Blog & News
Uninsured Profiles: New Resource from SHADAC Aims to Identify and Characterize Communities of Minnesota’s Uninsured Population
September 20, 2019:Over the past year, Dr. Kathleen Call and her research team at SHADAC have worked to build, refine, and now, publish, an interactive tool that allows users to better understand and define the uninsured population in Minnesota at the zip-code level. Partnering with the Blue Cross Blue Shield Foundation of Minnesota, who provided funding for the project, and with essential guidance from the advisory board of MNsure navigators and policymakers, this newly available resource consists of two cooperative components meant to be used concurrently with one another: a downloadable and interactive Excel spreadsheet tool, and an interactive Minnesota map.
Both components provide rates and counts of the uninsured in Minnesota at the ZIP code level (i.e., Census-defined ZIP code), compare characteristics of the total population to the uninsured population in that ZIP code, and provide an in-depth profile of the community characteristics. The map also shows the location of each ZIP code in relation to schools, hospitals, native reservations, and other important or distinctive landmarks.
The profile was designed as a way to support targeted outreach and enrollment activities of health insurance navigators and provide a way to identify and characterize hotspot communities with high uninsurance rates for policymakers as they develop strategies to reach the remaining uninsured in the state of Minnesota.
 For additional information on the uninsured profile tool, or to request the development of a similar tool for another state (which Dr. Call and her team hope to do in the future), readers can access the Uninsured Profile resource webpage to download the tool in Excel spreadsheet format, utilize and view the interactive map, and provide feedback on their user experience.
For additional information on the uninsured profile tool, or to request the development of a similar tool for another state (which Dr. Call and her team hope to do in the future), readers can access the Uninsured Profile resource webpage to download the tool in Excel spreadsheet format, utilize and view the interactive map, and provide feedback on their user experience.
Blog & News
A Deeper Dive on Employer-sponsored Health Insurance: Costs in Five States in Comparison with the United States (Infographics)
September 19, 2019:High health care costs have increasingly been a concern across the United States. Though presidential candidates have recently put forth proposals for changing the role of private insurance within the health care system, recent polls suggest that American consumers would rather hear about plans to lower the rising costs paid by individuals, such as deductibles and copays.[i]
Findings from SHADAC’s analysis of employer-sponsored insurance (ESI) in 2018 back up these consumer concerns. Researchers noted that employees on average paid higher-than-ever premiums ($6,715 for single coverage and $19,565 for family) and deductibles ($1,846 and $3,392 for single and family coverage, respectively) for their health plans last year. Rising costs have also led to record enrollment in high-deductible health plans (HDHPs), with nearly half of workers (49.1 percent) enrolled in such a plan in 2018.[ii]
Using data from Medical Expenditure Panel Survey Insurance Component (MEPS-IC), SHADAC has conducted a deeper dive into a state-level analysis of ESI trends in order to better understand which states are most affected by increasing premiums and deductibles or might have a population with high enrollment in HDHPs, leaving them financially vulnerable in case of an unexpected health crisis that leads to large medical bills.
We compared costs in four categories—high-deductible health plan enrollment, average annual deductibles for single and/or family coverage, average annual premiums for single and/or family coverage, and annual employee contributions for single and/or family coverage—for individual states and the United States, and identified five states (Arizona, Connecticut, Florida, New Hampshire, and Tennessee) where costs were significantly higher than the national average for last year across multiple (though not all) categories of ESI coverage.
Five States with the Highest ESI Costs Compared with the National Average
 Arizona
Arizona
In Arizona, the percent of employees enrolled in high-deductible health plans (HDHPs) was 59.3 in 2018, significantly greater (20.8 percent) than the national average of 49.1 percent and a continuation of consistently higher enrollment in HDHPs in Arizona as compared to the U.S. over the past five years.[iii] After decreasing from 2016 to 2017, average annual deductibles for single ESI coverage increased to $2,166 in 2018, a significantly higher amount (17.3 percent or $320) than $1,846, the nation’s average. Arizona employee contributions for single coverage ESI plans measured at 25.0 percent in 2018, a significantly higher amount (17.4 percent) than the national average of 21.3 percent.
 Connecticut
Connecticut
The share of Connecticut employees enrolled in high-deductible ESI plans was 55.3 percent in 2018—greater (by 12.6 percent) than the national average, though this difference was not statistically significant. Average annual premiums for single ESI coverage in Connecticut were $7,264 in 2018, a significant 8.2 percent ($549) higher than the average of $6,715 for the U.S. In 2018, average annual premiums for family ESI coverage measured at $20,735, also significantly greater (6.0 percent or $1,170) than the national average of $19,565. Additionally, Connecticut’s average single-coverage deductibles measured a significant 25.8 percent ($476) higher than the national average ($2,322 compared to $1,846).
 Florida
Florida
The percent of Florida employees enrolled in HDHPs was 56.7 percent in 2018, which was again significantly greater (15.5 percent) than the national average of 49.1 percent. Employee contributions for family coverage measured at 31.2 percent in 2018, a significantly higher amount (12.2 percent) than the national average. Average annual premiums for single ESI coverage in Florida increased to $6,674 in 2018, a 10.0 percent jump ($606) from $6,068 in 2017, though in both years were relatively close to the U.S. average. Average annual premiums for family ESI coverage increased even more significantly in 2018, soaring by $1,745 to $18,934 from $17,189 in 2017.
 New Hampshire
New Hampshire
The state of New Hampshire saw 67.4 percent of the state’s employees enrolled in HDHPs in 2018, a significantly higher amount than the national average by 37.3 percent. At $7,405 in 2018, average annual premiums for single ESI coverage in New Hampshire were significantly higher by 10.3 percent (or $690) than the U.S. average of $6,715. Average annual deductibles for single ESI coverage were also significantly higher in this state ($2,337) than the national average ($1,846) by 26.6 percent, or $491. The average family-coverage deductible in New Hampshire for 2018 was $4,644, a significantly greater amount ($1,252 or 36.9 percent) than the national average of $3,392.
 Tennessee
Tennessee
The measure of Tennessee employees enrolled in high-deductible ESI plans was 56.8 percent in 2018—significantly greater (15.7 percent) than the national average of 49.1 percent. The average deductible for single coverage ESI plans was $2,235, approximately 21.1 percent higher than the national average of $1,846 by $389. The average employee contribution for family ESI coverage in Tennessee was significantly higher than the U.S. average in 2018—31.2 percent and 27.8 percent, respectively, a difference of 12.2 percent between the state and the nation.
Explore More Data on ESI in the United States
As the majority of the U.S. population continues to receive health insurance coverage from their employer, it is important to remember that ESI trends in rising premiums and deductibles, as well as continuing high enrollment in HDHPs, affect a significant number of people. Though we have here highlighted five states in which costs are particularly high for residents as compared with the United States, other states face similar struggles to varying degrees, as noted in our original report. To explore the trends in any particular state, users can access, read, and/or download the original report narrative, or can explore SHADAC’s State Health Compare web tool, which features state-level data on five measures relating to ESI: Workers in Establishments that Offer Coverage, Average Annual ESI Premium, Average Annual ESI Deductible, Employee Contributions to Premiums, and High-Deductible Health Plans.
[i] Morning Consult. (2019, September 18). Next Time, Voters Want a Health Care Debate That Hits Closer to Home. Retrieved from https://morningconsult.com/2019/09/18/next-time-voters-want-a-health-care-debate-that-hits-closer-to-home/
[ii] Defined as plans that qualify for a tax-advantaged health savings account. In 2018, qualifying plans had to have a $1,350 deductible or higher for single coverage and $2,700 deductible or higher for family coverage.
[iii] SHADAC analysis of MEPS-IC data. Percent of private-sector employees enrolled in high-deductible health insurance plans [Arizona and the United States]. Retrieved from http://statehealthcompare.shadac.org/trend/172/percent-of-privatesector-employees-enrolled-in-highdeductible-health-insurance-plans-by-total#0/1,4/a/5,6,7,8,15,24,25/205
Blog & News
Understanding the New CPS Processing System and New 2018 Health Insurance Coverage Estimates
November 01, 2022:On Tuesday, September 10th, the U.S. Census Bureau released estimates of income, poverty, and health insurance coverage for 2018 from two large-scale federal data surveys conducted annually and administered by the Bureau: the American Community Survey (ACS) and the Current Population Survey Annual Social and Economic Supplement (CPS ASEC). The CPS ASEC is a key source of data on poverty, health insurance coverage, health status, and medical out-of-pocket spending, in addition to a range of other economic and demographic characteristics for the United States population. For information on the ACS estimates see the recently published blog, “National Uninsurance Increased alongside Eight States; Three States Saw Decreases.”
The 2019 CPS ASEC (2018 calendar year estimates) is the first release of a “Production File” to feature a new data processing system that takes into account changes made to the health insurance questions in the 2014 CPS ASEC redesign. Changes include the addition of new variables related to types of coverage that a person held at the time of interview, Marketplace coverage, and sub-annual coverage.[1] For a detailed discussion of these changes, please see several papers produced by the Census Bureau that are available here. This blog briefly discusses the implication of the new processing system on the ability to trend estimates of health insurance coverage.
According to Census, health insurance estimates created using the new processing system should not be compared with estimates produced using the old processing system.1 Currently, the Census Bureau has released three files that that were produced using the new processing system: the 2017 CPS ASEC Research File, the 2018 CPS ASEC Bridge File, and the 2019 CPS ASEC Production File. The Census Bureau publication released this past week—“Health Insurance Coverage in the United States, 2018”—compares the calendar year 2018 health insurance estimates from the 2019 CPS ASEC Production File with the calendar year 2017 estimates from the 2018 Bridge File because both of these files use the new processing system.
The table below illustrates the importance of distinguishing between estimates of health insurance coverage produced by the old versus the new processing system.
Sources: The uninsurance estimates are from “Health Insurance Coverage in the United States, 2018” and “Health Insurance Coverage in the United States, 2017”.
For example, when comparing estimates of the 2017 national uninsured rate, the old processing system (2018 Production File) produces an estimate of 8.8 percent, while the new processing system (2018 Bridge File) produces an estimate of 7.9 percent, nearly a whole percentage point lower. When examining changes in the uninsured rate between 2017 and 2018, the Census Bureau uses the 2017 estimate from the 2018 Bridge File (7.9 percent), created using the new processing system, to compare against the 2018 estimate from the 2019 Production File (8.5 percent), also created using the new processing system.
Using only estimates from data produced by the new processing system thus allows for a true apples-to-apples comparison.
[1] Notes.
New variables: The Research and Bridge Files and the 2019 CPS ASEC contain several additional variables based on new content added to the survey, including variables related to Marketplace-purchased individual coverage (i.e., if coverage was purchased from Marketplace and if the individual received a tax subsidy), concurrent coverage, and variables based on alternative definitions of medical out-of-pocket expenditures.
Sub-annual coverage: Sub-annual coverage variables (i.e., if a person was covered for none, some, or all of the previous calendar year) are available for any coverage, private coverage, government coverage, and Medicaid coverage. Sub-annual coverage data are used to determine if a person had any coverage during the calendar year. Berchick, E.R., Barnett, J.C., and Upton, R.D. (2019). Health Insurance Coverage in the United States, 2018 [Report P60-267]. Retrieved from https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-267.pdf
Blog & News
2018 ACS: National Uninsurance Increased alongside Eight States; Three States Saw Decreases (Infographic)
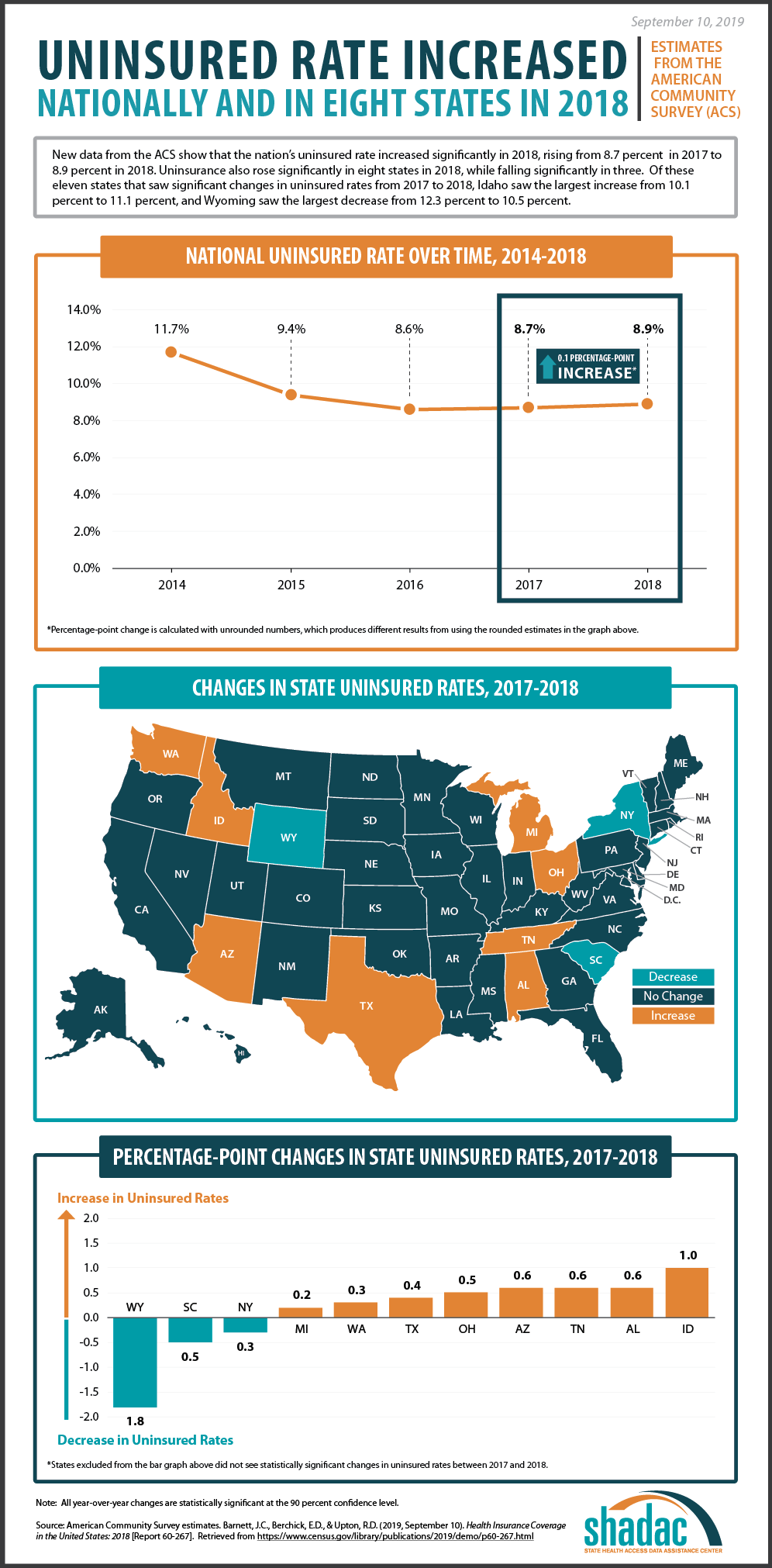
September 10, 2019:New health insurance coverage estimates from the U.S. Census Bureau’s American Community Survey (ACS) show that the rate of uninsured individuals in the United States increased by 0.1 percentage points in 2018, representing 535,000 more Americans without health insurance coverage as compared to 2017. Rates of uninsurance also increased significantly in eight states, and rates decreased significantly in just three states.
Changes in Uninsurance from 2017 to 2018
Nationally, uninsurance increased from 8.7 percent to 8.9 percent from 2017 to 2018, according to new estimates from the ACS.
Eight states saw significant increases in uninsurance from 2017 to 2018, including Alabama, Arizona, Idaho, Michigan, Ohio, Tennessee, Texas, and Washington (Table 1). Among these states, Idaho saw the largest increase in uninsurance, at 1.0 percentage points.
Michigan and Washington experienced the smallest increases in uninsurance, at 0.2 and 0.3 percentage points. 2018 increases in uninsurance in Ohio and Tennessee follow previous increases in uninsurance in these states from 2016 to 2017.
| State | 2017 Percent Uninsured | 2018 Percent Uninsured |
Percentage-Point Change, 2017-2018* |
| Idaho | 10.1 | 11.1 | 1.0 |
| Alabama | 9.4 | 10.0 | 0.6 |
| Tennessee | 9.5 | 10.1 | 0.6 |
| Arizona | 10.1 | 10.6 | 0.6 |
| Ohio | 6.0 | 6.5 | 0.5 |
| Texas | 17.3 | 17.7 | 0.4 |
| Washington | 6.1 | 6.4 | 0.3 |
| Michigan | 5.2 | 5.4 | 0.2 |
| United States | 8.7 | 8.9 | 0.1 |
| New York | 5.7 | 5.4 | -0.3 |
| South Carolina | 11.0 | 10.5 | -0.5 |
| Wyoming | 12.3 | 10.5 | -1.8 |
*Differences are calculated with unrounded numbers, which may produce different results from using the rounded values in the table.
Source. U.S. Census Bureau analysis of the American Community Survey. Health Insurance Coverage in the United States: 2018 [Report P60-267]. Table 6: Percentage of People Without Health Insurance Coverage by State: 2017 and 2018 [Excel file]. Retrieved from https://www.census.gov/data/tables/2019/demo/health-insurance/p60-267.html
Three states—New York, South Carolina, and Wyoming—each experienced statistically significant decreases in uninsurance from 2017 to 2018.
Of these states, Wyoming saw the largest drop in uninsurance at 1.8 percentage points. South Carolina also experienced a 0.5 percentage-point drop in uninsurance from 11.0 percent to 10.5 percent, reversing the significant increase experienced by the state from 2016 (10.0 percent) to 2017 (11.0 percent). New York also experienced a slightly smaller decrease of 0.3 percentage points in uninsured rates, from 5.7 percent in 2017 to 5.4 percent in 2018.
Uninsurance Levels in 2018
Texas continued to have the highest uninsured rate in 2018 at 17.7 percent—a 0.4 percentage-point increase from 17.3 percent in 2017.
The state with the lowest uninsured rate for 2018 was again Massachusetts, holding steady at 2.8 percent.
Among states that expanded Medicaid, Arizona, Michigan, Ohio, and Washington, saw increases in uninsurance, while only New York saw a decrease. State-level uninsured rates among expansion states ranged from a low of 2.8 percent in Massachusetts to a high of 12.6 percent in Alaska.
Overall, among states that did not expand Medicaid, Alabama, Idaho, Texas, and Tennessee each experienced an increase in uninsurance, while South Carolina and Wyoming experienced significant decreases. Individual state uninsured rates among non-expansion states ranged from a low of 5.5 percent in Wisconsin to a high of 17.7 percent in Texas.
SHADAC and Census Bureau Experts Will Share Insights during October 1st Webinar
On Tuesday, October 1st at 12:00 PM Central Time (1:00 PM Eastern), SHADAC will host a webinar to examine the new 2018 ACS and CPS estimates, with technical insight provided by researchers from SHADAC and from the U.S. Census Bureau, which administers both surveys.
Speakers will discuss the new national and state-level estimates, and attendees will learn:
- When to use which estimates from which survey
- How to access the estimates via Census reports and the new data.census.gov site
- How to access state-level estimates from the ACS using SHADAC tables
Attendees will have an opportunity to ask questions after the speaker presentations.
Notes
All differences described here are significant at the 90% confidence level.
All estimates are from the 2017 and 2018 American Community Surveys, as published here: https://www.census.gov/data/tables/2019/demo/health-insurance/p60-267.html
Publication
October 1st Webinar - An Annual Conversation with the U.S. Census Bureau: New Coverage Data from the ACS & CPS on the New Site for Census Bureau Data
Date: October 1, 2019
Time: 12:00 p.m. - 1:00 p.m. Central / 1:00 p.m. - 2:00 p.m. Eastern
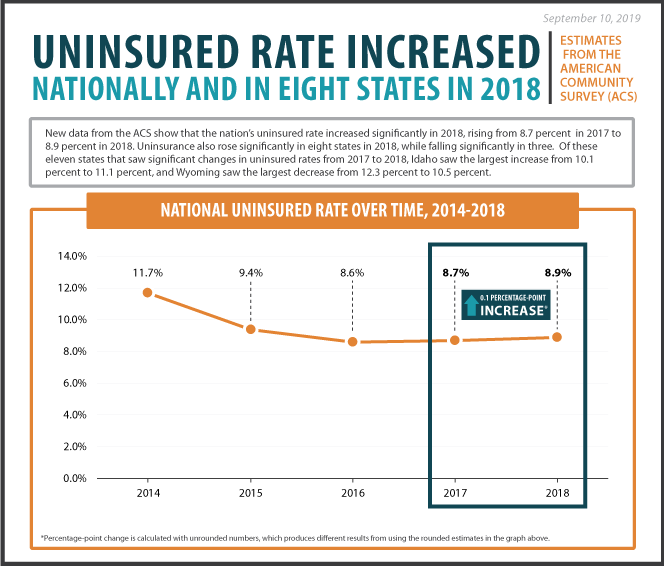 New 2018 data on health insurance coverage from the American Community Survey (ACS) show a nationwide increase in uninsurance from 8.7 percent in 2017 to 8.9 percent in 2018. State-level estimates within the ACS indicated uninsurance also grew significantly in eight states while decreasing significantly in just three.
New 2018 data on health insurance coverage from the American Community Survey (ACS) show a nationwide increase in uninsurance from 8.7 percent in 2017 to 8.9 percent in 2018. State-level estimates within the ACS indicated uninsurance also grew significantly in eight states while decreasing significantly in just three.
SHADAC hosted a webinar on Tuesday, October 1st, examining the new 2018 health insurance coverage data from both the ACS and the Current Population Survey Annual Social and Economic Supplement (CPS ASEC), along with additional national and state-level ACS estimates of health insurance by coverage type released on Thursday, September 26th and those yet to be released on Thursday, October 17th.
SHADAC researchers were joined by experts at the U.S. Census Bureau,
which administers both the ACS and the CPS, and attendees learned about:
The new 2018 national and state coverage estimates
When to use which estimates from which survey
How to access the estimates via Census reports and the new site: data.census.gov
How to access state-level estimates from the ACS using SHADAC tables
SHADAC researchers and Census experts also answered questions from attendees after the presentation.
Slides from the webinar, as well as a transcript, are available for download.
Event Resources
2018 ACS: National Uninsurance Increased alongside Eight States; Three States Saw Decreases (SHADAC Blog and Infographic)
2018 ACS: Private Coverage Changes Split Evenly among States, Public Coverage Changes Experience Greater Variability than in 2017 (SHADAC Blog and Infographic)
SHADAC's State Health Compare (Data Dissemination Site)
2017 ACS Tables: State and County Uninsured Rates, with Comparison Year 2016 (SHADAC Resource)
U.S. Census Bureau: Health Insurance (Data Dissemination Site)
U.S. Census Bureau Health Insurance (PDF Report)
U.S. Census Bureau Statistical Testing Tool
U.S. Census Bureau Explore Census Data (Data Dissemination Site)