Newly available COVID-19 vaccines promise to help protect individual Americans against infection and eventually provide population-level herd immunity. The pace of the COVID-19 vaccination rollout in the United States has been somewhat erratic—with reports of slow early going before picking up somewhat in following weeks, only to be hampered by recent storms across the southern region. However, signs of vaccination progress are appearing on the horizon once again, with manufacturers ramping up production, shipping getting back on track after the recent roadblocks, and early positive news from the FDA regarding Johnson & Johnson’s single-shot vaccine. The initial groups prioritized for vaccination were health care workers on the front lines of the pandemic and nursing facility residents, many of whom are especially vulnerable to COVID-19 infection and severe outcomes.
While these groups continue to hold priority in vaccination slots, many states have expanded vaccine access to other (still high-priority) segments of the general population such as older adults, K-12 and child care workers, essential workers, and those with high-risk medical conditions. However, there are concerns that these prioritization decisions and the existing mechanisms of the vaccine rollout—in addition to evidence that lower-income individuals, people of color, and individuals without strong connections to the health care system are less likely to get vaccinated—are inadequate to narrow the clear disparities in the vaccine rollout so far and could worsen existing pandemic-related health inequities.
The available data have not assuaged these concerns, and show patterns of lower vaccination rates among people with lower incomes and levels of education, and marginalized racial and ethnic groups. The U.S. Census Bureau recently released updated data on take-up of COVID-19 vaccines from the most recent wave of its Household Pulse Survey (HPS), collected February 3-15, 2021.1 The HPS is an ongoing, weekly tracking survey designed to measure impacts of the COVID-19 pandemic. These data provide an updated snapshot of COVID-19 vaccination rates and are the only data source to do so at the state level by subpopulation. This blog post presents top-level findings from these new data, focusing on rates of vaccination (one or more doses) among U.S. adults (age 18 and older) living in households and comparing to results from the most recent wave of the HPS, collected January 20-February 1, 2021.2
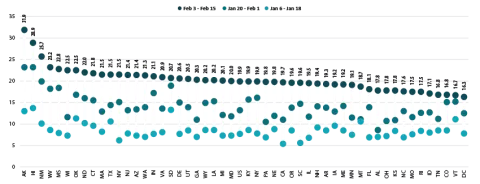
Nearly one in five adults had received a vaccination, but this varied by state
According to the new HPS data, 19.9% of U.S. adults had received one or more COVID-19 vaccinations during this two-week period in the first half of February, though this varied by state from a low of 16.3% in the District of Columbia (D.C.) to a high of 31.9% in Alaska. More than one in four adults had received a vaccine in three states: Alaska, Hawaii, and New Mexico.
Vaccination rates increased substantially across nearly all states; states with lower rates catching up
Nationally, adult vaccination rates were up from the previous wave of the HPS, increasing from 13.2% during January 20-February 1, 2021, to 19.9% during February 3-15, 2021. Most states also experienced increases in their vaccination rates, though again the size of these increases varied across the states, from an increase of 1.5 percentage points (PP) in Vermont to an increase of 10.9 PP in Wisconsin.
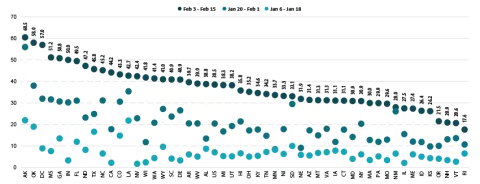
Percent of Adults Who Had Received a COVID-19 Vaccine
States that had previously had below-average vaccination rates caught up somewhat to the higher-performing states. The states that were below the national average in late January, such as California and Wisconsin, saw larger increases in their vaccination rates compared with the states that were above the national average in late January, so that by the middle of February, vaccination rates were somewhat more even across the states, with most states hovering just above or below 20% of their adult populations vaccinated.
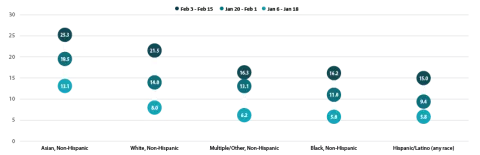
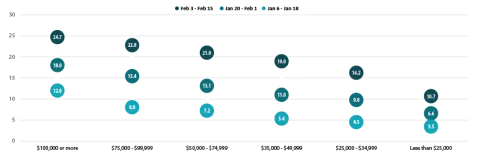
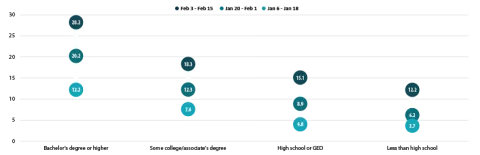
Disparities in vaccination rates remain largely unchanged
COVID vaccination rates continued to vary to a great degree by demographic and socioeconomic factors, though disparities narrowed slightly from previous weeks. This narrowing could be due to the expansion of priority groups to include a broader share of the population over this period; however, progress has remained limited in getting vaccines to certain groups such as low-income, Hispanic, and Black adults, for instance, and new vaccination strategies may be needed to reach the hardest-to-reach groups such as these.
By race and ethnicity, non-Hispanic Asian and non-Hispanic White adults continued to have above-average vaccination rates at 25.3% and 21.5%, respectively. Vaccination rates among non-Hispanic adults identifying with “Multiple” races or “Some other” race, which had previously increased relative to the average, fell behind pace and rose to just 16.3%, below the national average of 19.9%. Rates among non-Hispanic Black adults (16.2%) and Hispanic/Latino adults of any race (15.0%) remained below the national average.
Percent of Adults Who Had Received a COVID-19 Vaccine by Race/Ethnicity
Disparities in vaccination rates by income continued to narrow, though rates among those with the lowest incomes remained far below the average. Adults with household incomes of less than $25,000 were nearly half as likely to have received a vaccine compared with all adults (10.7% vs. 19.9%). This gap was largely unchanged from previous weeks, even as the gap between other lower-income groups and the average steadily narrowed from early January.
Percent of Adults Who Had Received a COVID-19 Vaccine by Income
Disparities by level of education remained, with adults holding a bachelor’s degree or higher continued to have the highest vaccination rate at 28.2%, and adults without a high school diploma having the lowest vaccination rates at 12.2%. However, disparities by education did narrow somewhat, and vaccination rates among both adults with a high school diploma or equivalent and adults with less than a high school education increased faster than the overall adult rate.
Percent of Adults Who Had Received a COVID-19 Vaccine by Education
Nearly 2 in 5 older adults received a COVID vaccine as the U.S., and many states, continued to make large progress in vaccinating older adults
Nationally, 38.5% of older adults (age 65 and older) had received at least one dose of the COVID-19 vaccine, which was 18.6 percentage points higher than the rate among all adults (19.9%). Vaccination rates for older adults ranged from 17.6% in Rhode Island to 60.5% in Alaska. Older adult vaccination rates were below 25% in four states (New Hampshire, Oregon, Rhode Island, and Vermont) and at or above 50% in five states (Alaska, Georgia, Indiana, Mississippi, and Oklahoma) and in D.C.
Percent of Adults Age 65+ Who Had Received a COVID-19 Vaccine
As in the previous period, states continued to make large progress in rates of vaccination among older adults. Compared to the end of January, 19 states more than doubled their 65+ vaccination rates, and three states (Minnesota, Wisconsin, and Nebraska) more than tripled their 65+ vaccination rates, with Minnesota nearly quadrupling its rate (from 8.5% to 33.7%). Only a handful of states failed to make substantial progress in increasing vaccination rates among older adults.
Notes about the Household Pulse Survey Data
The estimated rates presented in this post were calculated from the count estimates published by the Census Bureau. Though these counts are accompanied by standard errors, standard errors are not able to be accurately calculated for rate estimates. Therefore, we are not able to determine if the differences we found in our analysis are statistically significant or if the estimates themselves are statistically reliable. Estimates and differences for subpopulations at the state level should be assumed to have large confidence intervals around them and caution should be taken when drawing strong conclusions from this analysis. However, the fact that patterns of inequities in other vaccination rates are mirrored by these early indications of COVID-19 vaccination inequities demonstrates reason for concern.
Though produced by the U.S. Census Bureau, the HPS is considered an “experimental” survey and does not necessarily meet the Census’s high standards for data quality and statistical reliability. For example, the survey has relatively low response rates (7.3% for February 3-15), and sampled individuals are contacted via email and text message, asking them to complete an internet-based survey. These issues in particular could be potential sources of bias, but come with the tradeoffs of increased speed and flexibility in data collection as well as lower costs. A future post will investigate differences between COVID vaccination rates estimated from survey data (such as the HPS) and administrative sources. The estimates presented this post are based on responses from 77,122 adults. More information about the data and methods for the Household Pulse Survey can be found in a previous SHADAC blog post.
Previous Blogs in the Series
COVID-19 Vaccination Rates: New State-level and Subpopulation Evidence from the Household Pulse Survey (Update: Jan 10 to Feb 1)
COVID-19 Vaccination Rates: New State-level and Subpopulation Evidence from the Household Pulse Survey (Jan 6 to Jan 18)
Related Reading
State-level Flu Vaccination Rates among Key Population Subgroups (50-state profiles) (SHADAC Infographics)
50-State Infographics: A State-level Look at Flu Vaccination Rates among Key Population Subgroups (SHADAC Blog)
Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns (SHADAC Brief)
New Brief Examines Flu Vaccine Patterns as a Proxy for COVID – Anticipating and Addressing Coronavirus Vaccination Campaign Challenges at the National and State Level (SHADAC Blog)
Ensuring Equity: State Strategies for Monitoring COVID-19 Vaccination Rates by Race and Other Priority Populations (Expert Perspective for State Health & Value Strategies)
SHADAC Webinar - Anticipating COVID-19 Vaccination Challenges through Flu Vaccination Patterns (February 4th) (SHADAC Webinar)