Publication
Impact on Vital Community Conditions: Underlying Factors of Medicaid Inequities Annotated Bibliography
*Click here to jump to the 'Impact on Vital Community Conditions' annotated bibliography*
The State Health Access Data Assistance Center (SHADAC) with support from the Robert Wood Johnson Foundation (RWJF) and in collaboration with partner organizations is exploring whether a new national Medicaid Equity Monitoring Tool could increase accountability for state Medicaid programs to advance health equity while also improving population health.
During the first phase of this project, a conceptual wireframe for the potential tool was created. This wireframe includes five larger sections, organized by various smaller domains, which would house the many individual concepts, measures, and factors that can influence equitable experiences and outcomes within Medicaid (see full wireframe below).
While project leaders and the Advisory Committee appointed at the beginning of the project all agree that the Medicaid program is a critical safety net, they specifically identified the importance and the need for an “Underlying Factors” section of the tool. This section aims to compile academic research and grey literature sources that explain and provide analysis for the underlying factors and root causes that may contribute to inequities in Medicaid.
 |
|
 |
- Historical context of Medicaid inequities
- Information on how underlying factors perpetuate inequities in Medicaid
- Potential solutions for alleviating inequities within Medicaid
Once selected, researchers compiled sources in an organized annotated bibliography, providing a summary of each source and its general findings. This provides users with a curated and thorough list of resources they can use to understand the varied and interconnecting root causes of Medicaid inequities. Researchers plan to continually update this curated selection as new research and findings are identified and/or released.
Sections of the full annotated bibliography include:
- Systemic Racism
- Systemic / Structural Ableism
- Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination
- Reproductive Oppression in Health Care
- Impact on Vital Community Conditions
This page is dedicated to a single section from the full annotated bibliography:
Impact on Vital Community Conditions

Underlying Factors Annotated Bibliography: Impact on Vital Community Conditions
Have a source you'd like to submit for inclusion in our annotated bibliography? Contact us here to propose a source for inclusion.
Click on the arrows to expand / collapse each source.
Semprini, J., Ali, A. K., & Benavidez, G. A. (2023). Medicaid Expansion Lowered Uninsurance Rates Among Nonelderly Adults In The Most Heavily Redlined Areas. Health Affairs, 42(10), 1439–1447. https://doi.org/10.1377/hlthaff.2023.00400
Author(s): Jason Semprini, University of Iowa, College of Public Health; Abinasir K. Ali, University of Iowa, College of Public Health; and Gabriel A. Benavidez, Department of Epidemiology and Biostatistics, University of South Carolina
Article Type: Peer-reviewed journal
While there has been ample research on the effect of Medicaid expansion on reducing individual-level racial and ethnic disparities in health insurance coverage, authors here attempt to fill the gap in research on how Medicaid expansion is affected by root causes of health inequities, such structural racism, as measured by the historically racist policy of residential redlining. The federal government’s rating system for mortgage investments, which benefited white, upper middle-class families and penalized minoritized communities and the working-class, has had lasting effects even after it was outlawed in the late 1960s. These effects include substantial wealth gaps, under-resourced communities, and poorer health outcomes. The authors use data from national surveys and a difference-in-differences design to explore how exposure to historical redlining may have influenced the effect of Medicaid expansion on population-level insurance rates for non-Hispanic Black, non-Hispanic White, and Hispanic nonelderly adults. When comparing uninsurance rates in Medicaid expansion and non-expansion states before and after the passage of the Affordable Care Act, authors found that Medicaid expansion had the greatest impact on lowering uninsurance rates in areas with the highest level of historic redlining. Even though no statistically significant differences were observed by race and ethnicity within each redline category, authors conclude that “Medicaid expansion may have helped to reduce some of the negative consequences of structural racism…” and emphasize the importance of studying contextual factors when evaluating health programs and policies.
Londhe, S., Ritter, G., & Schlesinger, M. (2019). Medicaid Expansion in Social Context: Examining Relationships Between Medicaid Enrollment and County-Level Food Insecurity. Journal of Health Care for the Poor and Underserved, 30(2), 532–546. https://doi.org/10.1353/hpu.2019.0033
Author(s): Shilpa Londhe, Department of Health Policy and Management, Yale School of Public Health; Grant Ritter, Heller School for Social Policy and Management, Brandeis University, Mark Schlesinger, Department of Health Policy and Management, Yale School of Public Health
Article Type: Peer-reviewed journal
This article studies the relationship between county Medicaid enrollment and food insecurity in over 350 counties. The authors acknowledge that food insecurity prevalence ranges widely across the country, from as low as 4 percent up to 39 percent in some states. The authors observe that counties who expanded their Medicaid program in 2012 had significantly reduced food insecurity compared to their baseline year of 2009, and compared to counties that expanded later in calendar year 2014. While the authors acknowledge that food insecurity and lack of insurance coverage are likely related, they conclude that Medicaid likely offers greater financial security overall, which alludes to many improvements for low-income families, with overcoming food insecurity being one positive of many likely effects.
Bowen, S., Elliott, S., & Hardison-Moody, A. (2021). The structural roots of food insecurity: How racism is a fundamental cause of food insecurity. Sociology Compass, 15(7). https://doi.org/10.1111/soc4.12846
Author(s): Sarah Bowen, Professor of Sociology at North Carolina State University; Sinikka Elliot, Associate Professor of Sociology at the University of British Columbia; Annie Hardison-Moody, Associate Professor of Agricultural and Human Sciences at North Carolina State University
Article Type: Peer-reviewed journal
This article, written by scholars in the US and Canada and funded by the US Department of Agriculture, provides a detailed overview of the patterns of food insecurity in the recent past. These patterns of food insecurity include that it is associated with lower income households, mostly cyclical as opposed to chronic, more prevalent in households with children and in households headed by women, and households headed by people of color and people with disabilities. Food insecurity also has negative effects on physical and mental health as well as academic performance and risk of hospitalization among children. Authors summarize evidence on the association between food insecurity and poverty, other forms of hardship, housing insecurity, and neighborhood support systems, but argue that there is a more fundamental cause for food insecurity: racism and persistent unequal access for people of color to opportunities and resources. To combat food insecurity, structural change is needed. While the article does not go into detail about specific recommendations for the Medicaid program, it references advocating for Medicaid expansion and against “...punitive and stringent policies that disproportionately harm people of color…,” which can be the price for access to assistance.
Charania, S. (2021). How Medicaid and States Could Better Meet Health Needs of Persons Experiencing Homelessness. AMA Journal of Ethics, 23(11), E875-880. https://doi.org/10.1001/amajethics.2021.875
Author(s): Sana Charania, George Washington University’s School of Public Health in Washington, DC
Article Type: Peer-reviewed policy reform brief
This peer-reviewed policy reform brief includes a list of strategies that state Medicaid programs can pursue with providers to alleviate health care stressors of those experiencing homelessness. The author remarks that in 2020, over half a million people experience homelessness on any given night in the United States. According to survey data from a decade earlier, about a quarter of “…sheltered persons experiencing homelessness had a severe mental illness and 35 percent had problems with substance use”. The author states that there is a need for better supportive housing options and discusses studies in several states that showed providing permanent housing and needed services (such as behavioral health care) to individuals who were previously homeless led to decreased inpatient or emergency department visits and lower health care costs. The author emphasizes that it is not entirely on state Medicaid programs to reach those experiencing homelessness; clinicians and hospitals have a role to play in resolving biases about this very stigmatized group of people and assessing the basic needs of their patients. The author does highlight the importance of Medicaid expansion under the ACA – citing the improved health conditions of those experiencing homelessness and an increase in coverage in expansion states.
Dennett, J. M., & Baicker, K. (2022). Medicaid, Health, and the Moderating Role of Neighborhood Characteristics. Journal of Urban Health, 99(1), 116–133. https://doi.org/10.1007/s11524-021-005792
Author(s): Julia M. Dennett, Yale University School of Public Health, New Haven, CT; Katherine Baicker, University of Chicago Harris School of Public Policy, Chicago, IL and the National Bureau of Economic Research, Cambridge, MA.
Article Type: Peer-reviewed journal
This article is an analysis of whether key neighborhood characteristics, such as “socioeconomic deprivation (which is a score that reflects neighborhood ethnicity, education, employment, poverty, and housing/crowding), food access, park access and green space, attributes that promote active living, and land use” influence the effect of health insurance coverage on health outcomes. Using data collected in 2009 and 2010 about participants in the Oregon Health Insurance living in the Portland area, some of whom had access to Medicaid coverage and some of whom did not, authors found neighborhood characteristics played only a limited role in moderating the impacts of coverage on select health outcomes. The study’s null findings imply that Medicaid expansion benefited many across the board, regardless of neighborhood. Also implied is that the relationship between coverage and neighborhood characteristics and health outcomes is complex. Authors note several study limitations, including other factors to consider in the definition of neighborhood characteristics and their inability to conduct subgroup analyses. They also call for future research to inform policy.
Satcher, L. A. (2022). (Un) Just Deserts: Examining Resource Deserts and the Continued Significance of Racism on Health in the Urban South. Sociology of Race and Ethnicity, 8(4), 483–502. https://doi.org/10.1177/23326492221112424
Author(s): Lacee Satcher, Professor of Sociology and Environmental Studies at Boston College
Article Type: Peer-reviewed journal
This peer-reviewed article summarizes research examining the relationship between resource scarcity (measured in terms of multiply-deserted areas (MDAs)) and health. The author goes on to discuss how this relationship varies according to race and class composition of urban neighborhoods in the South and its implications for public programs, including Medicaid. MDAs were constructed based on three types of resource deserts: food, green spaces, and pharmacy deserts. Health outcomes examined included adults with diabetes, obesity, asthma, and no leisure-time physical activity. Results show that, compared to less resource-scarce areas, MDAs are associated with higher disease prevalence as well as higher rates of inactivity. Co-occurring resource scarcity has more influence on outcomes and activity levels than single-resource scarcity resulting in greater stress and negative impacts on health. “While there have been efforts to increase food access or greenspace for low-income, predominantly Black neighborhoods via farmer’s markets and community gardens, understanding that these neighborhoods are experiencing compounded, co-occurring resource scarcity calls for a more comprehensive policy intervention or community initiative that increases access to healthy foods, greenspace, and prescription medicines.” The author explains further that, “reducing disparities in prescription access and adherence via expansion of Medicare Part D and Medicaid are important, but study findings suggest that policy efforts to reduce disparities should also increase spatial access to pharmacies.”
Wei, Y., Qiu, X., Sabath, M. B., Yazdi, M. D., Yin, K., Li, L., Peralta, A. A., Wang, C., Koutrakis, P., Zanobetti, A., Dominici, F., & Schwartz, J. D. (2022). Air Pollutants and Asthma Hospitalization in the Medicaid Population. American Journal of Respiratory and Critical Care Medicine, 205(9). https://doi.org/10.1164/rccm.202107-1596oc
Author(s): Yaguang Wei, Xinye Qiu, Mahdieh Danesh Yazdi, Longxiang Li, Adjani A. Peralta, Cuicui Wang, Petros Koutrakis, Antonella Zanobetti, are all from the Department of Environmental Health at Harvard T.H. Chan School of Public Health; Matthew Benjamin Sabath Francesca Dominici are from the Department of Biostatistics at Harvard T.H. Chan School of Public Health; Kanhua Yin is from the Department of Epidemiology at Harvard T.H. Chan School of Public Health; and Joel D. Schwartz is associated with both the Department of Environmental Health at Harvard T.H. Chan School of Public Health as well as the Department of Surgery, Massachusetts General Hospital, Harvard Medical School.
Article Type: Peer-reviewed journal
This peer reviewed study analyzes inpatient claims of Medicaid beneficiaries from 2000 to 2012 by zip code in order to determine the effect of three common air pollutants (nitrogen dioxide, ozone pollution, and particulate matter) on asthma hospitalizations. The researchers found a positive relationship between short-term exposures and increased risk of asthma hospitalization for those with one asthma admission during the study period, but air pollutants appeared to be less of a factor for those with multiple asthma admissions during the study period. A community-level analysis found higher risk of asthma hospitalization for people living in low population density zip codes, people with higher average BMI, and people living a longer distance to the nearest hospital. There were no significant differences in risk of asthma hospitalizations by race or ethnicity. These results emphasize the importance of both individual and contextual factors in assessing the quality of health care for the Medicaid population, where the impact of air pollutant exposures on asthma susceptibility differed by severity and place characteristics.
[1] State Health & Value Strategies (SHVS). (2021). Talking about anti-racism and health equity: Discussing racism. https://www.shvs.org/wp-content/uploads/2021/08/Talking-About-Anti-Racism-Health-Equity-1-of-3.pdf
Blog & News
Disability Health Care Data and Information: Resources from SHADAC
August 08, 2024:- Unfair treatment in health care settings, at work, or when applying for public benefits
- Adults with disabilities are more likely to live in poverty compared to adults with no disability
- People with a disability often have increased medical expenses, with a study from the National Disability Institute estimating that a U.S. household containing an adult with a disability must spend an estimated 28% more income to obtain the same standard of living as a household with no disability
- Those with disabilities have twice the risk of developing chronic health conditions like depression, diabetes, asthma, and poor oral health
Federal Survey Sample Size Analysis: Disability, Language, and Sexual Orientation and Gender Identity
- People who indicated sexual orientation or gender identity (SOGI)
- People with language access needs, and
- People with disabilities
Collection of Self-Reported Disability Data in Medicaid Applications: A Fifty-State Review of the Current Landscape (SHVS Brief)
State Health Compare Disability Breakdowns
Housing Affordability Matters: Unaffordable Rents Infographics Updated with 2022 Data
Minnesota Community and Uninsured Profile
Stay Informed on Disability Health Data Resources and Information
Publication
Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination: Underlying Factors of Medicaid Inequities Annotated Bibliography
*Click here to jump to the 'Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination' annotated bibliography*
The State Health Access Data Assistance Center (SHADAC) with support from the Robert Wood Johnson Foundation (RWJF) and in collaboration with partner organizations is exploring whether a new national Medicaid Equity Monitoring Tool could increase accountability for state Medicaid programs to advance health equity while also improving population health.
During the first phase of this project, a conceptual wireframe for the potential tool was created. This wireframe includes five larger sections, organized by various smaller domains, which would house the many individual concepts, measures, and factors that can influence equitable experiences and outcomes within Medicaid (see full wireframe below).
While project leaders and the Advisory Committee appointed at the beginning of the project all agree that the Medicaid program is a critical safety net, they specifically identified the importance and the need for an “Underlying Factors” section of the tool. This section aims to compile academic research and grey literature sources that explain and provide analysis for the underlying factors and root causes that may contribute to inequities in Medicaid.
 |
|
 |
- Historical context of Medicaid inequities
- Information on how underlying factors perpetuate inequities in Medicaid
- Potential solutions for alleviating inequities within Medicaid
Once selected, researchers compiled sources in an organized annotated bibliography, providing a summary of each source and its general findings. This provides users with a curated and thorough list of resources they can use to understand the varied and interconnecting root causes of Medicaid inequities. Researchers plan to continually update this curated selection as new research and findings are identified and/or released.
Sections of the full annotated bibliography include:
- Systemic Racism
- Systemic / Structural Ableism
- Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination
- Reproductive Oppression in Health Care
- Impact on Vital Community Conditions
This page is dedicated to a single section from the full annotated bibliography:
Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination

Underlying Factors Annotated Bibliography: Sexual Orientation, Gender Identity, and Gender Affirming Care Discrimination
Have a source you'd like to submit for inclusion in our annotated bibliography? Contact us here to propose a source for inclusion.
Click on the arrows to expand / collapse each source.
Mallory, C., & Tentindo, W. (2022). Medicaid Coverage for Gender-Affirming Care. Williams Institute UCLA School of Law. https://escholarship.org/content/qt4ng3j6st/qt4ng3j6st.pdf
Author(s): Christy Mallory and Will Tentindo, Williams Institute at University of California - Los Angeles
Article Type: Report
This report highlights key factors related to Medicaid coverage of gender affirming care. Emphasis is placed on the sheer number of individuals who identify as transgender or gender non-conforming that are covered by Medicaid – about one fourth of those who identify as transgender or gender non-conforming in the United States rely on Medicaid for their gender affirming care. Underlying factors contributing to inequities for this group include unclear language about what services are covered, and/or gender affirming care services are not covered at all in their state. Authors urge all states to fully expand their Medicaid program under the Affordable Care Act.
Kempf, R., Elias, N., & Rubin-DeSimone, A. (2021). Transgender and Gender Non-Binary Healthcare Coverage in State Medicaid Programs: Recommendations for More Equitable Approaches. Journal of Health and Human Services Administration, 44(1), 86–108. https://doi.org/10.37808/jhhsa.44.1.5
Author(s): Robin J. Kempf, Assistant Professor in the College of Public Service at the University of Colorado - Colorado Springs; Nicole M. Elias, Associate Professor in the Department of Public Management at John Jay College of Criminal Justice, City University of New York; Alonso J. Rubin-DeSimone, John Jay College of Criminal Justice, City University of New York
Article Type: Peer-reviewed journal
This peer reviewed journal article describes how transgender and gender non-binary individuals have been marginalized historically in U.S. society, including in terms of institutional or informal “erasure” as well as through isolation and “hypervisibility.” In health care, this discrimination translates into lack of access to qualified professionals and lack of coverage for a continuum of needed services. Authors chose to review state Medicaid program coverage policies to identify opportunities to build equity for all U.S. residents and noted that discrimination of individuals identifying as non-cisnormative gender can be compounded by the intersectionality of race, sexual orientation, socioeconomic status, and geographical location. They assessed comprehensiveness of state Medicaid coverage in accordance with the World Professional Association for Transgender Health (WPATH) standards. Authors found that the five states in their sample varied widely in terms of health coverage to transgender and gender non-binary Medicaid beneficiaries, however, there were stand out states in terms of the continuum of services offered as well as opportunities for improvement. Authors recommend removal of barriers to needed care such as prior authorization requirements as well as additional training for providers and individuals making coverage determinations.
Yuan, N., Chung, T., Ray, E. C., Sioni, C., Jimenez-Eichelberger, A., & Garcia, M. M. (2021). Requirement of mental health referral letters for staged and revision genital gender-affirming surgeries: An unsanctioned barrier to care. Andrology, 9(6), 1765–1772. https://doi.org/10.1111/andr.13028
Author(s): Nance Yuan, Cedars-Sinai Transgender Surgery and Health Program, and member of the Urology and Plastic Surgery Divisions at Cedars-Sinai Medical Center; Theodore Chung, David Geffen School of Medicine, University of California, Los Angeles; Alma Jimenez-Eichelberger and Caitlin Sioni, Cedars-Sinai Transgender Surgery and Health Program and the Division of Urology at Cedars-Sinai Medical Center; Edward C. Ray, Division of Plastic Surgery, Cedars-Sinai Medical Center; Maurice M. Garcia, Departments of Urology and Anatomy, University of California, San Francisco
Article Type: Peer-reviewed journal
This peer reviewed article investigates and discusses insurance requirements for referral letters from mental health providers prior to genital gender affirming surgeries for trans and non-binary individuals. In this study, half of the participants had federally funded insurance, such as Medicaid. Most plans, both public and private, required at least two referral letters at every stage of surgery (there may be four to five stages depending on the operation). Authors state that it took office staff, “an average of 2.5 hours per patient, per surgery, dedicated to coordinating submission of updated referral letters”. Some participants had to cancel or reschedule an operation due to lack of coordination of care, and/or administration not receiving referral letters. This resulted in patients being forced to pay for surgeries out-of-pocket instead of using insurance coverage. The authors discuss how multiple letters for each stage of a surgery is unnecessary, when no participant was deemed mentally unfit for any previously performed procedure. Authors state that requiring updated letters for each year was also a point of stress for participants as these administrative burdens were “costly and burdensome” to patients and providers alike. The authors urge organizations such as the World Professional Association for Transgender Health (WPATH) to revisit their recommendations for referral letter requirements to alleviate the burdens on both administrators and patients alike.
Mann, S. J., Carpenter, C. S., Gonzales, G., Harrell, B., & Deal, C. (2022). Effects of the affordable care Act’s Medicaid expansion on health insurance coverage for individuals in same-sex couples. Health Services Research, 58(3), 612–621. https://doi.org/10.1111/1475-6773.14128
Author(s): Samuel Mann, Christopher S. Carpenter, Benjamin Harrell, and Cameron Deal are all from the Department of Economics, LGBTQ+ Policy Lab, Vanderbilt University, Nashville, Tennessee; Gilbert Gonzales is also a member of the Department of Medicine, Health & Society, and Department of Health Policy at Vanderbilt University.
Article type: Peer-reviewed journal
This peer reviewed journal article analyzes how Medicaid expansion influenced health insurance coverage for individuals in same-sex partnerships. Using data from the American Community Survey, authors found that there was a significant increase in coverage between 2009 and 2018 for low-income adults who were in a same-sex relationship, especially for women. The authors attribute this to a much higher prevalence of children being in households of women same-sex couples compared to men. The authors also state that sexual minority women may have stronger social ties that reduce stigma surrounding Medicaid or public options compared to sexual minority men. This research has implications that are important for policymaking and underlying factors of inequity within Medicaid in terms of barriers to seeking health insurance coverage and accessibility of services for those individuals in same-sex partnerships.
[1] Human Rights Campaign. (n.d.). Sexual Orientation and Gender Identity Definitions. Human Rights Campaign; HRC Foundation. https://www.hrc.org/resources/sexual-orientation-and-gender-identity-terminology-and-definitions
[2] Ibid.
[3] HHS Office of Population Affairs. (n.d.). Gender-Affirming Care and Young People. U.S. Department of Health & Human Services. https://opa.hhs.gov/sites/default/files/2023-08/gender-affirming-care-young-people.pdf
Blog & News
Race/Ethnicity Data in CMS Medicaid (T-MSIS) Analytic Files: 2021 Data Assessment
December 6, 2023:The Transformed Medicaid Statistical Information System (T-MSIS) is the largest national database of current Medicaid and Children’s Health Insurance Program (CHIP) beneficiary information collected from U.S. states, territories, and the District of Columbia (DC).1 T-MSIS data are critical for monitoring and evaluating the utilization of Medicaid and CHIP, which together provide health insurance coverage to almost 90 million people.2
Due to their size and complexity, T-MSIS data files are challenging to use directly for research and analytic purposes. To optimize these files for health services research, Centers for Medicare and Medicaid Services (CMS) repackages them into a user-friendly, research-ready format called T-MSIS Analytic Files (TAF) Research Identifiable Files (RIF). One such file, the Annual Demographic and Eligibility (DE) file, contains race and ethnicity information for Medicaid and CHIP beneficiaries. This information is vital for assessing enrollment, access to services, and quality of care across racial and ethnic groups in the Medicaid/CHIP population, whose members are particularly vulnerable due to limited income, physical and cognitive disabilities, old age, complex medical conditions, housing insecurity, and other social, economic, behavioral, and health needs.
To guide researchers and other consumers in their use of T-MSIS data, CMS produces data quality assessments of the completeness of race and ethnicity data along with other data such as enrollment, claims, expenditures, and service use. The Data Quality (DQ) assessments for race and ethnicity data have been posted for data years 2014 through 2021 and indicate varying levels of “concern” regarding race and ethnicity data completeness. Some data years have multiple data versions (e.g., Preliminary, Release 1, Release 2), each with their own DQ assessment.
While completeness of race and ethnicity data reported to CMS has historically remained inconsistent among the states, territories, and DC, SHADAC has been monitoring the quality of these data over time. We are excited to discuss a noticeable improvement in quality as discussed below. This blog explores not only the 2021 Data Release 1, the most recent T-MSIS race and ethnicity data for which a DQ assessment is available, but also a brief analysis of data quality trends over time that we plan to follow in future T-MSIS file releases.
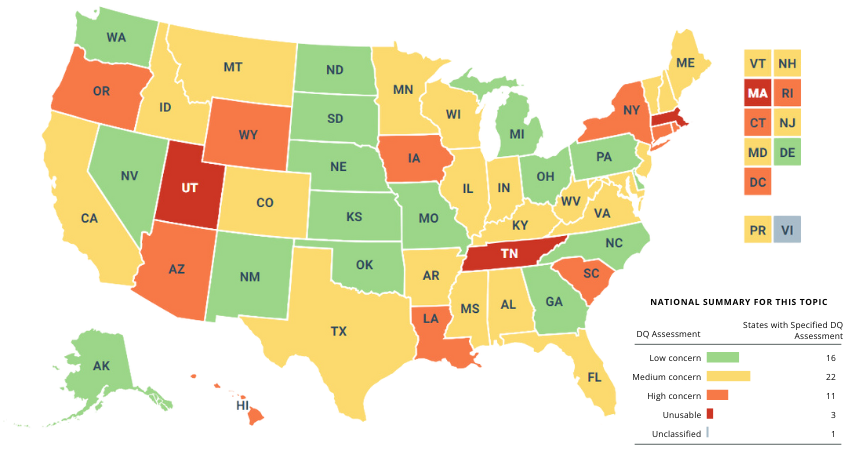
Evaluation of T-MSIS Race and Ethnicity Data
DQ assessments for each year and data version of T-MSIS data are housed in the Data Quality Atlas (DQ Atlas), an online evaluation tool developed as a companion to T-MSIS data.3 The DQ Atlas assesses T-MSIS race and ethnicity data using two criteria: the percentage of beneficiaries with missing race and/or ethnicity values in the TAF; and the number of race/ethnicity categories (out of five) that differ by more than ten percentage points between the TAF and American Community Survey (ACS) data. Taken together, these two criteria indicate the level of “concern” (i.e., reliability) for states’ T-MSIS race/ethnicity data. To construct the external ACS benchmark for evaluating T-MSIS data, creators of the DQ Atlas combine race and ethnicity categories in the ACS to mirror race and ethnicity categories reported in the TAF (see Table 1). More information about the evaluation of T-MSIS race and ethnicity data is available in the DQ Atlas’ Background and Methods Resource.
Five “concern” categories appear in the DQ Atlas: Low Concern, Medium Concern, High Concern, Unusable, and Unclassified. States with substantial missing race/ethnicity data or race/ethnicity data that are inconsistent with the ACS – a premier source of demographic data – are grouped into either the High Concern or Unusable categories, whereas states with relatively complete race/ethnicity data or race/ethnicity data that align with ACS estimates are grouped into either the Low Concern or Medium Concern categories. The Unclassified category includes states for which benchmark data are incomplete or unavailable for a given data year and version.
Table 1. Crosswalk of Race and Ethnicity Variables between the TAF and ACS
| Race/Ethnicity Category |
Race/Ethnicity Flag Value in TAF |
Combination of Race and Hispanic Variables in ACS |
| Hispanic, all races |
7=Hispanic, all races | Hispanic, all races |
| Other races, non-Hispanic |
4= American Indian and Alaska Native, non-Hispanic 5=Hawaiian/Pacific Islander 6=Multiracial, non-Hispanic |
- American Indian alone - Alaska Native alone - American Indian and Alaska Native tribes specified; or American Indian or Alaska native, non-specified and no other race - Native Hawaiian and other Pacific Islander alone - Some other race alone - Two or more races |
Source: Medicaid.gov. (n.d.). DQ Atlas: Background and methods resource [PDF file]. Available from https://www.medicaid.gov/dq-atlas/downloads/background-and-methods/TAF-DQ-Race-Ethnicity.pdf Accessed December 1, 2023.
Quality Assessment by State
Table 2 shows the Race and Ethnicity DQ Assessments for the 2021 TAF (Data Version: Release 1). The categorization criteria used to determine the levels of concern for the 2021 TAF Release 1 data are the same as those used to assess T-MSIS data from previous years and versions. 16 states received a rating of “Low Concern.” There were 22 states (including Puerto Rico [PR]) that fell into the “Medium Concern” category.
Most of the “Medium Concern” states (19 of 22) fell into the subcategory denoting the higher percentage range of missing race/ethnicity data (from 10 percent up to 20 percent). A similar pattern can be seen among the “High Concern” states, most of which (8 of 11) fell into the subcategory denoting the highest percentage range of missing race/ethnicity data (from 20 percent up to 50 percent).
Finally, 11 states (including DC) received a rating of “High Concern.” Three states (Massachusetts, Tennessee, and Utah) received an “Unusable” rating, as each of these states was missing at least 50 percent of race/ethnicity data. The Virgin Islands (VI) is the only state/territory categorized as “Unclassified” in the 2021 TAF (Data Version: Release 1) due to insufficient or incomplete data, and does not appear in Table 2.
Table 2. Race and Ethnicity Data Quality Assessment, 2021 T-MSIS Analytic File (TAF) Data Release 1
| Data quality assessment |
Percent of beneficiaries with missing race/ethnicity values | Number of race/ethnicity categories where TAF differs from ACS by more than 10% |
Number of states* |
States |
| Low Concern | <10% | 0 | 16 | AK, DE, GA, KS, MI, MO, NE, NV, NM, NC, ND, OH, OK, PA, SD, WA |
| Medium Concern | <10% | 1 or 2 | 3 | ID, IL, VA |
| 10% - <20% | 0 or 1 | 19 | AL, AR, CA, CO, FL, IN, KY, ME, MD, MN, MS, MT, NH, NJ, PR, TX, VT, WV, WI | |
| High Concern | <10% | 3 or more | 1 | RI |
| 10% - <20% | 2 or more | 2 | AZ, LA | |
| 20% - <50% | Any value | 8 | CT, DC, HI, IA, NY, OR, SC, WY | |
| Unusable | >50% | Any value | 3 | MA, TN, UT |
Notes: *T-MSIS includes all 50 states, the District of Columbia (DC), and the U.S. territories of Puerto Rico (PR) and the Virgin Islands (VI). However, a DQ assessment is not available for VI in the 2021 TAF (Data Version: Release 1) due to incomplete/unavailable data.
Despite ongoing variation in the completeness of race and ethnicity data reported to CMS, SHADAC researchers have noted a trend toward better quality data overall. Since beginning to track these quality assessments with the 2019 T-MSIS TAF release, a number of states have shifted up the quality assessment scale with noticeably fewer states seeing their data classified as “High Concern.” Specifically, 2021 race/ethnicity TAF data from 11 states received a rating of “High Concern” compared to 16 states’ data in 2020 and 17 states’ data in 2019. The number of states with “Unusable” data has also dropped each year – 3 states’ 2021 race/ethnicity TAF data was classified as “Unusable” compared to 4 states’ data in 2020 and 5 states’ data in 2019.
Visualizing T-MSIS Data in the DQ Atlas
The DQ Atlas enables users to generate maps and tables that compare the quality of T-MSIS data between states across different topics, such as race/ethnicity, age, income, and gender (see Figure 1). Visualizing T-MSIS data in this manner can help researchers quickly assess the completeness of a single variable as well as the relative completeness (or incompleteness) of certain variables compared to others. For example, in the 2021 TAF Data Release 1, all states and territories received a “Low Concern” rating for age data, whereas only 31 states and territories received a “Low Concern” rating for family income.
Figure 1. Data Quality Assessments of Beneficiary Information by U.S. State/Territory
Notes: Green = low concern; yellow = medium concern; orange = high concern; red = unusable; grey = unclassified.
Source: Medicaid.gov. (n.d.). DQ Atlas: Race and Ethnicity [2021 Data set: Version: Release 1]. Available from https://www.medicaid.gov/dq-atlas/landing/topics/single/map?topic=g3m16&tafVersionId=35 Accessed December 1, 2023.
Looking Ahead
Increasingly, a wide diversity of voices from non-profits, health insurers, state-based marketplaces, and policymakers have called for improving the collection of race, ethnicity, and language data, often with the goal of advancing health equity. CMS’s efforts to improve the quality and availability of T-MSIS data reflect this nationwide movement toward data collection practices that more accurately capture the diversity of the U.S. population.
SHADAC was excited to see the revised Office of Management and Budget (OMB) standards related to the collection of race and ethnicity data. The proposed revisions align with available evidence, are consistent with the changes made by leading states, and, most importantly, explicitly state that these standards should serve as a minimum baseline with a call to collect and provide more granular data. However, while these standards are specifically named as minimum reporting categories for data collection throughout the Federal Government, if adopted they are likely to shape data collection and reporting across all sectors, including the states that collect race/ethnicity data through the Medicaid application process.
Many states express difficulties reporting data, as there is misalignment in how state eligibility systems, Medicaid Management Information System (MMIS), and T-MSIS format race and ethnicity data. Before states submit data to T-MSIS, they must reformat and aggregate data, which may affect the quality of submitted data. One approach to improve the collection and reporting of data is providing states with an updated model application using evidence-based approaches to race and ethnicity questions that improve applicant response rate and data accuracy.
Sources
1 Medicaid.gov. Transformed Medicaid Statistical Information System (T-MSIS). Retrieved October 20, 2022, from https://www.medicaid.gov/medicaid/data-systems/macbis/transformed-medicaid-statistical-information-system-t-msis/index.html#
2 Medicaid.gov. August 2023 Medicaid & CHIP Enrollment Data Highlights. Retrieved on December 1, 2023, from https://www.medicaid.gov/medicaid/program-information/medicaid-and-chip-enrollment-data/report-highlights/index.html3 Saunders, H., & Chidambaram, P. (April 28, 2022). Medicaid Administrative Data: Challenges with Race, Ethnicity, and Other Demographic Variables. Kaiser Family Foundation. Retrieved October 31, 2022, from https://www.kff.org/medicaid/issue-brief/medicaid-administrative-data-challenges-with-race-ethnicity-and-other-demographic-variables/
4 Wang, H.L. (June 15, 2022). Biden officials may change how the U.S. defines racial and ethnic groups by 2024. NPR. Retrieved November 1, 2022, from https://www.npr.org/2022/06/15/1105104863/racial-ethnic-categories-omb-directive-15
5 Diaz, J. (August 16, 2022). California becomes the first state to break down Black employee data by lineage. NPR. Retrieved November 1, 2022, from https://www.npr.org/2022/08/16/1117631210/california-becomes-the-first-state-to-break-down-black-employee-data-by-lineage
6 The New York State Senate. (December 22, 2021). Assembly Bill A6896A. Retrieved November 2, 2022, from https://www.nysenate.gov/legislation/bills/2021/A689
Blog & News
SHADAC's Lynn Blewett Featured on 'Hospitals in Focus' Podcast
November 01, 2023: SHADAC Director Dr. Lynn Blewett was recently invited to join Federation of American Hospitals CEO and President Chip Kahn as a guest on his podcast Hospitals in Focus to share her thoughts on the impacts of the unwinding of the Medicaid continuous coverage requirement. The “unwinding” is a term used to describe the progressive ending of the provision included in the Families First Coronavirus Response Act (FFCRA), that allowed people to remain on Medicaid without needing to go through the re-enrollment process during the COVID-19 epidemic. With the end of this in sight, it’s been projected that millions are now facing either the need to quickly find other coverage or a total loss of coverage due to barriers for re-enrollment.
SHADAC Director Dr. Lynn Blewett was recently invited to join Federation of American Hospitals CEO and President Chip Kahn as a guest on his podcast Hospitals in Focus to share her thoughts on the impacts of the unwinding of the Medicaid continuous coverage requirement. The “unwinding” is a term used to describe the progressive ending of the provision included in the Families First Coronavirus Response Act (FFCRA), that allowed people to remain on Medicaid without needing to go through the re-enrollment process during the COVID-19 epidemic. With the end of this in sight, it’s been projected that millions are now facing either the need to quickly find other coverage or a total loss of coverage due to barriers for re-enrollment.
In the episode, Dr. Blewett discusses this very large change that’s occurring across the U.S. healthcare system. As of April 1, 2023, “States have started to redetermine all of the people on their programs to make sure they’re eligible,” she says, and “a new analysis shows that 500,000 people across eleven states have already dropped off Medicaid.” The podcast discusses specific cases and lessons that can be learned from states’ experiences - the good and the bad. Dr. Blewett dives into the different states’ methods for approaching the re-enrollment process, and how certain methods and diligence will affect any potential for procedural errors during this tumultuous period. There are also some states who are deciding to reinstate certain work requirements for people on Medicaid, which Blewett says “haven’t worked very well,” pointing out that: “There’s an estimate that 8 out of 10 Medicaid recipients who are not blind, disabled, or are able to work, already work. They either work part-time or full-time, and so you’re really targeting a very small number of people.”
In addition to the primary concern of people losing access to healthcare, there are many practical reasons that keeping populations on Medicaid actually helps state economies. To close out the discussion, Dr. Blewett highlights the financial impact that the unwinding could have on certain hospitals who were previously being compensated by the federal support that was coming from the increased number of Medicaid enrollees.