Health inequities are nothing new in Minnesota, but the pandemic placed them in a new light. Numerous studies have reported disparities in how COVID-19 affects many vulnerable groups, often placing them at higher risk of infection, hospitalization, and death. And the inequitable effects of the disease itself are not the only cause for alarm. Once COVID-19 vaccines received authorization, disparities in vaccination rates also became a concern, especially as surveys indicated widespread hesitancy and lagging uptake.
Partnering with the Minnesota Electronic Health Record Consortium, SHADAC delved deep into an analysis of COVID-19 vaccination rates in Minnesota. Unlike many other studies, we were able to examine not only how COVID-19 vaccination rates differed across different demographic groups, but also how those disparities developed over time. This type of analysis was possible because of the Consortium’s unique dataset, which matches data from large health care providers’ electronic health records—including detailed demographics with immunization records from the Minnesota Department of Health, ultimately covering almost all people who received a COVID-19 vaccine in the state.
Understanding the dynamics of vaccination disparities over time was a crucial element of our study. While we present data on COVID-19 vaccination rates for different demographic subpopulations at the end of 2022, we also examined the time it took to reach 50 percent of people in different demographic groups with COVID-19 vaccinations. That measure of time to vaccination is important because, in a public health crisis during which hundreds or even thousands of people were dying each day at its peak in the U.S. alone, the speed with which people were vaccinated was critical to saving lives.
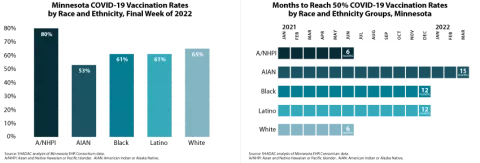
Our approach also allowed us to glean unique insights on COVID-19 vaccination disparities that are hidden below the headline numbers. For instance, although Minnesota’s Black, Latino, and White populations each had similar COVID-19 vaccination rates (61 percent, 61 percent, and 65 percent, respectively) at the end of 2022, they took distinctly different paths to reach that point. Within six months of the first COVID-19 vaccine receiving emergency use authorization, Minnesota vaccinated half of the state’s White population, but it took twice as long (12 months) for the state to vaccinate half of its Black and Latino populations.
Another crucial but under-recognized factor in COVID-19 vaccination disparities is the way public health policies placed some groups as a disadvantage in accessing vaccines in the early days of limited supply. Because experience showed that elderly people were at higher risk of severe disease and death from COVID-19, they were prioritized to be among the first people eligible for vaccines. But nationwide and in Minnesota, the White population skews older, effectively baking racial and ethnic disparities into the vaccine prioritization criteria. For that reason, we also stratified racial and ethnic groups’ COVID vaccination data by age—an approach that uncovered complex dynamics.
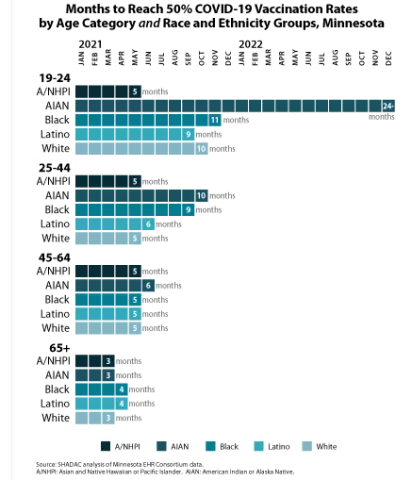
We found that disparities in COVID-19 vaccination rates were relatively small among Minnesota’s elderly population. For instance, Minnesota succeeded in vaccinating half of the elderly population across all racial and ethnic groups within three or four months—an example of how health inequities can be minimized. But disparities were stark among young adults, age 19-24. While Minnesota vaccinated half of Asian and Native Hawaiian and Pacific Islander young adults within five months, it took roughly twice as long to vaccinate half of Latino young adults (nine months), White young adults (ten months), and Black young adults (eleven months). And stunningly, Minnesota had failed to reach half of American Indian and Alaska Native young adults by the end of 2022—approximately 24 months after vaccines were first authorized.
We also examined COVID-19 vaccination rates by other demographic categories, finding higher vaccination rates and quicker vaccination progress among older population groups, urban and suburban communities, and females. Additionally, our study found disappointing rates of COVID-19 vaccination among children, particularly younger children. At the end of 2022, less than one-half of children age 5-11 had been vaccinated, despite having been eligible for vaccines for over a year; and less than one-tenth of children age six months to four years had been vaccinated, despite having been eligible for roughly six months. Despite a common, incorrect notion that COVID-19 is harmless for children, other researchers have found that COVID-19 was a top 10 cause of death for children during the pandemic, so those low vaccination rates are needlessly leaving Minnesota kids at risk.
Together, the findings from this new study highlight two main points: First, Minnesota’s COVID-19 vaccination efforts resulted in clear disparities. When looking at high-level data, it is easy to miss those disparities because some of them narrowed over time. But looking at detailed data illustrates the ways that certain groups were left vulnerable to COVID-19 for much longer than others. Second, our findings on disparities in the time Minnesota took to vaccinate half of different subpopulations demonstrate the importance of monitoring such health equity measures over time. Time is critical in an emergency such as the pandemic, and eventually closing gaps in health disparities simply isn’t good enough. Health equity requires urgency.