.
The following content is cross-posted from State Health & Value Strategies.
Authors: Emily Zylla and Elizabeth Lukanen, SHADAC
States, the federal government, advocates, and the media have all been closely tracking and monitoring the impacts of eligibility redeterminations during the unwinding of the Medicaid continuous coverage requirement. While there has been a strong focus on disenrollment data, recently, several states have also voluntarily begun reporting Medicaid reinstatement (also sometimes referred to as “re-enrollment” or “re-opening”) data. Medicaid and Children’s Health Insurance Program (CHIP) reinstatement data (especially when paired with enrollment data) allows states to tell a more complete story about what happens to individuals after they are disenrolled.
Individuals can be reinstated in Medicaid or CHIP for a variety of reasons. Recently, the Centers for Medicare & Medicaid Services (CMS) directed 29 states and Washington D.C. who self-identified as conducting ex parte renewal processes at the household level, rather than at the individual level, to reinstate coverage for at least 500,000 individuals whose coverage was terminated inappropriately.[1] Individuals may also have their coverage reinstated as a result of fair hearing cases, or as a result of re-enrolling in Medicaid or CHIP within the 90-day reconsideration period.[2]
This expert perspective reviews current state reporting of Medicaid reinstatement data and provides recommendations for the reporting of such data. To facilitate transparency, states are encouraged to report data for at least 90-days, disaggregate data by race, ethnicity, age and other population characteristics and provide additional information to contextualize reinstatement data.
States’ Reporting of Medicaid Reinstatement Data
SHADAC’s review of public unwinding data identified nine states that report some type of Medicaid reinstatement data:[3]
The federal government does not require states to report reinstatement data as part of their Monthly Unwinding Data; and, while CMS could presumably leverage Transformed Medicaid Statistical Information System (T-MSIS) data to track whether Medicaid or CHIP members who are disenrolled are later reinstated, the availability of such data is delayed. Without a standardized national approach, each of the nine states are reporting a measure with a slightly different definition. Specific differences include the population being counted within the “reinstatement” category and the timeframe being reported and tracked (Table 1).
Table 1. States Reporting Medicaid Unwinding Reinstatement Data*
| State | Reinstatement Measure Being Reported | Timeframe |
|---|---|---|
| Arizona | Count of individuals who have completed their renewal within the 90-day reconsideration period after a procedural discontinuance. | Within the 90-day reconsideration period |
| Connecticut | Status of individuals who were disenrolled for 30/60/90 days. | 30/60/90 days later |
| Kentucky | Number of individuals reinstated (no further definition provided). | Not defined |
| Massachusetts | Members who have departed and regained MassHealth benefits. | 0-3; 4-6; 7-12 months |
| New Hampshire | Number of protected individuals who closed and subsequently re-opened by the timeframe during which they returned to coverage (e.g., within 30 days of closing). | 0-30 days; 31-60 days; 61-90 days |
| New Jersey | Members [Modified Adjusted Gross Income (MAGI) and Aged, Blind, or Disabled (ABD)] who were due for renewal in June and July respectively; and who were reinstated in NJ FamilyCare. Reasons for reinstatements include responding to renewal during the 90-day reconsideration period, automatic renewal following a previous termination, or reinstatement due to a pending or finalized fair hearing case. | June & July cohorts |
| New York | Individuals who were reinstated in accordance with the CMS Household Ex Parte (administrative) Renewal Guidance. | June & July cohort reinstatements |
| Pennsylvania | Individuals whose cases were closed with Medicaid during the 12-month unwinding period and who have since had their Medicaid re-opened within four months of closing. | 4 months |
| Virginia | Number of individuals who were closed for procedural reasons who were reinstated in the first, second or third month. | 1, 2, & 3 months |
| Source: SHADAC review of states’ unwinding dashboard metrics. Note the definitions listed in the table are the definitions/wording provided by states. |
||
Variation in Reinstatement Measures
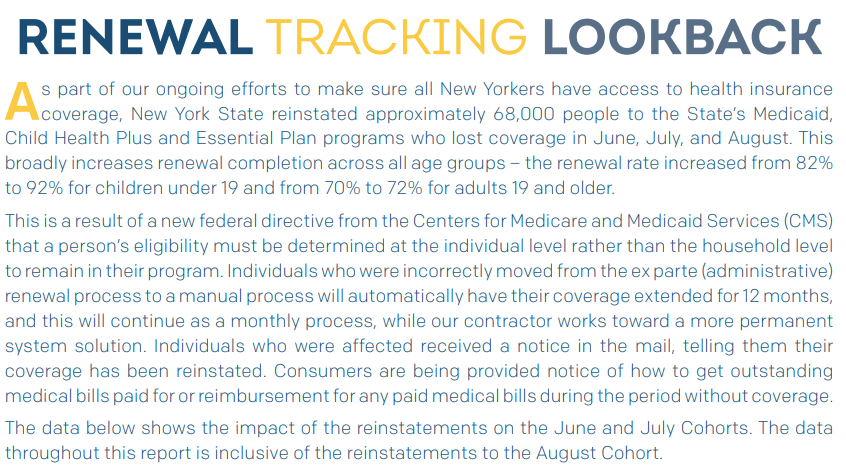
As seen above, there is wide variation in the definitions, timeframes, and amount of detail provided in the reinstatement data that states are reporting. For example, New York only reports the number of individuals reinstated in accordance with the CMS Ex Parte Renewal Guidance (Figure 1).
Figure 1. New York Medicaid Unwinding Data – Reinstatements
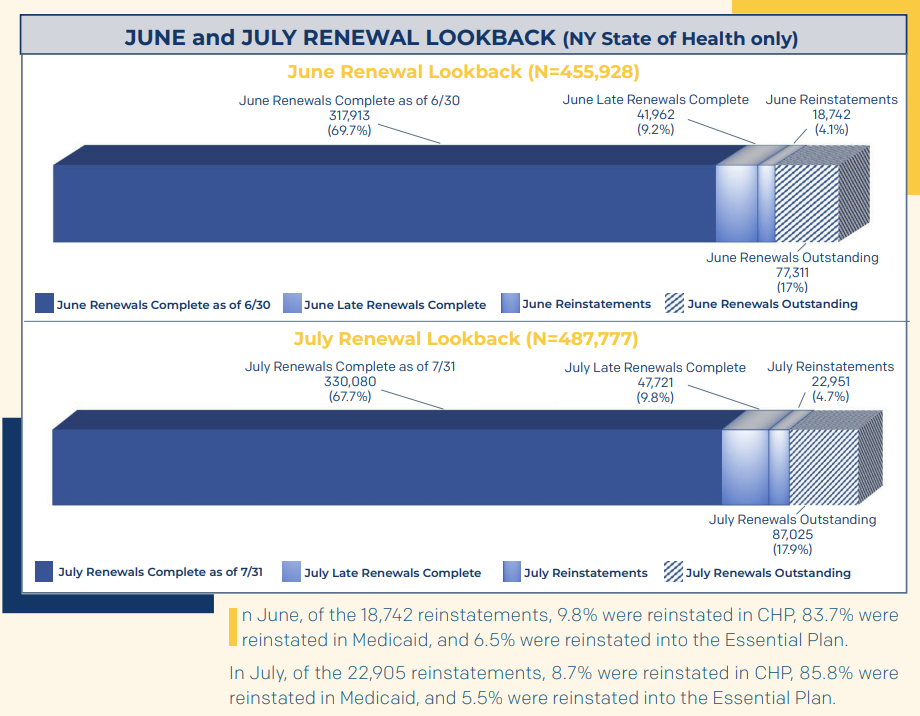
In contrast, Massachusetts reports the number of members who have departed and regained MassHealth benefits for any reason over the past 12 months (not just those reinstated due to CMS guidance) and for every month since the unwinding began (Figure 2). (Note, however, that Massachusetts does not provide a breakdown by the specific reinstatement reason.)
Figure 2. Massachusetts Unwinding Data – Re-Openings
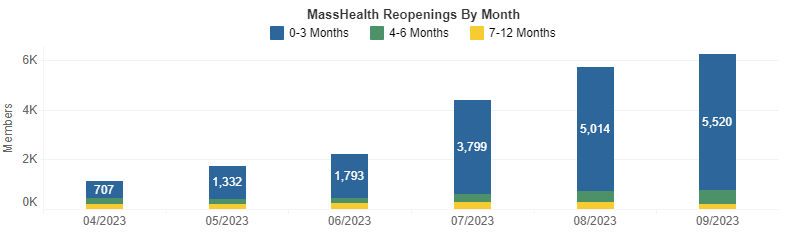
Arizona reports a cumulative total of reinstatements for those individuals who were procedurally disenrolled since the unwinding began in April (Figure 3).
Figure 3. Arizona Unwinding Data – Renewals After a Procedural Discontinuance
Best Practices for Reporting Reinstatement Data
Although it is not required, reporting Medicaid and CHIP reinstatement data publicly promotes transparency. Like the reporting of closure reason or transition outcome data (i.e., whether individuals who were disenrolled transitioned to coverage through a Marketplace plan or an employer-sponsored plan), reporting Medicaid reinstatement data (especially when paired with enrollment data) allows states to give the full picture about what happens to individuals after they are disenrolled. Being more transparent about who is coming back into Medicaid can help provide additional context about the impact of unwinding processes on populations.
Tracking and reporting Medicaid and CHIP reinstatement data over a 90-day period at a minimum is highly recommended. States that have reinstatement periods longer than 90 days can consider tracking and reporting data over both a 90-day period and the longer, state-elected period. If possible, states should also provide a breakdown of the type of reinstatements. For example, the number of individuals who were procedurally disenrolled and reinstated, the number of individuals who lost coverage due to an erroneous ex parte redetermination and were reinstated in accordance with the CMS Ex Parte Renewal Guidance, etc. While these standards are best, state reporting systems may have different functionality.
For example, some states are counting reinstatements for individuals who were terminated for procedural reasons as new applications, making those cases more difficult to track. Regardless of system capacity, states are encouraged to report at least some of the number of people who are reinstated, using whatever definition is feasible for ongoing reporting. Even limited reporting can be paired with state context to help shed light on the larger impact of unwinding.
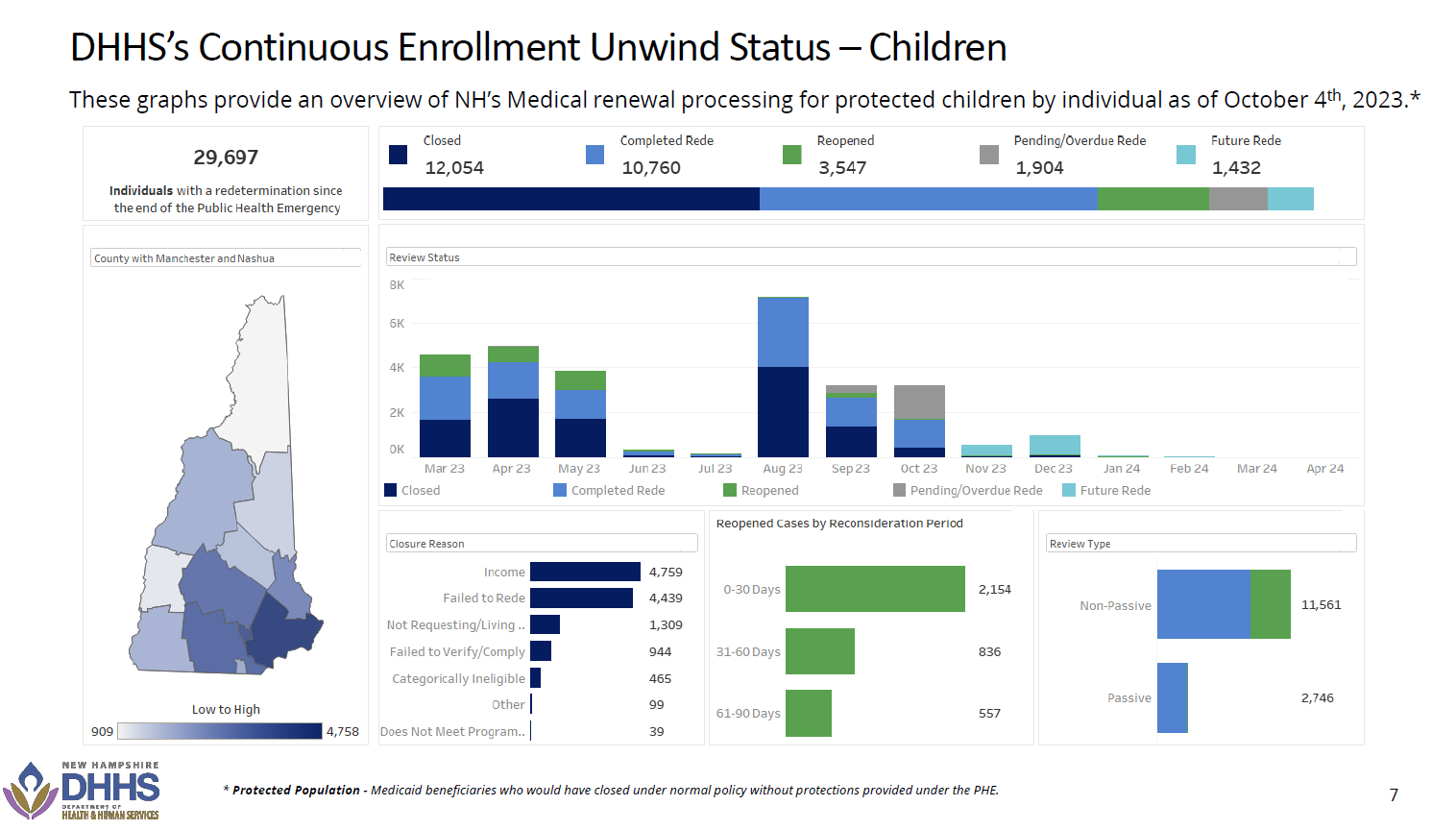
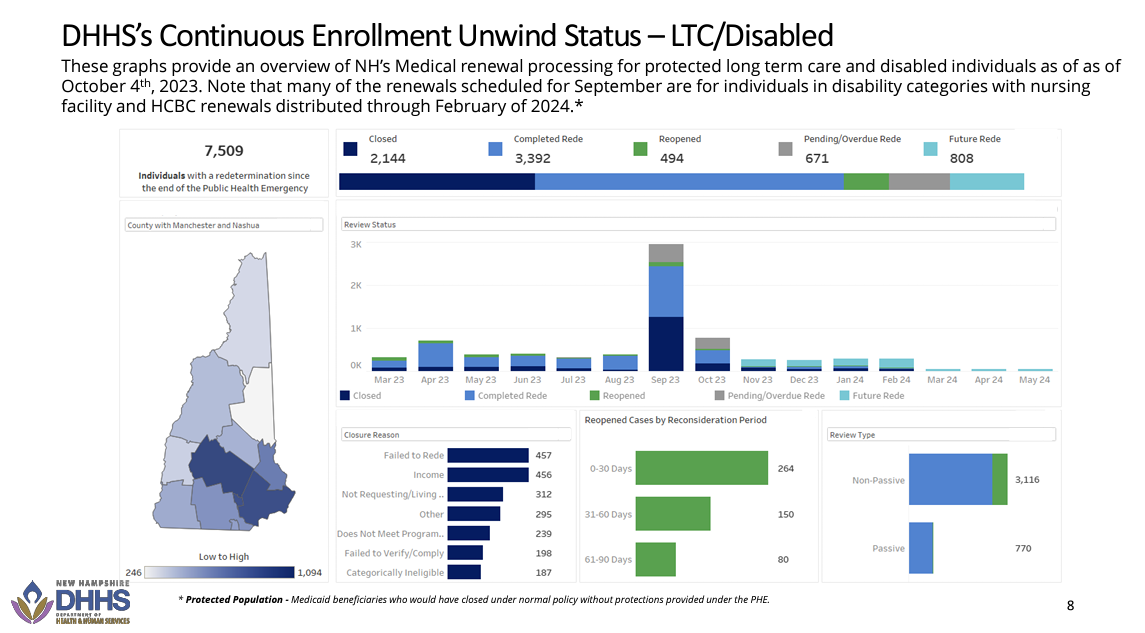
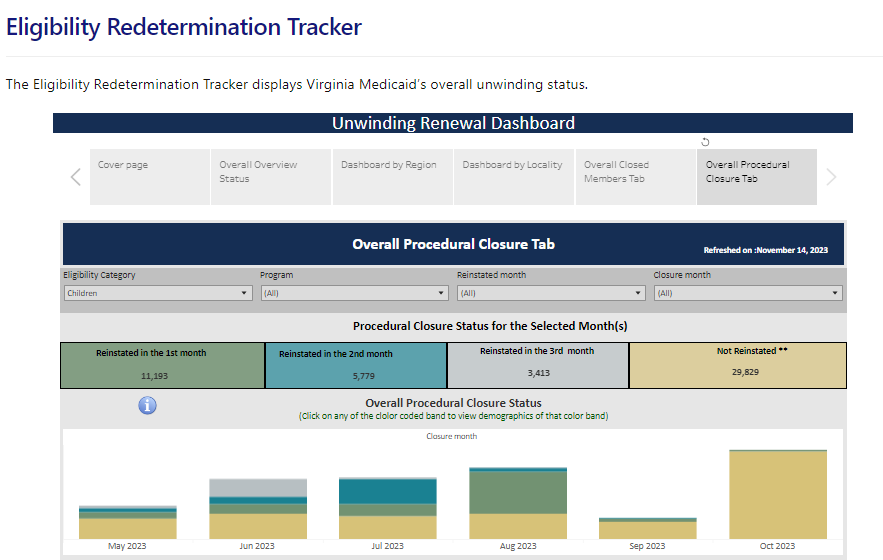
Reporting reinstatements by enrollee characteristics, such as age, race or ethnicity, or on the basis of eligibility (i.e., MAGI, CHIP, and non-MAGI if applicable) might also help provide insights into where barriers might exist, enabling states to target outreach. For example, New Hampshire reports the number of Medicaid cases that are reopened and provides breakdowns by both age (adults and children) and for individuals in long-term care (LTC) and disability categories (Figure 4). Virginia also reports reinstatements for individuals with a procedural closure that can be broken down by eligibility category (e.g., individuals who are blind or disabled, children, enrolled due to pregnancy, etc.) and by program type (i.e. fee-for-service versus managed care) (Figure 5). Connecticut provides detailed breakdowns showing where individuals who have been disenrolled have regained coverage and by what type (i.e., whether they have enrolled in a qualified health plan with advance premium tax credits, transitioned to a non-MAGI Medicaid program, or regained active Medicaid coverage) (Figure 6).
Figure 4. New Hampshire Unwinding Reopening Data – Children and Individuals who Are Disabled or in Long-Term Care
Figure 5. Virginia Eligibility Redetermination Tracker – Procedural Closure Tab
Figure 6. Connecticut Unwinding Data – Renewal Post-Disenrollment Tracking
Finally, states are strongly encouraged to include data labels, detailed definitions, and context for reinstatement data. Describe population numerators and denominators if relevant. And, if the format allows, link to information that can help contextualize the data, such as overall application or enrollment data or comparisons to a previous time period that might help a user understand the historical context of the data.
Conclusion
While Medicaid churn remains a challenge, states are working hard to maintain Medicaid enrollment for eligible individuals, and they should present data that provides a more complete picture of their efforts and impacts on coverage. Renewals and disenrollments remain important measures of successful unwinding, but there is a growing need for states to provide more information to tell the whole story. To convey a more nuanced narrative, states should provide information on CHIP and Medicaid reinstatement in whatever form is most feasible. This approach ensures that states effectively keep the public, policymakers, and advocates informed of their progress.
[1] See SHVS’ expert perspective, CMS Guidance on Conducting Eligibility Redeterminations at the Individual Level, for additional information.
[2] During the reconsideration period, states must reconsider eligibility without requiring the individual to fill out a new application if the renewal form or documentation is returned within 90 days after the date of the MAGI enrollee or CHIP enrollee’s termination. States have the option to (1) adopt a reconsideration period of longer than 90 days for MAGI enrollees, and (2) provide a 90-day (or longer) reconsideration period for individuals enrolled on a non-MAGI basis.
[3] No states reporting separate CHIP reinstatement data were identified—only New Hampshire and Virginia report reinstatement data by age.
States Reporting of Medicaid Unwinding Reinstatement Data