-option-on-driver-s-licenses/494909961/.
Publication
Minnesota Health Access Survey 2019 Technical Report
 This report describes the data collection process and methodology behind the Minnesota Health Access Survey (MNHA), emphasizing the most recent administration of the survey completed in 2019. The 2019 MNHA represents a break in series, involving for the first time the blending of two sample frames: the introduction of an address based frame and retention of a smaller dual landline/cell telephone frame used in all past MNHA surveys. This report describes this decision and the upshot for other aspects of the methodology.
This report describes the data collection process and methodology behind the Minnesota Health Access Survey (MNHA), emphasizing the most recent administration of the survey completed in 2019. The 2019 MNHA represents a break in series, involving for the first time the blending of two sample frames: the introduction of an address based frame and retention of a smaller dual landline/cell telephone frame used in all past MNHA surveys. This report describes this decision and the upshot for other aspects of the methodology.
Overview of MNHA
The Minnesota Health Access Survey (MNHA) is a biennial survey of non-institutionalized Minnesota residents. The survey collects detailed information on health insurance coverage options, access to coverage and health care services, and basic demographic data. The goal of the survey is to document trends in health insurance coverage, and access to insurance and health care at the state and regional level, as well as for select subpopulations (e.g., rural, low-income families, populations of color and American Indians). The MNHA represents a partnership between the Minnesota Department of Health (MDH) Health Economics Program and the University of Minnesota’s State Health Access Data Assistance Center (SHADAC).
The MNHA data play an important role in monitoring trends in health insurance coverage, evaluating and informing health policy development in Minnesota on topics such as affordability of coverage, access to healthcare, and redesign of public program coverage. The MNHA provides precise and timely estimates on a range of coverage and access relevant questions, is adaptable and responsive to developing state health policy issues, and ensures the availability of micro-data for time sensitive research and policy analysis.
The MNHA has been conducted a number of times over the years: in 1990, 1995, 1999, 2001, 2004, and every two years beginning in 2007.1 This technical report focuses primarily on the 2019 MNHA, providing some cumulative data in table form.2
1 Beginning in 2007, MNHA funding is from a legislative appropriation to the Minnesota Department of Health and additional support from the Minnesota Department of Human Services since 2011.
2 For information about earlier versions of the MNHA contact Kathleen Thiede Call at callx001@umn.edu and the Health Economics Program at health.mnha@state.mn.us.
Blog & News
Minnesota Health Access Survey (MNHA) Data Show Minimal Impact from COVID Pandemic on 2020 Insurance Coverage
March 9th, 2021:A new report released by the Minnesota Department of Health (MDH) shows that Minnesota’s uninsured rate for the first half of 2020—as well as the first known period of the coronavirus pandemic—was relatively unchanged from the fall of 2019, at 4.6% and 4.7%, respectively. The report uses data from the biennial Minnesota Health Access Survey (MNHA), conducted collaboratively between the Minnesota Department of Health (MDH) and the State Health Access Data Assistance Center (SHADAC), to examine changes in health insurance coverage across the state from 2017 to 2019, as well as preliminary coverage estimates from 2020 to measure changes to the insurance landscapr from fall 2019 to spring and summer of 2020.
Pre-Pandemic Coverage Conditions
Prior to the COVID-19 pandemic, the state of Minnesota was enjoying historic levels of health insurance coverage among the overall population. From 2017, the last time the MNHA Survey was conducted, statewide coverage grew significantly to 95.3% in 2019, propelled by gains in employer-sponsored insurance coverage (51.9% in 2017 to 53.6% in 2019), relatively unchanging numbers of public health insurance coverage enrollment, and stabilization of the individual market.
Impacts on Health Insurance Coverage, 2019 to 2020
Using data from the 2019 Minnesota Health Access Survey and the 2020 Health Insurance Enrollment Survey, the report looks at the changes wrought by the COVID-19 pandemic on the insurance coverage landscape from October 2019 to April 2020 and October 2019 to July 2020.
From October 2019…
- …the number of uninsured individuals increased by 600 people in April 2020 and 5,800 people in July 2020.
- …enrollment in public coverage increased by 16,000 individuals in April 2020 and 60,500 individuals in July 2020.
- …enrollment in private insurance fell for both group (i.e., employer-sponsored) coverage—14,400 by April 2020 and 40,100 by July 2020—and individual coverage—15,600 by April 2020 and 13,000 by July 2020.
Health Insurance Coverage Costs, 2017 to 2019
Regardless of the pandemic, a frequently cited issue among Minnesotans with health insurance coverage was the high cost of care, which led to issues of both foregone care as well as reports of trouble paying medical bills, or trouble paying other basic bills (food, housing, etc.) due to high medical bills.
Estimates from the MNHA survey revealed that:
- 25.0% of Minnesotans overall reported having to forgo needed health care due to cost (up from 21.1% in 2017)
- 27.1% of Minnesotans with public insurance reported having to forgo needed health care due to cost (up from 23.7% in 2017)
- 21.0% of Minnesotans with group coverage reported having to forgo needed health care due to cost (up from 16.5% in 2017)
Estimates from the MNHA survey revealed that when it came to experiencing financial burden due to medical bills:
- 22.0% of Minnesotans overall reported experiencing high medical burden (up from 19.8% in 2017)
- 22.5% of Minnesotans with group coverage reported experiencing high medical burden (up from 19.9% in 2017)
Read the full brief detailing these findings, from SHADAC and the Minnesota Department of Health’s Health Economics Program.
SHADAC Expertise
State Survey Research Activity
As part of our core activities, SHADAC tracks state-level data collection and research about health care coverage and access, including quantitative statewide population surveys. In addition to providing information about data collection years and links to these state surveys, we also provide links to websites and reports that show how states use this data.
The table below displays the years in which states conducted household and employer surveys relating to health care coverage and access. Hover over the marks for a high-level state summary of survey activity, or click the marks to access a list of available survey instruments, reports, and technical documentation conducted at the state level since 2010.
SHADAC also maintains an archive of state-level data collection for the years between 2000 and 2010. This archive includes household surveys, employer surveys, enrollee surveys, and focus groups relating to health care coverage and access. Please contact us with any inquiries about state surveys conducted prior to 2010.
NOTE: SHADAC periodically updates this page as new documents become available, so make sure to check back for the latest information. Last update: Summer 2023