Blog & News
Brett Fried: Expanding access to health care coverage critical to reducing a state's uninsurance rate (Cross-Post)
November 19, 2015:The following content is cross-posted from Health Talk, the blog of the University of Minnestoa's Academic Health Center. It was first published November 10, 2015, and posted by Matt DePoint:
Photo: New York Times http://www.nytimes.com/interactive/2015/10/31/upshot/who-still-doesnt-have-health-insurance-obamacare.html?emc=edit_th_20151101&nl=todaysheadlines&nlid=20932956&_r=2
According to a recent New York Times article, the majority of people who remain uninsured after the Affordable Care Act (ACA) was implemented in the United States live in the South and Southwest and they tend to be poor.
But why is this the case?
Health Talk spoke with Brett Fried, a senior research fellow at the State Health Access Data Assistance Center (SHADAC), to learn more about why there are such glaring differences in uninsurance rates across the United States.
Health Talk (HT): There is a distinct difference geographically in the NYT map. Why do you think this is?
Brett Fried (BF): As mentioned in the New York Times article, whether a given state chose to expand Medicaid seems to be the major driver of how many people remain uninsured the state. This association is consistent with recently released data from the National Center for Health Statistics (NCHS): These data show that, compared with non-expansion states, the percentage of uninsured non-elderly adults in Medicaid expansion states was generally lower and declined more dramatically between 2013 and the first quarter of 2015 (with an average drop of 7.8 percentage points in the expansion states and an average drop of 5.9 percentage points in non-expansion states).
HT: What is Minnesota doing well compared to other states?
BF: Minnesota has a long history of reform, including pre-ACA coverage expansions, which contributed to relatively low rates of uninsurance even before federal reform. Minnesota continued this tradition by implementing the early Medicaid expansion option under the ACA in 2010 (along with only six other states and the District of Columbia) and expanding Medicaid fully in 2014. In addition, Minnesota’s state-based marketplace, MNsure, conducted an intensive outreach and enrollment campaign and funded widespread in-person enrollment assistance. The impacts of these efforts can be seen in the New York Times map, which shows Minnesota already low uninsurance rate declining significantly between 2013 and 2014. This is consistent with U.S. Census Bureau data, which show the Minnesota uninsured rate dropped from 8.2 percent in 2013 to 5.9 percent in 2014.
HT: What can those predominantly southern states learn from Minnesota?
BF: The predominant lesson from Minnesota (and other states) is that a commitment to expanding access to coverage—whether through traditional Medicaid, a Medicaid waiver, or other public coverage programs—is critical to significantly reducing a state’s uninsured rate. While Minnesota has historically been a leader in health reform, resulting in consistently low rates of uninsurance, southern states such as Kentucky and Arkansas that expanded Medicaid under the ACA (the first through an expansion of traditional Medicaid and the second through a Medicaid waiver initiative) also saw dramatic reductions in their rates of uninsured. In fact, Census data show that the uninsurance rate dropped from 14.3 percent to 8.5 percent in Kentucky and from 16.0 percent to 11.8 percent in Arkansas between 2013 and 2014.
HT: Can you explain the role Medicaid expansion and politics plays in the uninsured rates?
BF: Data clearly show the Medicaid expansion has been the driver of coverage gains under the ACA. The Centers for Medicaid and Medicare services reports an increase in 13.6 million additional enrollees between October 2013 and August 2015. While Medicaid enrollment growth occurred in all states, it was driven by states that expanded coverage: Among states that expanded coverage, Medicaid grew by 31 percent between a pre-ACA baseline period and August 2015, compared to 10 percent growth among non-expansion states.
Among the 19 states that have not expanded Medicaid, politics seems be driving the debate around whether to expand. The political debate varies in each state, but opponents of expansion commonly cite: opposition to expanding a “broken system,” a belief that Medicaid reduces the incentive for personal responsibility among enrollees, concerns over the impacts of expansion on state budgets, and a belief that expansion would constitute an infringement on “states’ rights”, among others. In order to gain political support, a handful of states have applied for and received a waiver to expand Medicaid in a non-traditional way. Non-traditional approaches have included implementing expansion through a premium assistance program, charging premiums/contributions, eliminating select required benefits and providing incentives for healthy behaviors.
HT: What can be done to encourage more people to become insured?
BF: It has been commonly reported that states have seen enrollment gains among the “low hanging fruit” and that those who remain uninsured are the “hard to reach.” This seems particularly true for states with very low rates of uninsurance, like Minnesota. A recent SHADAC analysis examined the characteristics of the uninsured in 2013 versus 2014 seems to bear that out: Our analysis shows that compared to the uninsured in 2013, those in 2014 were more concentrated in groups that have consistently been uninsured (e.g. men, Hispanic, non-citizens, those with less education). State data can play in important role in targeting outreach to the uninsured, and to that end, SHADAC provides data to states on the characteristics and location of the remaining eligible for Medicaid and the health insurance marketplaces.
Publication
SHARE Quarterly Update: July - September 2015
SHARE Panel at APPAM Will Consider Early Post-Expansion Utilization Data
 Four researchers will present findings from their SHARE-funded studies on a panel at the 2015 Fall Research Conference hosted by the Association for Public Policy Analysis and Management (APPAM) in Miami, Florida. The panel, titled “Early Data on Health Care Utilization after Coverage Expansion,” will take place on Thursday, November 12th, and will feature presentations from Peter Cunningham (Virginia Commonwealth University), Marguerite Burns (University of Wisconsin – Madison), Angela Fertig (Medica Research Institute), and Michael Dworsky (RAND Corporation). Kathy Hempstead, Coverage Team Director at the Robert Wood Johnson Foundation, and Brett Fried, SHADAC Senior Research Fellow, will act as discussants. Learn more.
Four researchers will present findings from their SHARE-funded studies on a panel at the 2015 Fall Research Conference hosted by the Association for Public Policy Analysis and Management (APPAM) in Miami, Florida. The panel, titled “Early Data on Health Care Utilization after Coverage Expansion,” will take place on Thursday, November 12th, and will feature presentations from Peter Cunningham (Virginia Commonwealth University), Marguerite Burns (University of Wisconsin – Madison), Angela Fertig (Medica Research Institute), and Michael Dworsky (RAND Corporation). Kathy Hempstead, Coverage Team Director at the Robert Wood Johnson Foundation, and Brett Fried, SHADAC Senior Research Fellow, will act as discussants. Learn more.
December 8th Webinar: Analysis of Provider Network Monitoring Practices
 Karen Brodsky and Barbara Markham Smith of Health Management Associates (HMA), will discuss their SHARE-funded analysis of trends in provider network monitoring practices by states and health plans during a December 8th webinar hosted by HMA. They will highlight key findings from a survey of health plans and state regulators concerning provider network adequacy compliance and monitoring standards (detailed in an in-depth report here). Based on these findings, they will provide recommendations for states and health plans seeking more effective and efficient ways of ensuring adequate provider access for members. Register for the webinar.
Karen Brodsky and Barbara Markham Smith of Health Management Associates (HMA), will discuss their SHARE-funded analysis of trends in provider network monitoring practices by states and health plans during a December 8th webinar hosted by HMA. They will highlight key findings from a survey of health plans and state regulators concerning provider network adequacy compliance and monitoring standards (detailed in an in-depth report here). Based on these findings, they will provide recommendations for states and health plans seeking more effective and efficient ways of ensuring adequate provider access for members. Register for the webinar.
Sarah Gollust Discusses Geographic Variations in Media Messages about Reform
Dr. Sarah Gollust of the University of Minnesota discussed her SHARE-funded research in a presentation titled, “Media and the Politics of Implementation: Geographic Variation in ACA Coverage,”at the 2015 Annual Meeting of the American Political Science Association (APSA) on September 6th in San Francisco. The presentation focused on an analysis of the geographic variation in the volume and content of televised messages about the ACA from October 2013 through March 2014. The next stage of the project will link patterns of media messaging at the market level to individuals’ attitudes and behavior using national survey data (Kaiser Health Tracking Poll and the National Health Interview Survey).Angie Fertig Finds Evidence Consistent with Pent-Up Demand among New ACA Enrollees
 A new brief from Dr. Angie Fertig at Medica Research Institute highlights initial findings from a SHARE-funded study examining pent-up demand after the ACA. In the brief, Dr. Fertig, with co-authors Dr. Caroline Carlin and Dr. Sharon Long, examines administrative and claims data from a Minnesota health insurer to identify early patterns in the first claim for new Medicaid and commercial non-group (including Marketplace) enrollees who signed up for coverage between January and March 2014. The researchers found patterns of utilization that are consistent with pent-up demand among new Medicaid enrollees. However, the evidence of pent-up demand among new enrollees with non-group coverage relative to the comparison group is mixed.
A new brief from Dr. Angie Fertig at Medica Research Institute highlights initial findings from a SHARE-funded study examining pent-up demand after the ACA. In the brief, Dr. Fertig, with co-authors Dr. Caroline Carlin and Dr. Sharon Long, examines administrative and claims data from a Minnesota health insurer to identify early patterns in the first claim for new Medicaid and commercial non-group (including Marketplace) enrollees who signed up for coverage between January and March 2014. The researchers found patterns of utilization that are consistent with pent-up demand among new Medicaid enrollees. However, the evidence of pent-up demand among new enrollees with non-group coverage relative to the comparison group is mixed. Tal Gross Explains Why Medicaid Expansion Makes Economic Sense
 In a recent video from Columbia University’s Mailman School of Public Health, Dr. Tal Gross summarizes the policy implications of his SHARE-funded analysis of the economic impact of state ACA Medicaid expansion decisions. Dr. Gross and his colleagues at Northwest University found that the amount of money that state governments save from not expanding Medicaid is roughly equal to the amount of money that the hospitals in those states have to spend to care for the uninsured (i.e., their uncompensated care costs). These findings are detailed in Dr. Gross’s recent NBER working paper.
In a recent video from Columbia University’s Mailman School of Public Health, Dr. Tal Gross summarizes the policy implications of his SHARE-funded analysis of the economic impact of state ACA Medicaid expansion decisions. Dr. Gross and his colleagues at Northwest University found that the amount of money that state governments save from not expanding Medicaid is roughly equal to the amount of money that the hospitals in those states have to spend to care for the uninsured (i.e., their uncompensated care costs). These findings are detailed in Dr. Gross’s recent NBER working paper.
V-BID in Connecticut: Early Results Show Beneficial Impact on Utilization
The research team led by Dr. Richard Hirth at the Center for Value-Based Insurance Design (V-BID Center) at the University of Michigan released a brief highlighting initial findings from their SHARE-funded analysis of Connecticut’s Health Enhancement Plan (HEP) for state employees, which reduces cost-sharing for high-value clinical services and targets patient incentives to eliminate barriers to evidence-based care. The authors found significant improvements among HEP enrollees during the first HEP plan year for a variety of standard preventive measures compared to a control group of state employee health plan enrollees in four different states without a comparable intervention. The findings from this brief are highlighted in the podcast of an August 4th webinar that was co-hosted by SHARE and the V-BID Center.
Sarah Gollust, PhD
 Sarah Gollust is the principal investigator on a SHARE-funded project to measure geographic variation in ACA-related media messages and the subsequent relationship of media messages to insurance enrollment from 2013 to 2014. Her broad research interests are in the politics and ethics of health policy, and she is particularly interested in understanding the media’s role in influencing the public’s opinions and perceptions of health policy issues. Learn more.
Sarah Gollust is the principal investigator on a SHARE-funded project to measure geographic variation in ACA-related media messages and the subsequent relationship of media messages to insurance enrollment from 2013 to 2014. Her broad research interests are in the politics and ethics of health policy, and she is particularly interested in understanding the media’s role in influencing the public’s opinions and perceptions of health policy issues. Learn more.
Fertig, A. August 4, 2015. "The First Insurance Claim of New ACA Enrollees." Presentation. Minneapolis, MN: Medica Research Institute Seminar.
Gross, T. July 2015. "Why Medicaid Expansion Makes Economic Sense." Video. New York, NY: Mailman School of Public Health, Columbia University.
Gollust, S. September 6, 2015. “Media and the Politics of Implementation: Geographic Variation in ACA Coverage,” Presentation. San Francisco, CA: 2015 Annual Meeting of the American Political Science Association (APSA).
Hirth, R. August 4, 2015. "Innovative Benefit Design for Connecticut State Employees - Findings from a V-BID Evaluation." Webinar. SHARE and the Center for Value Based Insurance Design at the University of Michigan.
Hirth, R. March 2015. "Connecticut's Health Enhancement Program for State Employees UPDATE (2015)." Issue Brief. Ann Arbor, MI: Center for Value-Based Insurance Design at the University of Michigan.
Publication
SHARE Quarterly Update: April - June 2015
SHARE Quarterly Update, April - June 2015
|
|||||||
|
|||||||
|
|||||||
Publication
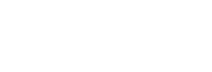
Exploring State Choices in Benefit Design for Medicaid Expansion Populations
Colin Planalp lead a lunch roundtable discussion on the topic of alternative benefit plans (ABPs) at the 2015 NASHP Annual Conference.
View a PDF of his presentation handout
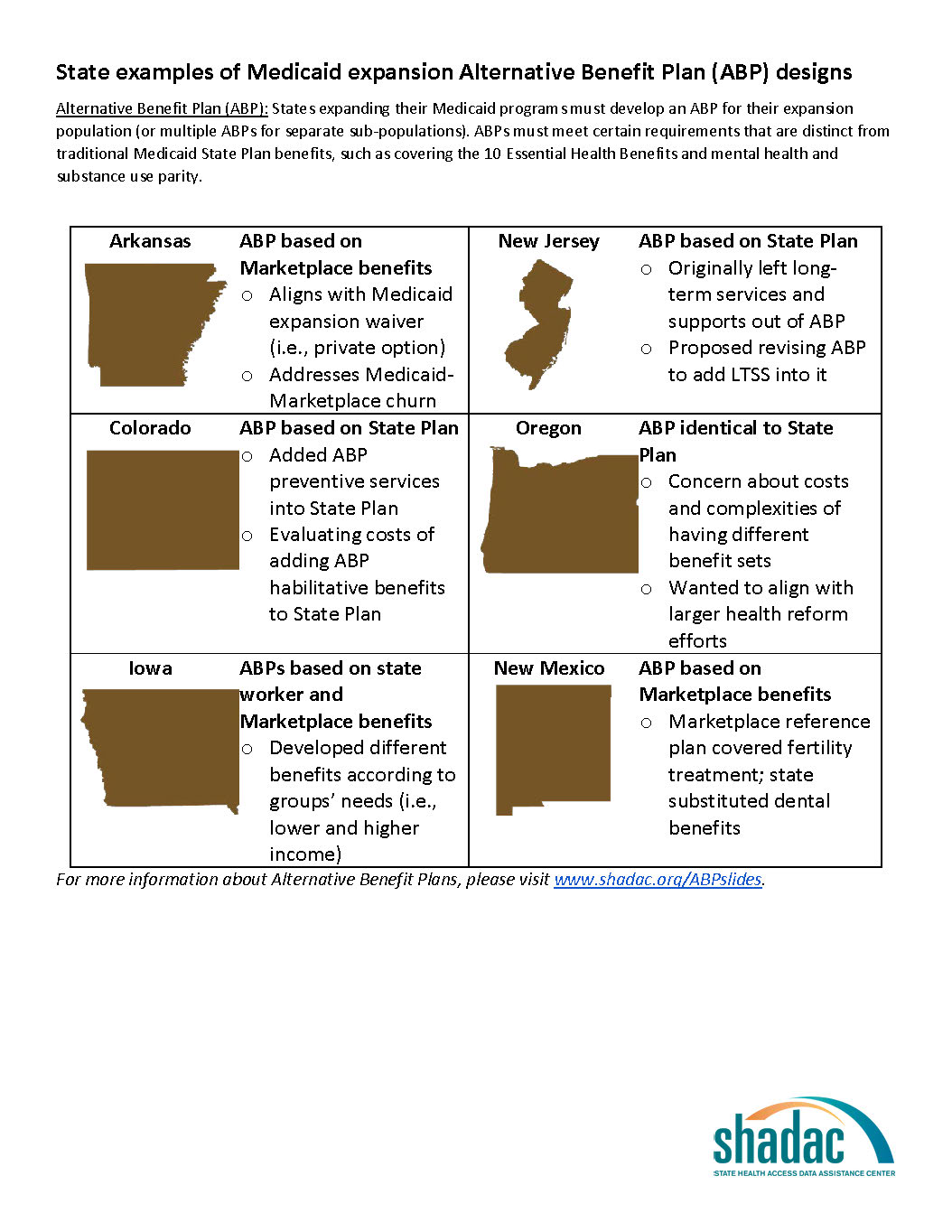
For more information about Alternative Benefit Plans, please visit www.shadac.org/ABPslides
Blog & News
SHADAC at NASHP 2015 Annual Conference
October 20, 2015:The 2015 Annual Conference of the National Academy for State Health Policy (NASHP) is currently underway in Dallas, TX. This year's conference theme is "Blazing New Trails: Innovations in State Health Policy", and a number of SHADAC staff are lending their voices to the discussion:
- Donna Spencer is discussing Medicaid expansion today (10/20) on a panel titled, "Medicaid Expansion: Staking New Ground and Corralling Cost Savings," at 1:30 p.m.
- Elizabeth Lukanen will discuss enrollment tomorrow (10/21) on a panel titled, "The Enrollment Rodeo: Who's Galloped In and Who Will Be Lassoed Next?" at 9:00 a.m.
- Colin Planalp will lead a lunch roundtable tomorrow (10/21) on the topic of alternative benefit plans (ABPs). The roundtable, "Exploring State Choices in Benefit Design for Medicaid Expansion Populations," will begin at 12:30 p.m.
Also leading a lunch roundtable tomorrow at 12:30 p.m. is Karen Brodsky of Health Management Associates, who will be discussing findings from her SHARE-funded study of provider network monitoring practices.
We will post presentation slides from SHADAC researchers to the website after the conference.