Blog & News
Employer-Sponsored Insurance (2019-2021): A National-Level Look at Cost and Coverage Rates (Infographic)
August 30, 2022:Throughout the United States, a majority of Americans and their families receive health insurance coverage through their employer. In 2021, the number of individuals enrolled in this type of coverage–known as employer-sponsored insurance or ESI–exceeded 62.2 million. In this blog, infographic, and companion documents, SHADAC researchers use data from the Medical Expenditure Panel Survey-Insurance Component (MEPS-IC) to analyze the private-sector ESI landscape in 2021 on a national level and within the states. As discussed in SHADAC’s 2020 ESI coverage blog, the COVID-19 pandemic complicated the collection and analysis of data throughout recent years, leading our researchers to compare 2021 ESI access data against pre-pandemic (2019) estimates and 2021 ESI cost data against 2020 estimates.
Key Findings
Employee Access to Coverage (2019 vs. 2021)
Establishment
Not all private sector establishments offer their employees health insurance coverage. In fact, slightly less than half of establishments in the U.S. offered coverage in 2021 (49.2%). This was a significant increase from 47.4% in 2019.
Offer
The offer of employer-sponsored insurance coverage was extended to the majority of private-sector employees. In 2021, 85.7% of employees in the U.S. worked in establishments that offered health insurance coverage, a rate that remained statistically unchanged from 2019 (85.3%).
Eligibility
Among employees working at establishments that offered coverage, the percent eligible for coverage was 80.3% in 2021; an increase from 77.7% in 2019.
Take-Up
The take-up rate of ESI-eligible employees has varied over the years, and in 2021, 69.8% of eligible employees enrolled in coverage. This represented a 2.1 percentage-point decrease from 2019 (71.9%).
Employee Coverage Costs (2020 vs. 2021)
Premiums and contributions
- The average annual premium for single coverage rose to $7,380 in 2021, a $231 or 3.2% increase from 2020.
- For those enrolled in family coverage, average annual premiums also rose. In this case, premiums climbed to $21,381 in 2021, a $623 or 3.0% increase from 2020.
Deductibles
- For single coverage, the 2021 average individual deductible was $2,004. This represented a significant increase of 3.0% from 2020 ($1,945).
- Among those enrolled in family coverage, the average deductible per employee enrolled was $3,868 in 2021. This was also a significant increase of 3.9% from 2020 ($3,722).
High-Deductible Health Plans
- In 2021, the share of employees enrolled in high-deductible health plans (HDHPs) increased substantially in 2021 to 55.7% – an increase of 5.3 percentage points from 2020.
Key Takeaways
With so many Americans relying on their employers for health insurance coverage, ESI findings remain an important indicator of the financial and health burdens many individuals and families face. In 2021, the U.S. experienced several continuing ESI trends, including rising costs across employee premiums, premium contributions, and deductibles. Additionally, the share of private sector employees enrolled in high-deductible plans increased substantially. In regards to coverage, more employers offered ESI to their employees in 2021 when compared to pre-pandemic levels. Meanwhile, the rate of ESI-eligible employees enrolling in offered coverage was down overall from pre-pandemic, though unchanged from 2020.
For more detailed information on ESI findings from SHADAC, see the following products:

 Report Narrative
Report Narrative
The report narrative provides an in-depth look at 2019-2021 ESI estimates including state-level changes and trends.
50-State Comparison Tables
The 50-state tables include 2017-2021 ESI estimates and allow for easy cross-state and state vs. national analysis.
Other related resources
• 2021 ESI Blog (2019-2020 data)
• 2020 ESI Report, Blog, and Infographic (2015-2019 data)
• 2019 ESI Report, Blog, and Infographic (2014-2018 data)
Blog & News
Pandemic-Era Trends in Employer-Sponsored Health Insurance (ESI), 2019-2020
July 7, 2022:The COVID-19 pandemic continues to disrupt many patterns of life and work in the United States and internationally, while exacerbating many long-standing concerns regarding health care affordability, access, and utilization as well as rates of health insurance coverage for Americans. In this regard, one area of potential pandemic-related impact to consider is coverage rates for employer-sponsored health insurance (ESI), which remains the largest source of coverage for Americans, with 60.1 million private-sector employees enrolled in ESI in 2020.1
In anticipation of the release of the 2021 Medical Expenditure Panel Survey Insurance Component (MEPS-IC) data, SHADAC researchers analyzed private-sector ESI estimates from the 2020 MEPS-IC to better contextualize the forthcoming 2021 estimates. Understanding 2020 coverage data will supply a pandemic-era baseline, while providing a critical vantage point from which to observe and interpret trends in ESI composition, affordability, and access in this critical market.
This narrative provides an overview of the 2020 MEPS-IC private-sector ESI estimates, covering firm size, ESI cost, and access. It’s important to note that the overlay of COVID-19 on this data makes it difficult to interpret the cause of certain changes when compared to pre-pandemic estimates. One area where this is evident is within the composition of private-sector employees by employer firm size.
Small firms declined significantly in 2020
Many employers offer ESI to their employees, regardless of the number of individuals they employ. However, while ESI remains the most common source of coverage for Americans, the composition of private sector employees enrolled in ESI shifted significantly from 2019 to 2020. Specifically, the number of employees in small firms (defined here as <50 employees) experienced a 19 percent decline over this timeframe, leaving a greater proportion of medium and large firms (defined here as >50 employees) to drive trends in ESI access to coverage and cost.
With larger firms comprising an increasingly significant portion of the private sector, trends among this subset of firms are driving overall changes between 2020 and 2019. For this reason, it is difficult to analyze changes in ESI estimates from 2020 to 2019, as these changes could be attributed to actual trends in access, cost, and affordability, or they could be directly tied to this shift in composition of employers and employees.
Number of private-sector employees in the United States, by firm size: 2019—2020
| Employees, all firms |
Less than 50 employees |
50 or more employees |
|
| 2019 | 131,333,000 | 35,113,000 | 96,220,000 |
| 2020 | 122,677,000 | 28,507,000 | 94,171,000 |
| 2019-2020 Change | -8,656,000 | -6,606,000 | -2,049,000 |
| 2019-2020 Percent Change | -7% | -19% | -2% |
Source: SHADAC analysis of the Medical Expenditure Panel Survey—Insurance Component, 2019, 2020.
ESI costs and premiums remain mostly stable
Monitoring costs associated with ESI is essential for understanding health care-related financial burdens for employees. Nationally, 2020 premiums and cost sharing remained relatively stable for employees enrolled in ESI. While premiums for single coverage increased slightly by 2.5 percent ($177), family premiums, employee contributions, and deductibles (for both single and family coverage) remained steady when compared to 2019.
When examined on a state-level, 2020 ESI costs are more varied. Nationally, the average premium for single coverage was $7,149. Certain states exceeded that average in 2020, with Alaska and New York monthly premiums surpassing $8,000 ($8,635 and $8,177 respectively). Meanwhile, Alabama had the lowest premium for single coverage at $6,393. There was also a great deal of variation across states in the size of deductibles. Nationally, the average deducible for single coverage was just under $2,000 in 2020. However, deductibles ranged from an average of $2,500 in Montana to less than $1,500 in Hawaii.
High-deductible health plans (HDHP) represent one common form of ESI. Nationwide, the percent of employees enrolled in a HDHP increased in 2020, rising from 50.5 to 52.9 percent. Moreover, the majority of private-sector employees were enrolled in a HDHP across 36 states in 2020. North Carolina had the highest percentage of HDHP-enrolled employees at 69.5 percent, and Hawaii was at the other end of the spectrum with only 17.6 percent of employees enrolled in HDHPs.
Access to coverage varies by state
Employee access to ESI has three components:
Employee Offer: An employee must work in an establishment that offers coverage.
Employee Eligibility: An employee must meet the criteria established by the employer to be eligible for coverage that is offered.
Employee Take-Up: The employee must decide to enroll in (“take up”) the offer of ESI coverage.
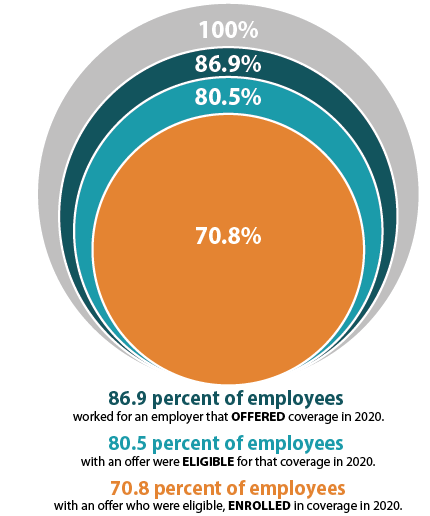
The decision to offer ESI to employees is determined by the employer, with 51.1 percent of private sector firms choosing to offer coverage in 2020 (compared to 47.4 percent in 2019). However, although over half of employers provided optional ESI, not all of their employees were eligible to enroll in that coverage. Meaning, while 86.9 percent of employees worked for an employer offering ESI coverage in 2020, only 80.5 percent were eligible for that coverage; eligibility could be based on a minimum number of hours worked per pay period or a minimum length of service with an employer, for example. Among employees eligible for ESI, overall enrollment declined in 2020, dropping from 71.9 percent to 70.8 percent—a difference of 1.745 million employees.
ESI access also varied across states in 2020. In Hawaii, Tennessee, Massachusetts, Illinois, Pennsylvania, New Jersey, and the District of Columbia (D.C.), more than 90 percent of employees worked at a firm that offered ESI. Meanwhile, less than 75 percent of Montana and Wyoming employees worked for an employer that offered ESI (73.8 percent and 70.6 percent, respectively).
It’s important to note that trends in access are particularly difficult to interpret due to the sharp decline in employees who work in firms with <50 employees, as small firms are much less likely to offer coverage.
To revisit 2019 ESI findings from SHADAC, see the following products:
- Printable version of 2019 ESI Report Narrative
- Companion Blog and Infographic highlighting key findings at the national level regarding ESI coverage affordability and access
- Two-Page Profiles on ESI trends for each state
- 50-State Interactive Map showing levels of, and changes in, average annual premiums for single and family coverage in 2019, with links to state profile pages
- 50-State Comparison Tables including 2015-2019 ESI data
Notes and Sources
Hawaii has a broad employer mandate that preceded the ACA. The Hawaii Prepaid Health Care Act, enacted in 1974, requires private employers to provide health insurance for employees who work at least 20 hours (some exceptions apply).
High-deductible health plans (HDHP) are defined as plans that meet the minimum deductible amount required for Health Savings Account (HSA) eligibility (e.g., $1,400 for an individual and $2,800 for a family in 2020).
The labor market changed significantly between 2019 and 2020 with a dramatic reduction in small firm employment. It is difficult to determine whether 2020 changes in ESI were driven by this change in the labor force or reflect actual changes in ESI access and cost.
Data are from the 2019–2020 Medical Expenditure Panel Survey–Insurance Component (MEPS-IC), produced by the Agency for Healthcare Research and Quality (AHRQ), and are available on SHADAC’s State Health Compare web tool at statehealthcompare.shadac.org.
1 State Health Access Data Assistance Center. (n.d.). Health Insurance Coverage Type (2020)* http://statehealthcompare.shadac.org/bar/279/health-insurance-coverage-type-2020-by-total#0/1/5,4,1,10,86,9,8,6/32/325
Publication
Comparing Federal Government Surveys That Count the Uninsured: 2021
With the release of new insurance coverage estimates from surveys conducted by the U.S. Census Bureau, the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Disease Control and Prevention (CDC), SHADAC has updated our annual “Comparing Federal Government Surveys that Count the Uninsured” brief.
The brief provides an annual update to comparisons of uninsurance estimates from four federal surveys:
- The American Community Survey (ACS)
- The Current Population Survey (CPS)
- The Medical Expenditure Panel Survey - Household Component (MEPS-HC)
- The National Health Interview Survey (NHIS)
In this brief, SHADAC presents current and historical national estimates of uninsurance along with the most recent available state-level estimates from these surveys (where possible). We also discuss the main reasons for variation in the estimates across the different surveys as well as possible reasons for incomparability of estimates across and within the surveys.
Due to the substantial impacts of the COVID-19 pandemic on federal survey data collection and production, this year the brief also includes a brief overview of the unique challenges faced by each agency conducting the four surveys due to pandemic-related disruptions, how the agencies addressed and compensated for these challenges, and what these impacts mean in terms of utilizing survey data on health insurance coverage for 2020.
Download a PDF of the Comparing Federal Government Surveys Brief.
Last year’s brief with data from the 2020 collection year, and certain 2019 collection-year data, can be accessed here.
Publication
Comparing Federal Government Surveys That Count the Uninsured: 2020
 With the release of new insurance coverage estimates from surveys conducted by the U.S. Census Bureau, the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Disease Control and Prevention (CDC), SHADAC has updated our annual “Comparing Federal Government Surveys that Count the Uninsured” brief.
With the release of new insurance coverage estimates from surveys conducted by the U.S. Census Bureau, the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Disease Control and Prevention (CDC), SHADAC has updated our annual “Comparing Federal Government Surveys that Count the Uninsured” brief.
The brief provides an annual update to comparisons of uninsurance estimates from four federal surveys:
- The American Community Survey (ACS)
- The Current Population Survey (CPS)
- The Medical Expenditure Panel Survey - Household Component (MEPS-HC)
- The National Health Interview Survey (NHIS)
In this brief, SHADAC presents current and historical national estimates of uninsurance along with the most recent available state-level estimates from these surveys. We also discuss the main reasons for variation in the estimates across the different surveys as well as possible reasons for incomparability of estimates across and within the surveys.
Download a PDF of the Comparing Federal Government Surveys Brief.
Last year’s brief with data from 2019, and certain 2018 data, can be accessed here.
SHADAC Expertise
MEDICAL EXPENDITURE PANEL SURVEY
The Medical Expenditure Panel Survey (MEPS) is a large set of surveys of families and individuals, their medical providers, and employers across the United States. MEPS is the most complete source of data on the cost and use of health care and health insurance coverage.
MEPS has two major components:
- The Household Component (MEPS-HC) provides data from individual households and their members, which is supplemented by data from their medical providers.
- The Insurance Component (MEPS-IC) is a separate survey of employers that provides data on employer-based health insurance.
MEPS is a panel survey with several rounds of interviews. More information on the study design is available on the MEPS survey design web page.
State-level estimates are available for both components:
Microdata are available for the household component, and MEPS offers data user workshop.
Microdata are not available for the Insurance Component.
MEPS-IC: Employer Coverage by Firm Size - Special Tabulations
To enhance the policy-relevance of the MEPS-IC employer coverage estimates, SHADAC provides annual special tabulations according to the following firm sizes:
- Fewer than 50 employees
- 50 to 99 employees
- 100 or more employees
Click here to access these special tabulations.













