The speed and accuracy with which state Medicaid programs process applications will become increasingly important as the COVID-19 Public Health Emergency (PHE) comes to an end. Once states phase out the PHE, they will have to manage new Medicaid and Children’s Health Insurance Program (CHIP) applications at the same time they start processing the unprecedented volume of redeterminations and renewals that were on hold due to the continuous enrollment condition of the Families First Coronavirus Response Act (FFCRA). One performance indicator that provides a window into how efficiently state Medicaid programs process their Medicaid Modified Adjusted Gross Income (MAGI) and CHIP applications is Medicaid MAGI and CHIP Application Processing Times. This indicator was developed in 2013 to improve both programs through the provision and analysis of quality data. The Centers for Medicare and Medicaid Services (CMS) released its fourth update of this indicator in April 2022, which also appears as a measure of State Administrative Accountability on the Medicaid & CHIP Scorecard. In this blog, we provide an overview of the performance indicator and highlight the following themes that have emerged since the last reporting period (February – April 2021):
- Many states saw improvements in their processing times even as timeliness standards were relaxed during the PHE. Nearly 71 percent of all determinations on applications were conducted in less than 7 days.
- More than 51 percent of all determinations on applications were conducted in under 24 hours. On average, expansion states had a larger percentage of applications being processed under 24 hours than non-expansion states.
- 31 states either improved the number of applications processed within seven days, or stayed the same from 2020.
- Only 5 percent of all determinations do not meet CMS standards because they were conducted in over 45 days.
Overview of Performance Indicator and Data Quality
Every month, CMS relies on state Medicaid and CHIP agencies to collect and submit eligibility and enrollment data as part of CMS’ Performance Indicator Project. The MAGI and CHIP application processing times performance indicator provides an understanding of how many calendar days it takes between when the state agency receives an application and when it made a final eligibility determination using the MAGI standard. Determinations must be made within 45 days for new MAGI Medicaid applicants, and once the PHE ends, state agencies will have 4 months to resume timely application processing for both MAGI and non-MAGI Medicaid applications. States are not required to meet the timeliness standards for application processing due to COVID-19, which provides important context for these performance indicator findings: with increased applications and relaxed rules, many states were still able to make improvements to processing times during a time of crisis.1
The CMS provides technical assistance to ensure timely and accurate eligibility determinations – states are continuously improving their data quality for Medicaid MAGI and CHIP application times. Only three states - California, Nevada, and South Dakota - are not reporting on this indicator in 2021 (based on CMS’ specifications), which is a marked improvement from five states not reporting in 2020. However, it is important to note that this report only shows three months out of the year, and these data are constantly fluctuating based on policy changes and other factors that may or may not be state-specific.
Changes to MAGI Medicaid and CHIP Processing Times in 2021 by State
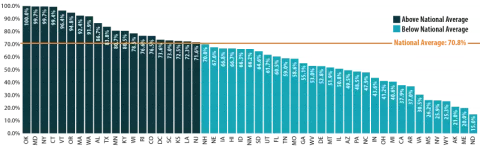
On average, close to 71 percent of applications were processed within seven days, which is well-above the CMS standard and an increase from 2020. Additionally, 19 states and the District of Columbia have processed their applications quicker than the seven day national average (see Figure 1). More than 51 percent of all determinations on applications were conducted in under 24 hours, which increased from 2020 as well.
Figure 1. Average Percent of MAGI Medicaid and CHIP Applications Processed within 7 days, States vs National, 2021
Source: SHADAC analysis of CMS Medicaid MAGI and CHIP Application Processing Times, 2021, available here: https://www.medicaid.gov/state-overviews/medicaid-modified-adjusted-gross-income-childrens-health-insurance-program-application-processing-time-report/index.html
In 2021, 31 states either improved the number of applications processed within seven days or stayed the same from 2020. (Almost the same number – although a slightly different mix – of states showed improvements in this indicator between 2019 and 2020 as well.) Oklahoma was one of two states that stayed the same (the other being Maryland) and had the highest number of applications (100%) processed; this was also achieved within 24 hours. Texas saw the greatest improvement, with a 46.7 percentage point [pp] increase. Texas’ level of improvement was followed by Iowa (43.7pp increase with 66.8 percent of applications processed within seven days in 2021), Georgia (42.6pp increase; 55.1 percent of applications processed within seven days), Missouri (41.5pp increase; 58.6 percent of applications processed within seven days), and Vermont (39.0pp increase; 96 percent of applications processed within seven days). In general, there are still nearly 5 percent of applications processed after 45 days (therefore not meeting the CMS standard) though this indicator has decreased from 2020.
On average, states that adopted the Affordable Care Act (ACA) Medicaid expansion had a larger percentage of processed applications within 24 hours than non-expansion states–an average of 40.5 percent of applications were processed within 24 hours by expansion states, compared to an average of 22.9 percent processed within 24 hours by non-expansion states. However, the average percentage of processed applications from both expansion and non-expansion states are comparable within 7 days, at 62.8 percent and 61.1 percent respectively.2
Medicaid enrollment grew significantly during the COVID-19 pandemic, driven by job and income loss as well as maintenance of eligibility (MOE) requirements. From February 2020 to April 2021, enrollment grew by 15.5 percent, and a rapid mini-survey of Medicaid directors from 44 states showed 8.9 percent enrollment growth for the 2022 fiscal year overall.3,4 However, application increases varied widely state-by-state. In general, application growth was significant, as 17 states saw an increase in applications in 2020 compared to 2019 (according to a national survey conducted by the Kaiser Family Foundation and the Georgetown University Center for Children and Families). Seven of those states reported increases higher than 10 percent.5, Of the 17 states experiencing application increases, over half saw a greater share of those applications being processed within 7 days.6 In addition, few of these states reported application backlogs.
However, there were nearly 29 percent fewer applications during the February to April 2021 reporting period compared to 2020. States that did not experience application increases could attribute this to a number of factors, including “smaller than expected declines in employer-sponsored insurance, [or] a drop in applications early in the pandemic due to office closures and the elimination of reapplications (where an individual loses coverage, often due to procedural reasons, then reapplies a short time later) due to the MOE requirements”.7
Conclusion
The CMS’ latest update on MAGI and CHIP application processing shows an overall improvement regarding processing times, despite significant increases in application volumes and the relaxation of timeliness standards during the PHE. While processing times have improved, there are still challenges with streamlined eligibility, enrollment, and renewal processes. CMS recently released a resource to remind states on best practices to process new applications, challenges to anticipate, and how to meet the requirements associated with submitting their data after the PHE. SHADAC has previously highlighted enrollment and renewal challenges that predated the pandemic as well as mitigation strategies. As we take these challenges into consideration alongside the end of the COVID-19 PHE, it will be necessary to continue monitoring this indicator for improvements and setbacks.
1 CMS. (2021, January 6). Covid-19 Frequently Asked Questions (FAQs) for State Medicaid and Children's Health Insurance Program (CHIP) Agencies. https://www.medicaid.gov/state-resource-center/downloads/covid-19-faqs.pdf
2 CMS. (2022, April 21). Medicaid MAGI and CHIP Application Processing Time Report. https://www.medicaid.gov/state-overviews/downloads/magi-application-time-report-2021.pdf
3 Williams, E. (2021, October 27). Medicaid Enrollment & Spending Growth: FY 2021 & 2022. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/medicaid-enrollment-spending-growth-fy-2021-2022/
4 Williams, E., & Hinton, E. (2022, April 4). Medicaid Spending and Enrollment: Updated for FY 2022 and Looking Ahead to FY 2023. Kaiser Family Foundation. https://www.kff.org/medicaid/issue-brief/medicaid-spending-and-enrollment-updated-for-fy-2022-and-looking-ahead-to-fy-2023/
5 Brooks, T., Gardner, A., Tolbert, J., Dolan, R., & Pham, O. Medicaid and CHIP Eligibility and Enrollment Policies as of January 2021: Findings from a 50-State Survey. Kaiser Family Foundation. https://www.kff.org/report-section/medicaid-and-chip-eligibility-and-enrollment-policies-as-of-january-2021-findings-from-a-50-state-survey-report/
6 SHADAC analysis of CMS Medicaid MAGI and CHIP Application Processing Time Report. https://www.medicaid.gov/state-overviews/downloads/magi-application-time-report-2021.pdf
7 Brooks, T., Gardner, A., Tolbert, J., Dolan, R., & Pham, O. Medicaid and CHIP Eligibility and Enrollment Policies as of January 2021: Findings from a 50-State Survey. Kaiser Family Foundation. https://www.kff.org/report-section/medicaid-and-chip-eligibility-and-enrollment-policies-as-of-january-2021-findings-from-a-50-state-survey-report/