Minnesota's Integrated Health Partnerships (IHPs) have pioneered a new approach to implementing accountable care organizations (ACOs) for the Medicaid population. Initially launched in 2013 by the Minnesota Department of Human Services (DHS), these partnerships are voluntary agreements between health provider groups and DHS. Health provider groups partner directly with DHS in multi-year contracts to both improve the quality of and reduce the total cost of care for specified patient populations using a shared savings/shared risk financing model.
When IHPs were first established in Minnesota, there were six provider groups participating. A little more than 10 years later, the number of IHPs in Minnesota has more than tripled, with 25 total partnerships covering more than 505,000 beneficiaries, as of July 2024.
DHS released the 2025 Request for Proposals (RFPs) (which recently closed) hoping to expand the program to more interested organizations and to allow current organizations to continue their partnership with the agency.
In order to better understand potential expansions and changes that may be implemented through Minnesota’s IHPs, we must first understand the foundation, function, and purpose of these partnerships.
In this blog, SHADAC staff will explore:
- What is the purpose of an Accountable Care Organization (ACO)?
- How do IHPs relate to ACOs?
- How have IHPs been established in Minnesota and how have they evolved?
- How can IHPs advance health equity for included populations?
- What are some future considerations that could help in better understanding the effect of IHPs?
Keep reading to start learning about the IHP program and how it impacts communities in Minnesota.
ACOs in Medicaid
Accountable Care Organizations (ACOs) are groups of health care providers that agree to take financial responsibility for the quality and cost of care they deliver to a defined patient population. There are national, state, and regional ACO models, and they may support multiple insured populations, i.e., Medicare, Medicaid, commercial, and self-insured.
ACOs often operate alongside Managed Care Organizations (MCOs), offering additional avenues for health care reform and focusing increasingly on advancing health equity. ACOs are a pivotal tool in promoting access to care, investing in population health, and addressing social determinants of health that affect health equity.
Since the enactment of the Affordable Care Act (ACA) in 2010, the Center for Medicare and Medicaid Innovation (CMMI) has supported state initiatives like Minnesota's State Innovation Model (SIM) to test and expand ACO models within Medicaid, and Medicaid-specific ACOs have now been established in nearly a dozen states.*
These programs vary by state in terms of delivery system reform, payment expectations, and in the authorities needed to administer them, but all such Medicaid ACO alternative payment models (APMs) are standardized through classification under Categories 2, 3, and 4 of the Health Care Payment – Learning Access Network (HCP-LAN) APM framework.
IHPs are Minnesota’s Medicaid ACO model. In 2008, the Health Reform Law of Minnesota included recommendations for statewide quality reporting, payments for coordinated care services provided in health care homes (HCHs), and encouragement to participate in bundled payment demonstrations. The law was then amended in 2011 to require DHS to develop a program to “test alternative and innovative health care delivery systems, including ACOs that provide services to a specified patient population for an agreed-upon total cost of care or risk/gain sharing payment arrangement”, leading to the creation of IHPs.
In 2017, SHADAC had the opportunity to conduct an evaluation of early Minnesota IHP implementation as part of Minnesota’s SIM cooperative agreement with CMMI, which documented IHP expansion and evolution, helpful data analytics, and importance of ongoing monitoring of the effects of the IHP program on health care utilization, cost, and quality.
Minnesota's Integrated Health Partnerships Today
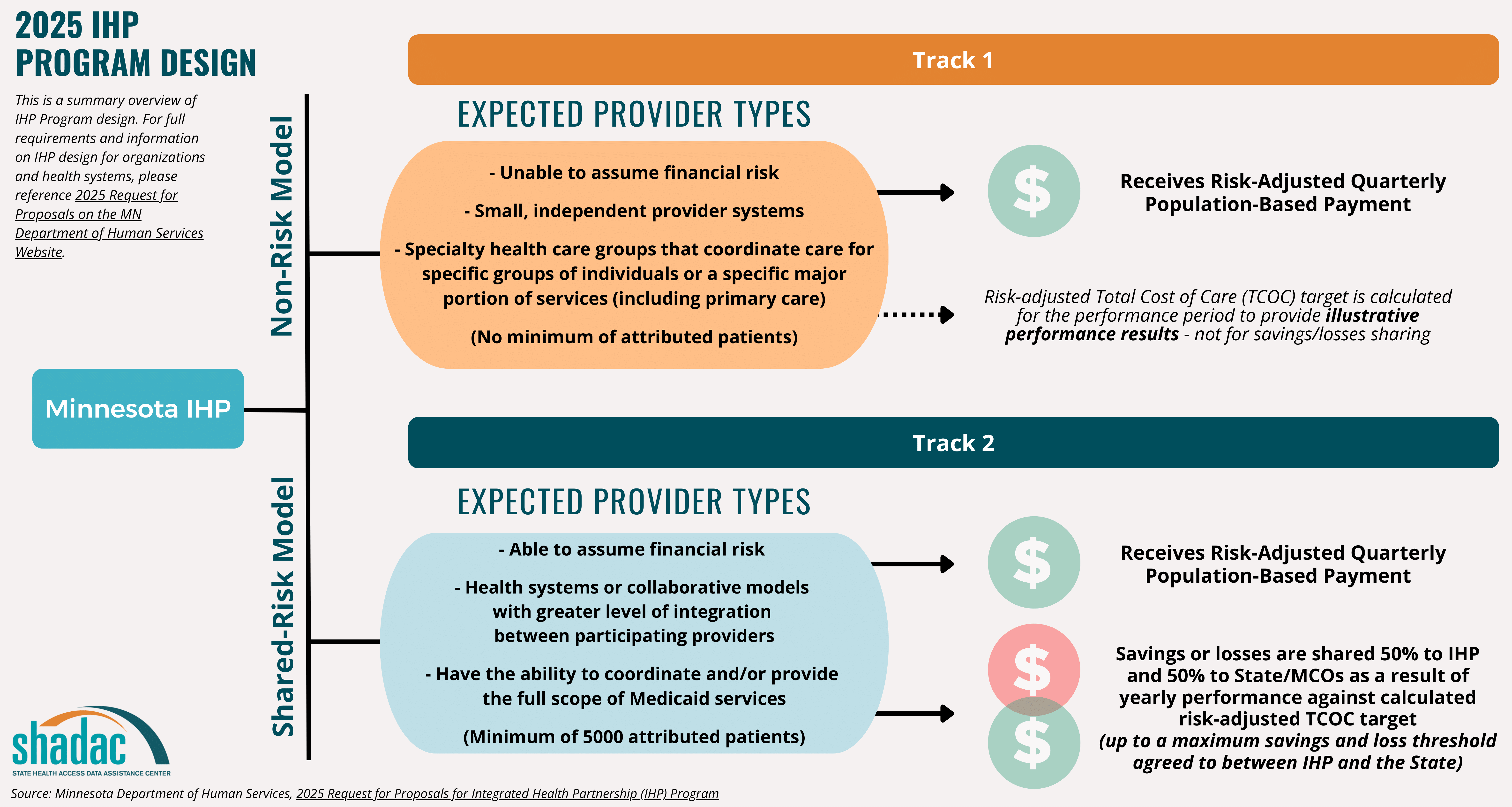
As noted earlier, Minnesota’s IHP program began over 10 years ago in 2013. In 2018, the program was updated with various enhancements and changes in order to place a stronger focus and effort on health equity, enhance the risk arrangement incentives, and provide a population-based payment. This led to the implementation of a new overall IHP model (Integrated Health Partnerships 2.0) with two possible tracks for Minnesota IHPs to operate under (see figure below). These two distinct organizational design tracks are tailored to both provider capabilities and population needs.
For full details and requirement on IHP design tracks, please reference the Minnesota Department of Human Services 2025 Request for Proposals for IHP Program
On top of improving care quality and reducing the total cost of care, IHPs on both tracks are also required to design interventions that address specific health disparities across their target population. IHPs in both tracks receive a quarterly risk-adjusted population-based payment (PBP) which is intended to contribute to care coordination and other investments for the population served. IHPs are also assessed based on quality, utilization, and health equity measures. This population-based payment is flexible, adjusting to reflect changing numbers of the included population specified by the IHP’s intervention plan, as well as changing risk factors due to medical and social complexities in the population makeup.**
IHPs are measured through quality and data metrics (e.g., comparing percent change between performance years), as well as a calculation of standards across five domains for those in the shared-risk model - Quality Core Set, Care for Children and Adolescents, Quality Improvement, Closing Gaps, and Equitable Care - a process which is described in further detail in the following section.
Ultimately, IHPs have proven quite successful in Minnesota, with significant savings and quality improvements. Since their inception, IHPs have yielded nearly $546 million in total savings through 2022.
Emphasis on Advancing Health Equity
In response to evolving health care needs and feedback suggesting that the timing was right to build on prior successes of the original IHP program, DHS introduced an improved program, IHP 2.0, enhancing its focus on health equity. The IHP 2.0 program, included modifications to allow the program to more directly address social determinants of health (SDOH) and incentivize partners to reduce racial, geographical, and/or other disparities.
The Minnesota Department of Health describes health equity as “addressing health disparities as part of a broad spectrum of public investments in housing, transportation, education, economic opportunity and criminal justice.” By implementing changes and integrating health equity goals into core operational frameworks, the hope with the IHP 2.0 program is to overcome the limitations of traditional health care approaches in addressing SDOH and health disparities that arise as a result.
In fact, recent case studies on Medicaid payment reforms conducted by the Urban Institute directly referenced and cited Minnesota’s IHPs, describing their influence on health equity along with the overall changes made to the program in 2018 in order to continue to advance equity in Medicaid.
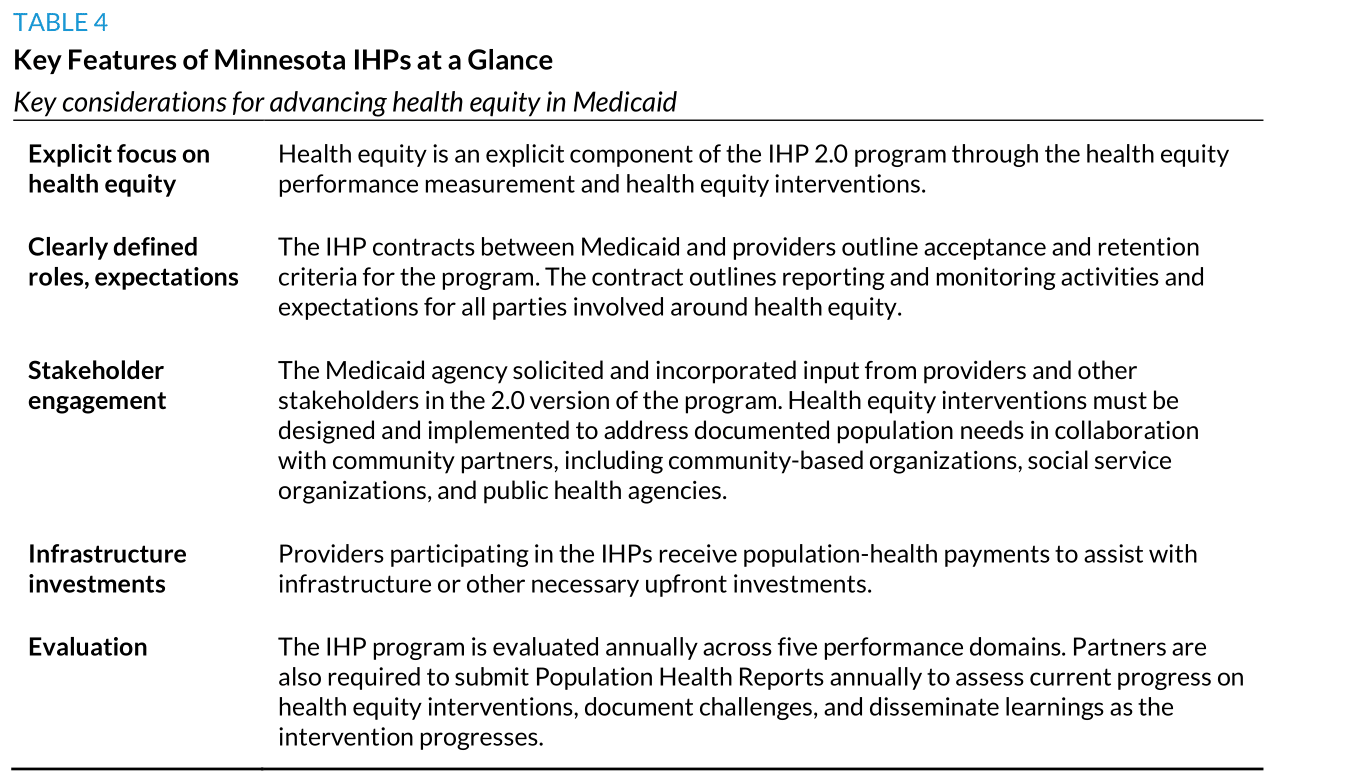
The table below from the Urban Institute identifies and describes the core features of the IHP 2.0 program designed to both focus on and advance equity for beneficiaries.
Source: Allen & Willis, “Can Medicaid Payment and Purchasing Strategies Advance Health Equity?” The Urban Institute, December 2023, https://www.urban.org/sites/default/files/2023-12/Can%20Medicaid%20Payment%20and%20Purchasing%20Strategies%20Advance%20Health%20Equity_0.pdf
As described above, the success of IHPs is evaluated based on performance in health care quality, utilization, health equity, and total cost of care (TCOC). When monitoring quality for those in risk arrangements where quality has an impact on shared savings and losses, the quality-related assessments are organized into five domains.
As a reminder, those domains are as follows:
- Quality Core Set
- Care for Children and Adolescents
- Quality Improvement
- Closing Gaps
- Equitable Care
Two of these domains, “Closing Gaps” and “Equitable Care,” specifically target health equity through tailored clinical and utilization measures aimed at reducing and eliminating disparities among specific Medicaid populations. IHPs can also receive ‘bonus points’ on their overall quality score for creating additional initiatives under the Quality Improvement, Closing Gaps, and Equitable Care domains.
Recent Health Equity Interventions
As a part of the enhanced focus on health equity, IHPs are encouraged to design interventions to address targeted populations’ health equity challenges.
Target populations may differ among the IHPs, with some initiatives aimed at supporting the entire IHP patient population and some designed to serve a more specific sub-population. A summary list of common target populations of Minnesota’s 25 IHPs include:
- Children, adolescents, families, and new mothers
- Justice-involved individuals
- Patients with a mental illness or individuals living with a family member with a mental illness
- Patients that are food insecure
- Adults with substance use disorder
- Individuals experiencing challenges accessing care, including Black, Indigenous, and people of color
A summary list of common social risk factors across Minnesota’s 25 IHPs include:
- Housing instability
- Food insecurity
- Social isolation
- Transportation
- Difficulty paying bills
- Education
- Employment
- Mental health needs
- Access to care
- Language barriers
- Income
- Childcare
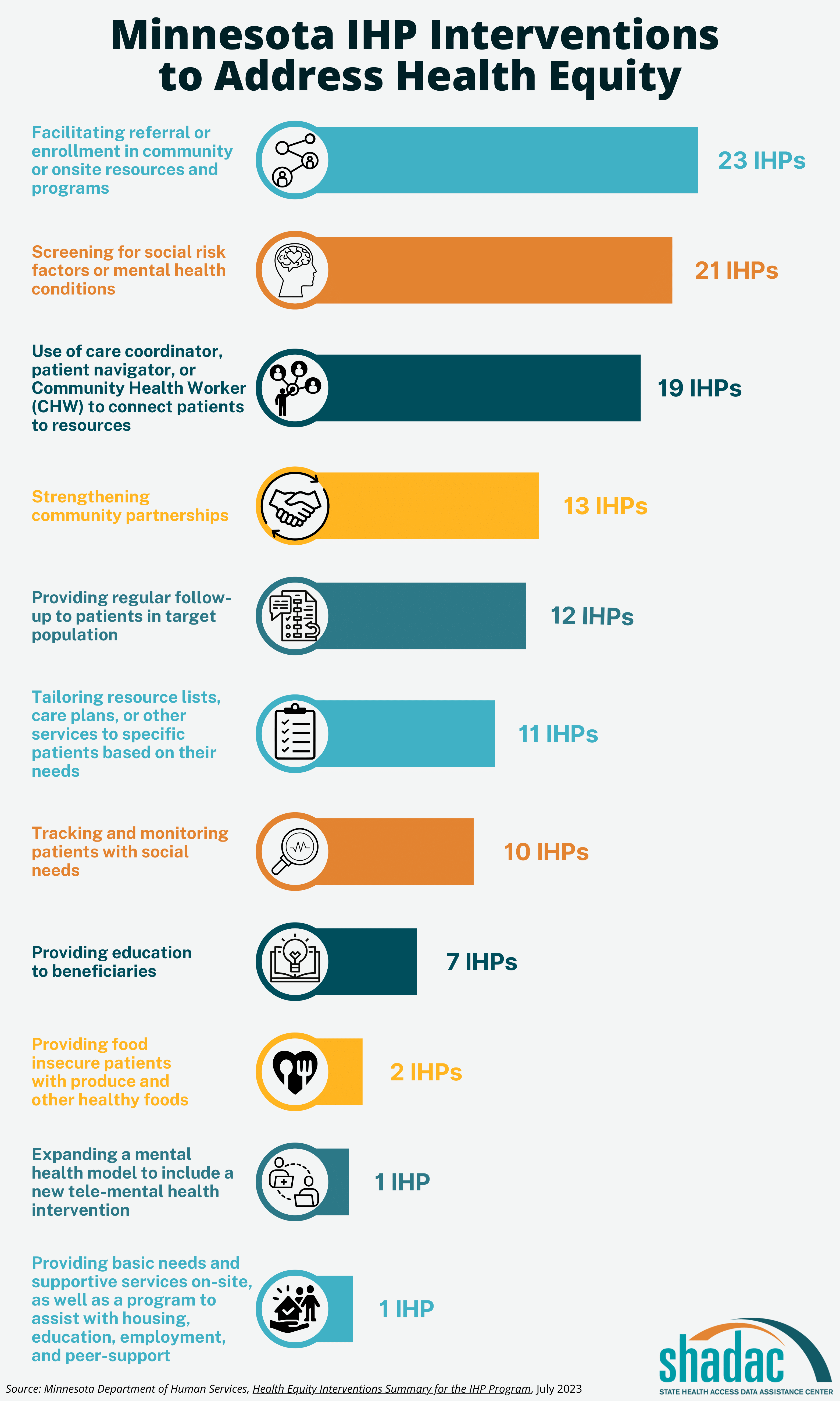
IHPs must first identify the population or populations that they are serving, and then they must design, develop, and implement targeted intervention efforts based on those populations, risk factors, and SDOH to advance equity for those groups. IHPs are encouraged to identify an intervention that will meet the needs of their specific population given their knowledge of their community. Examples of these efforts include community partnerships, screening initiatives, referrals to community resources or other needed programs, and care coordination for social needs. The following is a summary list of common interventions currently being used to address health equity across Minnesota’s 25 IHPs:
For a full list, the Health Equity Interventions Summary at this link provides the specific target population, social risk factors, interventions, and milestone components for each IHP in Minnesota.
Closing Thoughts
As DHS’ IHP Program continues to evolve, its focus on data analytics and population health management remains pivotal for achieving comprehensive care delivery and advancing health equity statewide. The IHP 2.0 Program exhibits the importance of translating equity-focused policy goals into actionable requirements and programs. DHS’ work to monitor and disseminate the outcomes of the health equity initiatives and interventions implemented by IHPs will continue to provide valuable insights into their effectiveness and impact on Minnesota's health care landscape.
One potential dissemination method would be to make the Population Health Reports from IHPs publicly available. This would not only increase transparency around the data collected by IHPs and the lessons learned from putting interventions into practice, but also aid in our understanding of the effectiveness of IHPs in addressing SDOH, improving access to care, and eliminating health disparities.
Continue learning about health equity in Medicaid and beyond with the following SHADAC products: