Blog & News
The Children's Health Insurance Program: A Minnesota Perspective
January 22, 2018:Congress has still not fully reauthorized the Children’s Health Insurance Program (CHIP), and states are working to figure out how to keep their kids covered. CHIP provides essential coverage for millions of our nation’s poorest children and should not be used as a bargaining tool in federal budget negotiations. It’s time to put politics aside and reauthorize this program that is vital for vulnerable children and that both sides ofthe aisle claim to support.
Minnesota: A Pioneer in Covering Kids
Minnesota, as a national leader in health care, has a long history of providing coverage for its children--well before the passage of the federal CHIP program. As far back as 1987, Minnesota provided coverage to low-income children who were just above the income level to qualify for Medicaid, and we paid for it with state funds alone. The program initially covered physician services for children under age six and low-income pregnant women who were not Medicaid-eligible. The state financed the program through an annual fee of $35 for pregnant women and $25 for children, and a one-cent tax on cigarette packs.
In 1991, Minnesota's public coverage for kids was expanded to all children under age 18, and in 1992, Governor Carlson passed comprehensive health reform legislation, the HealthRight Act, with broad bipartisan support. Renamed MinnesotaCare, the state's public coverage program provided subsidized health insurance for working families with incomes just above Medicaid eligibility levels (up to 275% of the Federal Poverty Level) who not eligible for employer-sponsored insurance. The program continued to be funded with state-only dollars, and the legislation behind it included earmarked funding from a new 2% provider tax, a 1% health insurance premium tax, as well as a five-cent increase in the cigarette tax.
Early analyses of the impact of MinnesotaCare found that between 1990 and 1995 the proportion of uninsured children (uninsured for 12 months or longer) in Minnesota decreased from 5.2% to 3.1%. This change translated to an increase in access to care for kids and a reduction in the amount of free care given by medical providers to the uninsured.
CHIP's Evolving Role in Minnesota and the Nation
Minnesota and other states that had similarly funded their own safety net programs were thrilled when CHIP passed in 1997. Modeled in part on the Minnesota program, CHIP targeted families just above the eligibility level for Medicaid and provided needed support to low-income working families. In its early years, CHIP funded very few of Minnesota’s low-income children, as the program was targeted to states with larger numbers of uninsured children; in fact, a report from 2000 showed only 8 children in Minnesota covered by CHIP. However, Minnesota leveraged CHIP funding over time, and today Minnesota uses its CHIP dollars to support coverage for 127,000 children and pregnant women. Nationwide, the program is now well-established and covers close to 9 million children.
The Uncertain Future of CHIP Puts the Most Vulnerable at Risk
Minnesota’s goal has always been to get and keep children and their families insured. We know that providing health insurance coverage enhances children’s school performance, increases parents’ work attendance, improves and sustains high immunization rates, and advances the health and economic future of children as they age into adulthood. Most of all, coverage assures that all have an opportunity to pursue their goals and aspirations in life.
Both the delay in the CHIP reauthorization and the real potential for no future funding affects the most vulnerable: poor children. It’s hard to believe, but close to one in every four children in this country lives in poverty. For African American children, the rate is over 40%.
States Employing Stopgap Measures
With the end of CHIP’s authorization on September 30th, states have been able to apply for emergency funding to keep their programs going. Oregon and Minnesota have both pledged to make up what they hope is a temporary funding gap with state dollars, but it puts their finances in jeopardy — Minnesota’s latest budget projection released in early December includes a $188 million shortfall if CHIP is not reauthorized. Meanwhile, other states will need to shut down new enrollment and start notifying families of potential loss of coverage.
In the meantime, the stress to families of not knowing if coverage will continue and for how long, is real. States are scrambling to keep kids covered — making tremendous efforts to find alternative funding, notifying families of the potential phase out of the program, and placing limits on new enrollment in anticipation of a lack of funding.
Funding CHIP: A No-Brainer and the Right Thing to Do
Lynn A. Blewett, PhD, MPA, is Professor of Health Policy at the University of Minnesota, School of Public Health
Blog & News
Minnesota's 2018 Preliminary Individual Market Premium Rate Filings in Context: News Is Good but Challenges Remain
August 21, 2017:From the Desk of Lynn Blewett
Minnesota insurance companies filed their preliminary premium rates for plans sold on the individual health insurance market. The rate increases for 2018 are much lower than the rate increases seen last year when premiums increases were as high as 50 to 67 percent. This blog provides my initial impressions on the preliminary rate increases for 2018 and additional context to understand the dynamics of a rapidly evolving health insurance market.
Minnesota’s individual health insurance market is in a state of flux with the implementation of the Affordable Care Act (ACA). Individuals without access to employer-sponsored insurance and without access to the premium subsidies offered through MNsure faced exorbitant, and for some, unaffordable, health insurance premiums in 2016. This crisis prompted the Minnesota legislature to pass two pieces of significant legislation last session. The Health Insurance Premium Relief bill provided enrollees with rebates to health plans, with the requirement that quoted premium prices would be reduced by 25%. The Premium Security Plan established a reinsurance plan to provide additional premium relief and stabilize the premiums in the individual market. Together, the legislature authorized nearly $1 billion in support of the individual health insurance market.
Rate Increases with and without Reinsurance
The rate increases for 2018 are presented in the table below. Rate increases with reinsurance ranged from a 14.5 percent decrease in premiums submitted by UCare to an 11.4 percent increase in rates submitted by Blue Plus. Without reinsurance, the rate increases ranged from a 3.3 percent increase in rates submitted by Group Health to a 31.7 percent increase submitted by Blue Plus.
| Proposed 2018 Individual Market Health Insurance Rates for Minnesota | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Insurer |
Proposed Average Change with Reinsurance |
Proposed Average Change without Reinsurance |
|||||||||
| Blue Plus | -1.5% | to | +11.4% | +16.4% | to | +31.7% | |||||
| Group Health* | -14.5% | to | -13.4% | +3.3% | to | +4.6% | |||||
| Medica Insurance Company* | -5.3% | to | +5.3% | +15.4% | to | +29.4% | |||||
| PreferredOne Insurance Company^ | -40.8% | to | -36.8% | -25.5% | to | -20.6% | |||||
| UCare | -14.5% | +9.4% | |||||||||
| *Current HealthPartners Insurance Company enrollees will default renew into Group Health, and current Medica Health Plans of Wisconsin enrollees will default renew into Medica Insurance Company. A consumer is not required to accept the default renewal plan and may select any plan from any insurer during open enrollment. | |||||||||||
| ^PreferredOne Insurance Compnay left the Minnesota individual market in 2015 and is not offering new insurance products. | |||||||||||
| Source: 2018 Proposed Health Insurance Rates,” Minnesota Department of Commerce, July 31, 2017. | |||||||||||
| State 1332 Innovation Waivers | ||
|---|---|---|
|
Section 1332 of the Affordable Care Act provides the opportunity for states to propose innovative strategies around the access expansions included in the ACA—including the Medicaid expansion and the premium subsidies provided through tax credit for those buying on the exchange within certain income limits. The plans must be approved by both the Secretary of Health and Human Services and by the Department of the Treasury; must provide at least the level of coverage provided under the ACA; and may not increase the federal deficit. The waivers are approved for five-year periods. State-based reinsurance represents one of the first policy strategies being implemented to stabilize the individual market. Reinsurance also represents a key policy strategy of interest to CMS as evidenced by a March 13, 2017 communication from HHS Secretary Price, sent to each Governor, encouraging states to consider using the 1332 waiver opportunity to implement reinsurance programs and making specific reference to the Alaska reinsurance approach. Alaska's Reinsurance Approach Alaska’s 1332 waiver proposal to establish a reinsurance program was recently approved by the federal government. Alaska’s reinsurance plan is financed through assessments on private health insurers with additional federal funding of $332 million over a five-year period. Alaska uses a condition-specific reinsurance approach that provides 100 percent of the cost of all claims for policyholders that have one of 33 pre-existing conditions. Pass-Through Funding Alaska's waiver, and Minnesota's waiver proposal, uses “pass through” federal dollars—funding that otherwise would be used for the subsidies offered on the Health Insurance Marketplace, namely the Advanced Premium Tax Credits (APTC) and the Consumer Cost-Sharing Reductions (CSRs). Because premiums are expected to go down under reinsurance, the subsidies required to fund the APTCs and the CSRs would be reduced, and the amount of savings from reduced subsidies would be “passed through” to the state to help fund its reinsurance program. Each state must estimate the amount of federal savings achieved through reinsurance and include this in its waiver application. |
Minnesota’s Reinsurance Proposal
Insurance companies buy reinsurance to reduce the volatility in their costs and provide stability to premiums. Reinsurance is basically insurance for insurance companies and is standard practice for different types of insurance products, not just health care. There are different models of reinsurance, and Minnesota is one of five states with current reinsurance proposals for health insurance offered in the individual market.
Minnesota proposed a publicly-funded reinsurance program using a claims corridor approach. The reinsurance company will reimburse insurers at an 80%/20% coinsurance rate for claims that fall between $50,000 and $250,000. Instead of the insurers covering the costs of reinsurance, the state has proposed public financing with an appropriation of $271 million per year for two years—a total of $542 million for the biennium.
The legislatively-created Minnesota Comprehensive Health Association would serve as the administrator of the reinsurance product, using state funds appropriated to the commissioner of commerce. The legislative language authorizing the reinsurance program requires federal approval of a State Innovation Waiver (a 1332 waiver), which was submitted on May 5, 2017. Under this waiver, Minnesota has proposed that the federal government pay about a third of the cost of the reinsurance program, with tthe federal government contributing between $138 million and $167 million toward the $270 million total cost of the program each year.
My Initial Thoughts
In general, the 2018 preliminary insurance rate filings are great news. Minnesota’s individual market is relatively small (about 300,000 pre-ACA and 170,000 in 2017), and implementing insurance reforms was difficult. The premiums in the individual market started low but over time had to catch up with increases in costs. Many of the premiums filed last year increased by more than 50% from 2016. The first look at the preliminary 2018 rates with limited increases, and in some cases decreases, was welcome.
There is also some hope that Secretary Price will approve Minnesota’s 1332 State Innovation Waiver. He recently approved the waiver proposal submitted by the state of Alaska, and the Minnesota approach to reinsurance is relatively straightforward. Governor Dayton recently met with Secretary Price, and the meeting reportedly went well.
However, there continues to be uncertainty at the federal level in terms of conflicting messaging around federal funding of CSRs and enforcement of the individual mandate, and the broader political debate about the ACA’s future has further escalated insurers’ concerns. These factors, in turn, have led to the exit of insurers from local markets or entire states, exceedingly high increases in premiums, and fewer plan choices for consumers.
Here are a few of my initial concerns.
- The legislature funded reinsurance for just two years, and reinsurance is likely to be an ongoing need. The state appropriated funding for just two years using funds from the Health Care Access Fund. If state-based reinsurance will be an ongoing need, and I suspect it will, a new source of funds will need to be found.
- Financing of reinsurance uses funding from Minnesota's Health Care Access Fund (HCAF), which may soon be needed to support the state's safety net. Typically, reinsurance is funded by assessments on private insurers to cede a portion of their risk to another insurance company. The temporary reinsurance program provided in the ACA and the more recent Alaska reinsurance program were both funded with assessments on the insurance carriers.
The HCAF comes from a two percent fee on most health care providers’ bills. The HCAF was initially established to fund MinnesotaCare, which was designed to support health insurance coverage for Minnesotans whose incomes fell just above the Medicaid income limits. The target population was Minnesota families working in low-wage jobs with no access to employer-based health insurance. MinnesotaCare provided needed coverage and limited premiums based on income, and providers who once provided care without payment now received reimbursement for their services.
Minnesota was fortunate to move into the 2017 legislative session with a $1.6 billion dollar surplus, allowing the legislature to fund different programs including the premium rebates described above. Yet given the uncertainty at the federal level and discussions of cuts to safety net programs such as Medicaid, the HCAF may be needed in the near future to support the safety net in Minnesota as initially intended. For long-term funding of reinsurance, alternative financing should be considered, including fees assessed on the insurance carriers.
- The 105,000 people purchasing coverage on MNsure who got a 25 percent rebate on their premiums this year will likely see some increase in their premiums next year, even with reinsurance. The premium increases cited in the table above are based on last year’s base premiums without the 25 percent premium rebate adjustment. For example, a person facing a $1,000 a month premium in 2017 received a 25 percent rebate, bringing their 2017 premium to $750. But even with no premium increase for 2018, the individual would be back to the $1,000 premium, which represents a 33% increase.
In general, rates will remain flat for most people who purchase coverage on Minnesota's health insurance exchange, MNsure: Premium increases will not be felt by the 85 percent of people who are income-eligible (i.e., with an income of $24,000 to $48,680 annually for a family of four) for Advanced Premium Tax Credit subsidies to bring down the cost of their monthly premiums: Because the amount of the subsidy is based on household income, such that no individual will pay more than 9.6 percent of income on health insurance premiums, premium rate increases are absorbed by the premium subsidy. However, broad premium decreases for this segment of the MNsure population won't happen, either.
- We still do not know if every Minnesota county will have options to purchase coverage in the individual market. And we do not know what the provider networks look like. Last year, the networks were tighter, and some of the pairings of hospitals and clinics did not facilitate the best geographical access. So, we still need to see what the plans look like and if all counties are covered.
- The PreferredOne products with the largest declines in premiums are not offered on Minnesota's individual market for new enrollees. These are the products that have retained enrollees since PreferredOne abruptly left the individual market in 2015. They are not offering new products.Technically, PreferredOne should not be included on this list because its products are not currently offered on the individual market.
States like Minnesota and Alaska are forging ahead and making decisions to assure that people have access to affordable coverage. We are out in front of the pack but still have work to do.
Blog & News
How Would an ACA Repeal Affect Minnesota?
May 11, 2017:A new SHADAC brief examines the implications of an Affordable Care Act repeal for Minnesota. The authors, SHADAC Research Assistant Robert Hest and SHADAC Director Lynn Blewett, present an overview of the the impact of the ACA's coverage expansions in the state and highlight the potential for losses with a repeal. They look specifically at rates of health insurance coverage, hospital uncompensated care, and levels of federal health funding for Minnesota's public coverage programs.
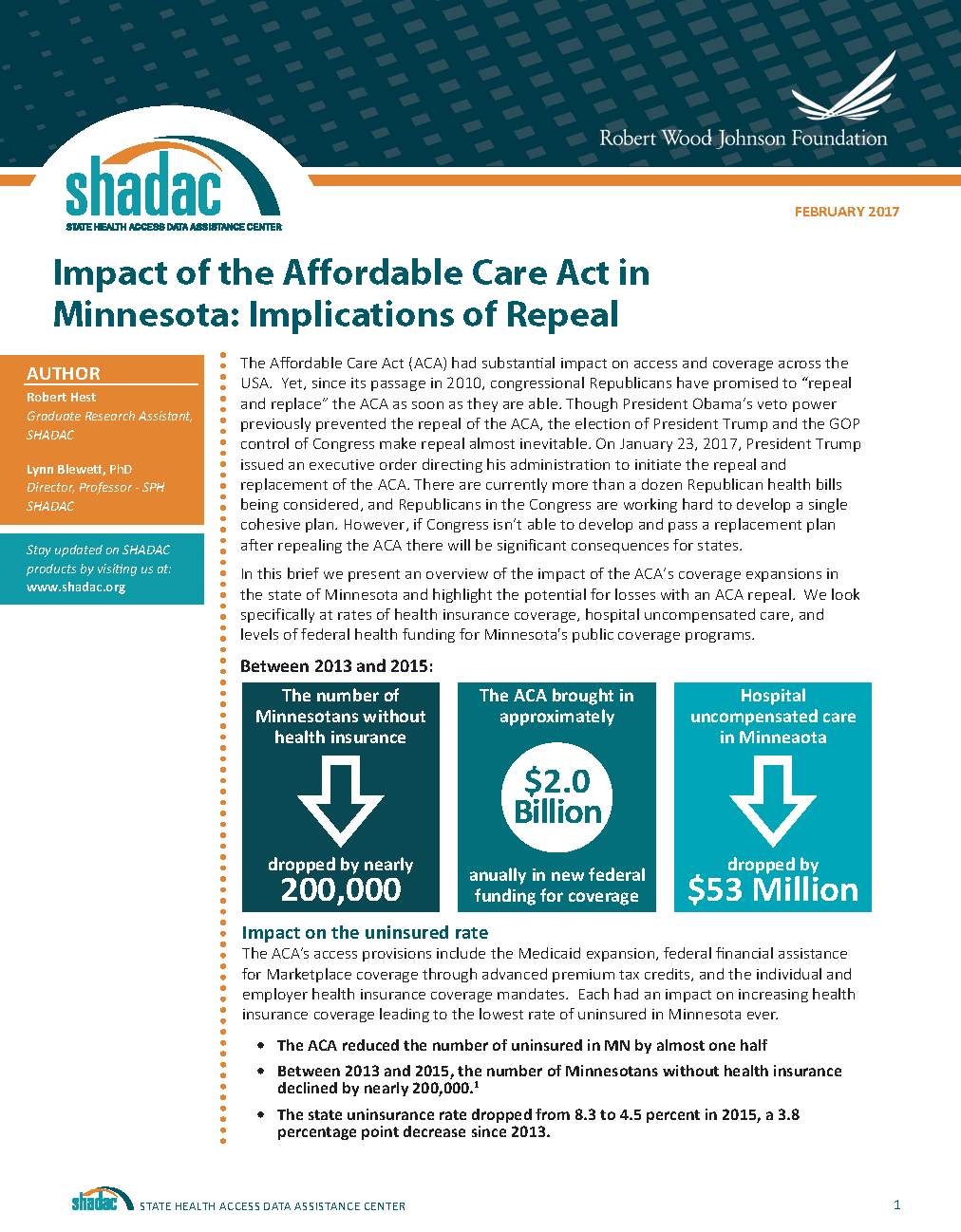 The authors point out that between 2013 and 2015
The authors point out that between 2013 and 2015
- The ACA reduced the number of uninsured in Minnesota by nearly 200,000 (almost one half), bringing the state's uninsurance rate down to 4.5 percent from 8.3 percent. 1
- Minnesota's hospital uncompensated care fell by $53 million (a 16.7 percent decrease). 2
With an ACA repeal
- The number of uninsured Minnesotans would more than double. 3
- Minnesota's hospital uncompensated care would increase by an estimated $548 million by 2019. 4
The authors also emphasize that individuals enrolled in health plans through MNsure received an estimated $115 million in tax credits and cost-sharing reductions from the federal government in 2016--funds that would no longer be available with an ACA repeal. 5 Moreover, the State of Minnesota stands to lose the $2 billion in annual federal funding that it currently receives for Medical Assistance and MinnesotaCare, along with $80.8 million in federal Preventional and Public Health fund grants. 6, 7
1 SHADAC Analysis of the 2013-2015 American Community Survey
2 Minnesota Department of Health: Health Economics Program. "Uncompensated Care at Minnesota Hospitals Drops for the Second Year in a Row," October 31, 2016. http://www.health.state.mn.us/news/pressrel/2016/costs103116.pdf
3 SHADAC Analysis of the 2015 American Community Survey
4 Buettgens, M., Blumber, L., & Holahan, J. "The Impact on Health Care PRoviders of Partial ACA Repeal through Reconciliation," Urban Institute, January 2017. http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2017/rwjf433621
5 Kaiser Family Foundation. "Estimated Total PRemium Tax Credits Received by Marketplace Enrollees," March 31, 2016. http://kff.org/health-reform/state-indicator/average-monthly-advance-premium-tax-credit-aptc/
6 Minnesota Department of Human Services. "Repealing the Affordable Care Act: Impacts to Minnesota's Public Healthcare Programs," January 6, 2017. http://mn.gov/dhs/aca-repeal/issue-brief/
7 Trust for America's Health. "Minnesota Could Lose More than $80 Million to Fight Health Epidemics over Five Years if the ACA and Prevention and Public Health Fund Are Repealed," 2017. http://healthyamericans.org/reports/prevention-fund-state-facts-2017/release.php?stateid=MN
Blog & News
SHARE Research at ASHEcon 2016
June 15, 2016:Seven research teams are presenting their SHARE-funded work at the 2016 American Society of Health Economics Conference (ASHEcon), which takes place this year at the Leonard Davis Institute for Health Economics at the University of Pennsylvania from June 12th through the 15th. We encourage you to check out these presentations if you’re attending the conference.
Podium presentations of SHARE-funded research at ASHEcon 2016 are as follows:
Early Evidence on Employment Responses to the Affordable Care Act
Speaker: Jean Abraham (University of Minnesota)
Discussant: Laura Dague (Texas A&M)
Date/Time: Monday (6/13), 10:55 a.m.
Location: G50 (Huntsman Hall)
As the insurance market changes with the implementation of the ACA, this research examines how the existence of employer-based health insurance coverage impacts employees’ access to such insurance as well as labor market outcomes, such as part-time work. Researchers investigate how labor market outcomes are changing over time as the ACA is implemented.
Speaker: Pinar Karaca-Mandic (University of Minnesota)
Discussant: Anthony LoSasso (University of Illinois at Chicago)
Date/Time: Monday (6/13), 5:25 p.m.
Location: B26 (Stiteler Hall)
This research documents the relationship between television media campaigns and health insurance enrollment, as federal and state governments, as well as nonprofit organizations, spent over $3 billion on media advertising to promote newly available insurance through ACA marketplaces in the first open enrollment period.
Choice Dynamics of “Money Wasting” Plan Choices in ACA State Marketplaces
Speaker: Anna Sinaiko (Harvard University)
Discussant: Chapin White (RAND)
Date/Time: Wednesday (6/15), 8:50 a.m.
Location: G60 (Huntsman Hall)
This research examines the decisions made by people, particularly members of vulnerable populations, in choosing health insurance plans that potentially result in wasted money. The researchers surveyed enrollees in the ACA marketplace in 2015 to determine whether enrollees were enrolled in the most cost effective plan.
Speaker: Lindsay M. Sabik (Virginia Commonwealth University)
Discussant: Ari B. Friedman (University of Pennsylvania)
Date/Time: Wednesday (6/15), 9:10 a.m.
Location: G50 (Huntsman Hall)
This study examines the impact of early Medicaid expansion in California on admissions of patients at safety net hospitals, defined as hospitals that serve a disproportionately high number of uninsured and Medicaid patients. By comparing California hospital admissions from 2010-2013 to other states that did not experience significant changes to their Medicaid coverage during this time period, the researchers find that both safety net and non-safety net hospitals in California experienced an increase in Medicaid patient admissions and decreases in uninsured admissions.
Pent-up Health Care Demand Among New Medicaid Enrollees after the Affordable Care Act
Speaker: Angela Fertig (Medica Research Institute)
Discussant: James Marton (Georgia State University)
Date/Time: Wednesday (6/15), 12:40 p.m.
Location: F55 (Huntsman Hall)
This study examines claims data for evidence of pent-up demand for health care, meaning that newly insured individuals access care at higher rates due to delaying or foregoing care while uninsured or underinsured, for new Medicaid enrollees in Minnesota.
Poster presentations of SHARE-funded research at ASHEcon 2016 are as follows:
Specialty Drug Benefit Design and Patient Out-of-Pocket Costs in the ACA Health Insurance Exchanges
Speaker: Erin A.Taylor (RAND)
Date/Time: Tuesday (6/14), 12:00 p.m.
Location: Annenberg Center, Lobby
Insurers often require more cost sharing from patients for high-cost specialty drugs, meaning that patients end up paying more money out-of-pocket for these drugs than they would for other drugs. This research simulates potential out-of-pocket costs in health exchange plans for patients taking three specialty drugs.
Speaker: Michael Dworsky
Date/Time: Tuesday (6/14), 12:00 p.m.
Location: Annenberg Center, Lobby
Overview: This research examines the impact of the ACA’s Medicaid expansion on insurance status and type of coverage for adults who became newly eligible for Medicaid in 2014. The researchers use 2009 – 2014 data from the National Health Interview Survey to estimate the effect of Medicaid expansion on insurance status, and compare states that chose to expand Medicaid coverage to states that chose not to do so. They find that expanding Medicaid to non-disabled childless adults in poverty reduced uninsurance rates without impacting the number of enrollees on private market plans.
Blog & News
New Brief: Using HCUP Data for State Health Policy Analysis
May 12, 2017: The SHARE grant program has released a new brief examining the use of administrative data for the purpose of state health policy analysis. In particular, the brief highlights the hospital administrative data available from the Healthcare Cost and Utilization Project (HCUP) and presents a case study of a SHARE-funded project that uses HCUP data to evaluate the impacts of California’s early ACA Medicaid expansion on inpatient hospital utilization.
The SHARE grant program has released a new brief examining the use of administrative data for the purpose of state health policy analysis. In particular, the brief highlights the hospital administrative data available from the Healthcare Cost and Utilization Project (HCUP) and presents a case study of a SHARE-funded project that uses HCUP data to evaluate the impacts of California’s early ACA Medicaid expansion on inpatient hospital utilization.
What is the HCUP?
The HCUP is a collection of six different databases sponsored by the federal Agency for Healthcare Research and Quality (AHRQ) that can be purchased through the HCUP Central Distributor. These databases consist of longitudinal hospital data—with a primary focus on community hospitals--based on de-identified discharge records for individual patients. The six different HCUP databases are:
- • National Inpatient Sample (NIS)
- • Kids’ Inpatient Database (KID)
- • Nationwide Emergency Department Sample (NEDS)
- • Nationwide Readmissions Database (NRD)
- • State Inpatient Databases (SID)
- • State Emergency Department Databases (SEDD)
Using HCUP Data to Examine State-Level Utilization
For state-focused health policy research, the State Inpatient Databases (SID), which consist of hospital inpatient discharge data on approximately 90 percent of all U.S. hospital discharges, are especially useful for understanding patient utilization. The SID not only allow researchers to examine hospital-level differences within states but also foster multi-state comparisons and analyses because of their uniformity.
Case Study: Early Medicaid Expansion in California
Researchers at Virginia Commonwealth University (VCU), led by Dr. Peter Cunningham, used the SID to examine the utilization impact of California’s early Medicaid expansion. Specifically, the research team compared
- Utilization at hospitals in California from 2010 to 2013 with utilization at hospitals in neighboring states without an early Medicaid expansion, and
- Utilization over the same time period at safety net and non-safety net hospitals within California.
Preliminary Findings: Highlights
Preliminary findings from the VCU study include (among others):
- • Inpatient volumes increased at California hospitals relative to the comparison states following California’s Medicaid expansion, when controlling for national trends.
- • Medicaid admissions as a percent of total admissions increased after California’s Medicaid expansion, while uninsured admissions declined when compared to non-expansion states (again, controlling for national trends).
- • Overall inpatient volumes at safety net hospitals within California increased to a greater extent than at the state’s non-safety net hospitals following the early Medicaid expansion.
- • Both safety net and non-safety net hospitals within California observed similar patterns in payer mix after the Medicaid expansion, with an increase in Medicaid admissions as a percent of total admissions and a decrease in uninsured admissions as a percent of total admissions.
Further Details
For more information on the HCUP, the SID, and preliminary findings from the VCU study, view the full issue brief: “Using HCUP Data for State Health Policy Analysis: A Case Study Examining the Impacts of an Early Medicaid Expansion.”