Blog & News
Tracking Health Insurance Coverage During the Unwinding: Monthly Data from the Household Pulse Survey
Originally posted on July 24, 2023 - Last updated on October 4, 2024:This update was posted on October 4, 2024 and uses data from the October 2024 release of the Household Pulse Survey, collected August 20 - September 16, 2024.
Important Note: This will be the final data release from the Household Pulse Survey, and the final update of this SHADAC product. Moving forward, the U.S. Census Bureau will be launching a similar study with a longitudinal design called the Household Trends and Outlook Pulse Survey (HTOPS) in January 2025. You can read more about this study here.
Introduction
The unwinding of the Medicaid continuous coverage requirement represents the largest nationwide coverage transition since the Affordable Care Act. Since February 2020, enrollment in Medicaid and the Children’s Health Insurance Program (CHIP) has increased by 23 million enrollees and analysis indicates that as many as 15 million individuals will exit Medicaid to other coverage or become uninsured. This blog uses data from the U.S. Census Bureau’s Household Pulse Survey (HPS) to track trends in adult health insurance coverage rates as states “unwind” the Medicaid continuous coverage requirement and restart standard redetermination procedures.
Given the intense interest from policymakers and the media in monitoring coverage transitions during the unwinding, many states have released Medicaid administrative data showing their progress, with some State-based Marketplaces also reporting transition data. Though administrative data can show the number of successful Medicaid renewals and coverage terminations along with transitions to Marketplace coverage, they cannot provide information on transitions to other sources of coverage, such as employer-sponsored insurance or provide an estimate of changing rates of uninsured individuals.
As states continue the process of redetermining beneficiaries’ Medicaid eligibility, this resource will help track transitions in coverage. Specifically, it will present rates of primary source of health insurance coverage by type (Employer/Military, Direct Purchase, Medicaid/CHIP) and rates of no insurance as they are observed in the HPS. Estimates will be presented at the state and national level by selected individual and geographic characteristics. The survey does not include children, so the analysis is limited to adults 18 and older.
This blog will be updated on a monthly basis as new HPS data are released and compare the latest monthly coverage estimates (reference above in the subtitle) to estimates from March 2023, the last month before the unwinding began.
Highlighted Findings
Limited to statistically significant changes at the 95% confidence level.
- Compared to March 2023, ESI/Military coverage fell 1.6 percentage points (PP) to 52.1% among all adults in September. This decrease was reflected across several groups:
- Adults age 65 or older (2.4PP)
- White, non-Hispanic adults (2.1PP)
- Adults living in Medicaid expansion states (1.7PP)
- The uninsurance rate overall did not change significantly. While uninsurance rates among adults age 65 or older fell 1.1PP, significant increases were seen in the following groups:
- Adults age 18 - 64 (1.2PP)
- White, non-Hispanic adults (1.1PP)
- Adults with prior year household incomes of $50,000 - $74,999.
- Rates of any Medicaid fell 4.2PP among adults with prior year household incomes of $50,000 - $74,999. Rates among all adults held steady at 18.0%.
- The rate of Direct Purchase coverage increased in adults with prior year household incomes of $50,000 - $74,999.
- There were few meaningful changes in rates of Medicaid/CHIP as a primary source of coverage.
Select a coverage type from the orange box on the right in the dashboard below to filter the visualizations.
Methods and Data
This analysis uses public use microdata from the Household Pulse Survey (HPS), a monthly, nationally representative, quick-turnaround survey that collects data on topics including household demographics, education, employment, food sufficiency, financial spending, housing security, and physical and mental health, in addition to current health insurance coverage.
The survey has a typical monthly sample size of 60,000 to 80,000 U.S. adults and is designed to produce state-level (and a select number of metropolitan-level) estimates of the civilian noninstitutionalized adult population. The survey does not include children (those age 17 or younger).
As of January 2024, data is collected for approximately four weeks each month from adults age 18 or older via a short, online survey and is released on a monthly basis. Prior to this, data was collected for approximately two weeks each month and released on a monthly basis. Readers should keep in mind that the HPS emphasis on producing near-real-time data comes with the tradeoff of lower levels of data quality compared with “gold standard” surveys such as the American Community Survey (ACS).
These data quality issues include very low response rates (e.g., 6.7% response rate in the March 2023 survey), underrepresentation of harder-to-reach groups (e.g., adults with lower levels of education, young adults), a lack of editing and imputation for most variables, and likely some degree of nonresponse bias. For these reasons, HPS estimates should be treated with a greater degree of caution than estimates from other federal surveys.
Further, like other surveys, the HPS relies on respondents’ self-reporting their coverage, which is often associated with known biases such as the Medicaid Undercount and reflects respondents’ (sometimes imperfect) knowledge of their own coverage rather than the reality reflected in administrative data sources.
The HPS’ health insurance coverage measure is similar to that used in the ACS and asks respondents: “Are you currently covered by any of the following types of health insurance or health coverage plans?” Respondents are allowed to select “Yes” or “No” from among the following coverage types:
1. “Insurance through a current or former employer or union (through yourself or another family member)”;
2. “Insurance purchased directly from an insurance company, including marketplace coverage (through yourself or another family member)”;
3. “Medicare, for people 65 and older, or people with certain disabilities”;
4. “Medicaid, Medical Assistance, or any kind of government-assistance plan for those with low incomes or a disability”;
5. “TRICARE or other military health care”;
6. “VA (including those who have ever used or enrolled for VA health care)”;
7. “Indian Health Service”; or
8. “Other”
The response options for employer coverage [1], TRICARE [5], and VA [6] were combined into one Employer/Military coverage category, and respondents were considered uninsured if they didn’t affirmatively report any coverage under options 1-6.
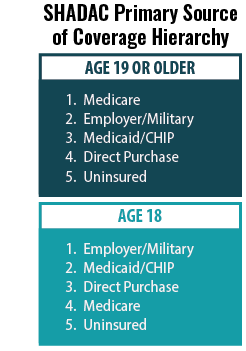 SHADAC’s primary source of coverage hierarchy was applied to determine which payer was likely primary when a respondent reported multiple sources of coverage (see SHADAC brief for more information).
SHADAC’s primary source of coverage hierarchy was applied to determine which payer was likely primary when a respondent reported multiple sources of coverage (see SHADAC brief for more information).
For example, the hierarchy would classify a respondent reporting both Medicaid/CHIP coverage and Employer/Military coverage as having Employer/Military as a primary source of coverage, as Employer coverage typically acts as the primary payer for individuals with Employer and Medicaid coverage.
Estimates with a relative standard error (standard error divided by the percentage estimate) of 30% or greater, based on an unweighted denominator count of less than 50, based on an unweighted numerator count of less than five, or with a weighted estimate of exactly 0% or 100% were considered statistically unreliable and were suppressed.
Two-sided t-tests (95% confidence level) were used to assess statistically significant differences between the most recent data month and the baseline month (i.e., March). A lack of statistically significant difference does not affirmatively establish that there was no significant difference but rather that the data presented here are not sufficient to show a significant difference.