Newly available COVID-19 vaccines promise to help protect individual Americans against infection and eventually provide population-level herd immunity. However, the rollout of the COVID-19 vaccines thus far—largely delegated to the states—has been slow and inconsistent. The initial groups prioritized for vaccination were health care workers on the front lines of the pandemic and nursing facility residents, many of whom are especially vulnerable to COVID-19 infection and severe outcomes. However, there are concerns that these prioritization decisions—in addition to evidence that lower-income individuals, people of color, and individuals without strong connections to the health care system are less likely to get vaccinated—could worsen existing pandemic-related health inequities.
Preliminary data have unfortunately reinforced these concerns, showing patterns of lower vaccination rates among people with lower incomes and levels of education, and marginalized racial and ethnic groups. The U.S. Census Bureau recently released new data on take-up of COVID-19 vaccines from the most recent wave of its Household Pulse Survey (HPS), collected January 6-18, 2021. The HPS is an ongoing, weekly tracking survey designed to measure impacts of the COVID-19 pandemic. These data are the first to provide estimates of COVID-19 vaccination rates at the state level and by subpopulation. This blog post presents top-level findings from these new data, focusing on rates of vaccination (one or more doses) among U.S. adults (age 18 and older) living in a household unit.1
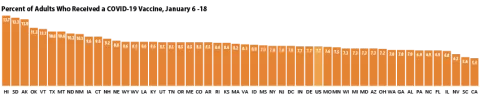
Roughly eight percent of adults had received a vaccination, but this varies by state
According to the new HPS data, 7.7% of U.S. adults had received one or more COVID-19 vaccinations during this two week period in January, though this varied by state from a low of 5.4% in California to a high of 13.7% in Hawaii. More than one in ten adults had received a vaccine in nine states: Alaska, Hawaii, Montana, New Mexico, North Dakota, Oklahoma, South Dakota, Texas, and Vermont.
Disparities in vaccination rates reflect concerns about harder-to-reach groups and groups prioritized for initial round of vaccinations
Vaccination rates also varied substantially by a number of demographic and socioeconomic factors. These could be partly a result of decisions to prioritize health care workers, who tend to be less racially and ethnically diverse than the overall population, and who often have higher incomes and levels of education.
By race and ethnicity, non-Hispanic Asian adults had the highest vaccination rates at 13.1%, followed by non-Hispanic White adults at 8.0%. Hispanic/Latino adults (any race), non-Hispanic Black adults, and non-Hispanic adults identifying with multiple races or some other race had lower vaccination rates (5.8%, 5.8%, and 6.2%, respectively). A similar pattern was seen across many states, with Asian and White adults often more likely to have received a vaccine than Black and Hispanic adults.
Large disparities in vaccination rates by income were also apparent, with the highest income groups reporting higher rates of vaccination compared to those with lower incomes, and rates increasing steadily in correlation with income. Of adults with household incomes of $100,000 or higher, 12.0% had received a COVID-19 vaccine, which was nearly 2.5x higher than the rate among those with incomes below $25,000.
Nearly half of all adults who had received a COVID-19 vaccine have incomes of at least $100,000, despite making up only three in ten adults in the overall population.
Similar patterns by income were seen across the states. For example, in 17 states, adults in the highest income category were at least 5x more likely to have been vaccinated than those in the lowest income category.
Patterns of vaccination by education were similar to those by income, with adults with less education being less likely to have received a vaccine compared to adults with more education. Nationally, 12.2% of adults with a bachelor’s degree or higher have received a vaccine compared with 3.7% of adults with less than a high school education.
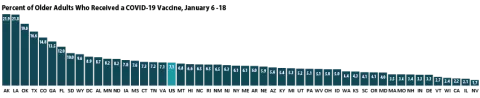
More progress is needed in vaccinating the older adult population most vulnerable to severe COVID-19 morbidity and mortality
Nationally, older adults (age 65 older) were no more likely to have received a COVID-19 vaccine than the overall adult population. During the period of January 6 through January 18, 7.1% of older adults had received a vaccine compared with 7.7% of all adults. This may be of concern because older adults are more likely to develop severe COVID-19 cases or die from the disease compared to the general population. Consequently, many states have given precedence to vaccinations for older adults, but these early data don’t show that prioritization is resulting in higher vaccination rates.
Vaccination rates for older adults ranged from 1.7% in Nevada to 21.9% in Alaska. Vaccination rates were below five percent in 15 states and were above ten percent in seven states. Older adults were more likely to have received a vaccine than the overall population in just 11 states
Notes about the Household Pulse Survey Data
Many of the estimates published by the Census Bureau and presented here were not accompanied by standard errors. Therefore, we are not able to determine if the differences we found in our analysis are statistically significant or if the estimates themselves are statistically reliable. Estimates and differences should be assumed to have large confidence intervals around them—especially for subpopulations at the state level—and caution should be taken when drawing strong conclusions from this analysis. However, the fact that patterns of inequities in other vaccination rates are mirrored by these early indications of COVID-19 vaccination inequities demonstrates reason for concern.
Though produced by the U.S. Census Bureau, the HPS is considered an “experimental” survey and does not necessarily meet the Census’s high standards for data quality and statistical reliability. For example, the survey has relatively low response rates (6.5% for January 6–18) and sampled individuals are contacted via email and text message, asking them to complete an internet-based survey. These issues in particular could be potential sources of bias, but come with the tradeoffs of increased speed and flexibility in data collection as well as lower costs. The estimates presented this post are based on responses from 68,348 adults. More information about the data and methods for the Household Pulse Survey can be found in a previous SHADAC blog post.
Related Reading
Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns (SHADAC Brief)
New Brief Examines Flu Vaccine Patterns as a Proxy for COVID – Anticipating and Addressing Coronavirus Vaccination Campaign Challenges at the National and State Level (SHADAC Blog)
Ensuring Equity: State Strategies for Monitoring COVID-19 Vaccination Rates by Race and Other Priority Populations (Expert Perspective for State Health & Value Strategies)
Upcoming SHADAC Webinar - Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns (February 4th) (SHADAC Webinar)
1 It is important to mention that the HPS does not collect data for institutionalized adults, such as those living in nursing facilities. These individuals were commonly prioritized for the first rounds of COVID-19 vaccines, so the estimates of vaccination rates presented here are likely an undercount of population-wide vaccination rates. This undercount could be more pronounced among the total 65-and-older population, as they are disproportionately likely to reside in institutions. Further, these data do not represent adults in correctional facilities such as prisons or jails—another group of adults who are also at increased risk of contracting COVID-19.