The following content is cross posted from California Healthcare Foundation. It was first published on May 25, 2016.
Authors: Amy Adams, California Healthcare Foundation, and Sam Patnoe, State Health Access Data Assistance Center (SHADAC)
Newly available data on the CHCF's ACA 411 tool show that state residents who bought insurance through the individual market spent significantly less on health care in 2014, year one of the Affordable Care Act (ACA), than they did the year before. The first year that ACA premium tax credits and cost-sharing subsidies were available was 2014.
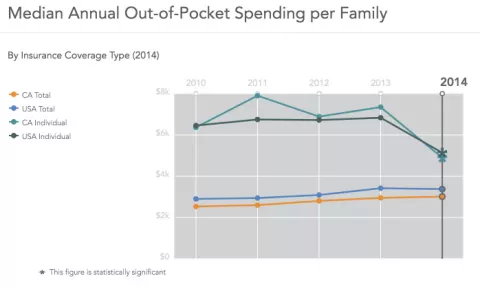
Median out-of-pocket spending for families with individual coverage dropped from $7,345 in 2013 to $4,893 in 2014 (see green line in first graph below). The percentage of Californians with individual coverage who reported a "high health care cost burden" — health care costs ate up more than 10% of household income — dropped from 42.9% in 2013 to 34.5% in 2014 (see yellow line in second graph).
While these declines in spending among those with individual coverage mirrored national trends in 2014, they were more pronounced in California. In fact, it's likely that the declines in spending for this group in California, the most populous state, helped pull down the national averages.
ACA Largely Credited with Declines in Spending for Those with Individual Coverage
Spending for those with individual coverage was likely driven down primarily by the premium tax credits and cost-sharing subsidies made available for the first time in 2014 through Covered California, the state's ACA health insurance marketplace. In 2014, 2.2 million Californians had individual health coverage — and 51% of them purchased it through Covered California. Ninety percent of Covered California enrollees were eligible for premium tax credits (valued on average at $436 a month); over half were eligible for additional cost-sharing subsidies (worth on average $100 a month) to defray the cost of deductibles and copays.
Looking across all coverage types (including Medi-Cal, Medicare, employer/military, and uninsured), changes in spending varied in 2014 — and were far less dramatic. Improvements were also seen for those on Medicare: the percentage of beneficiaries reporting a high health care cost burden dropped from 28.4% to 23.9%, and out-of-pocket spending declined by $476. However, out-of-pocket spending increased by approximately $200 for those with employer/military coverage. There were no statistically significant changes in high health care cost burden or in out-of-pocket spending for those on Medi-Cal or the uninsured. It will be important to continue monitoring these data in the coming years.
More Work Needed to Improve Affordability
Data newly available on ACA 411 shows that striking progress was made in the ACA's first year to reduce the burden of health care costs for those with individual coverage. Yet even with the substantial declines in their spending, more than one in three with individual coverage still spent more than 10% of their income on health care. Cost was the top reasonreported by California's uninsured for not obtaining coverage in 2014.
CHCF is studying cost barriers to low-income consumers' ability to purchase, maintain, and use health coverage in order to inform policy solutions. This includes an analysis of how high local cost of living impacts Californians' ability to afford health insurance. The county-by-county analysis, performed by the UC Berkeley Center for Labor Research and Education, will be released in the coming weeks.
Stay tuned for ongoing updates to ACA 411. Share your thoughts on this latest affordability data on social media using #ACA411.